
by All Things Neonatal | Sep 21, 2016 | bioethics, preemie
While we draw the line at 22 5/7 weeks for offering active resuscitation where I work, what does one do when the family requests resuscitation prior to that point. While I am a clear fan of social media, one consequence of having such widely available information at our fingertips is that families may already know before you come to speak with them that were they only to have been born in another place like Montreal, the cutoff would have been lower. When faced with such demands what does one do? Well, in the case of my own experience it was to give in to the demands of the parents. While I certainly discourage such heroic attempts, what is one to say when the family having received your opinion states “I want everything done”. Informed consent is a tricky one in that if you approach a family for informed consent and they refuse to accept your desired direction of care where does that leave you? It leaves you with informed refusal and if we are being fair to our families we have to accept that informed refusal is just as important as informed consent.
Nothing New?
The truth is informed refusal has been recognized as being critically important to decisions in patient care for many years. Previous papers on the subject include a nice review by Ridley DT, Informed consent, informed refusal, informed choice–what is it that makes a patient’s medical treatment decisions informed? What this really comes down to is a patient’s right to personal autonomy and self determination. Does a parent in this case have the right to do what they want even in the face of dismal odds? Furthermore where are we placing the importance of values? Is it physician or patient centric? In the physician centric world, after we impart our experience and wisdom we expect the patient to generally follow through with what we are steering them towards in cases such as this. Informed consent of course is meant to be free of coercion but let’s face it, when we truly believe something is fairly futile are we honestly playing an impartial role or using our tone, body language and choice of words to direct families down the path that fits with our own beliefs and values? I would offer that in most cases when we seek informed consent what we are really doing is seeking to pass along the justification for what we are wanting to do and then moving forward once obtained.
What do we do though when after hearing the pros and cons the family still opts to move forward and worse yet is in disagreement with our preferred plan. Well there you arrive at informed refusal. If after hearing our best transfer of information the family still wants to proceed what does one do? As a physician if I believe something is completely futile and I find myself in this position then I am truly at fault. Seeking informed consent in this situation was completely inappropriate. One should have simply said there is nothing that can be done.
The Montreal Example
Getting back to the example that started this piece, if a family knows that there are places in Canada (or let’s be honest, if I know there are survivors in Canada at 22 weeks) that resuscitate and have survivors then it isn’t really futile is it. I know many of you would say “but the odds are so stacked against the baby” and “they don’t know what they are getting themselves into” but what does one say in this circumstance when despite your best attempts the family still wants to resuscitate?
Therein lies the challenge. If we approach this as an opportunity for informed consent we need to accept that we may find ourselves face to face with “informed refusal”. Now I need to be careful here. I am not advocating a wide open optimistic approach to resuscitation at 22 weeks. What I am suggesting though is that if you find yourself coming into a unit somewhere in the next few months and find yourselves looking at a 22 week infant don’t jump to conclusions! Did the family despite all the warnings want this? Don’t leap to the thought that the Neonatologist is pushing for this but rather it may indeed be a case of a family advocating for their child against all odds. It may not be something that we agree with in many cases but are we thinking from the perspective of the family or our own value system?

by All Things Neonatal | Jul 9, 2016 | preemie, Prematurity, Uncategorized
Preterm infants born between 22 to 25 weeks gestational age has been a topic covered in this blog before.
I think it is safe to say that this topic stirs up emotions on both sides of the argument of how aggressive to be when it comes to resuscitating some of these infants, particularly those at 22 and 23 weeks. Where I work we have drawn a line at 23 weeks for active resuscitation but there are those that would point out the challenge of creating such a hard-line when the accuracy of dating a pregnancy can be off by anywhere from 5 – 14 days. Having said that, this is what we have decided after much deliberation and before entertaining anything further it is critical to determine how well these infants are doing not just in terms of survival but also in the long run. In the next 6 months our first cohort should be coming up for their 18 month follow ups so this will be an informative time for sure.
Do Days Matter?
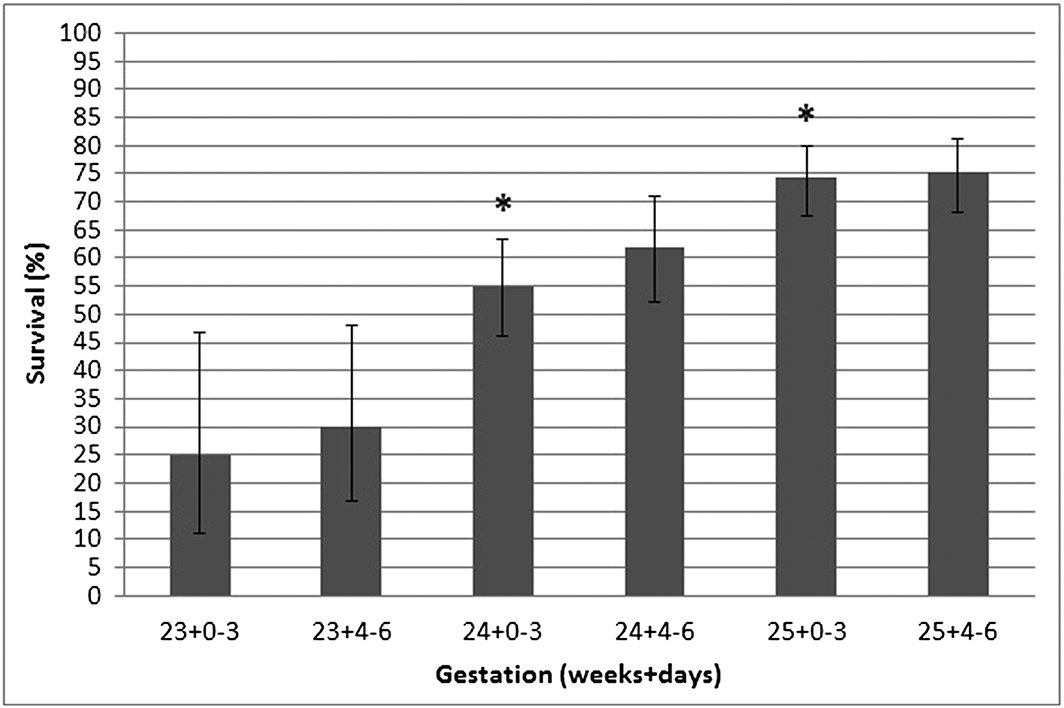
This is the subject of a short report out of Australia by Schindler T et al. In this communication they looked at the survival alone for preterm infants in a larger study but broke them down into 3 and four-day periods from 23 to 25 weeks as shown below.
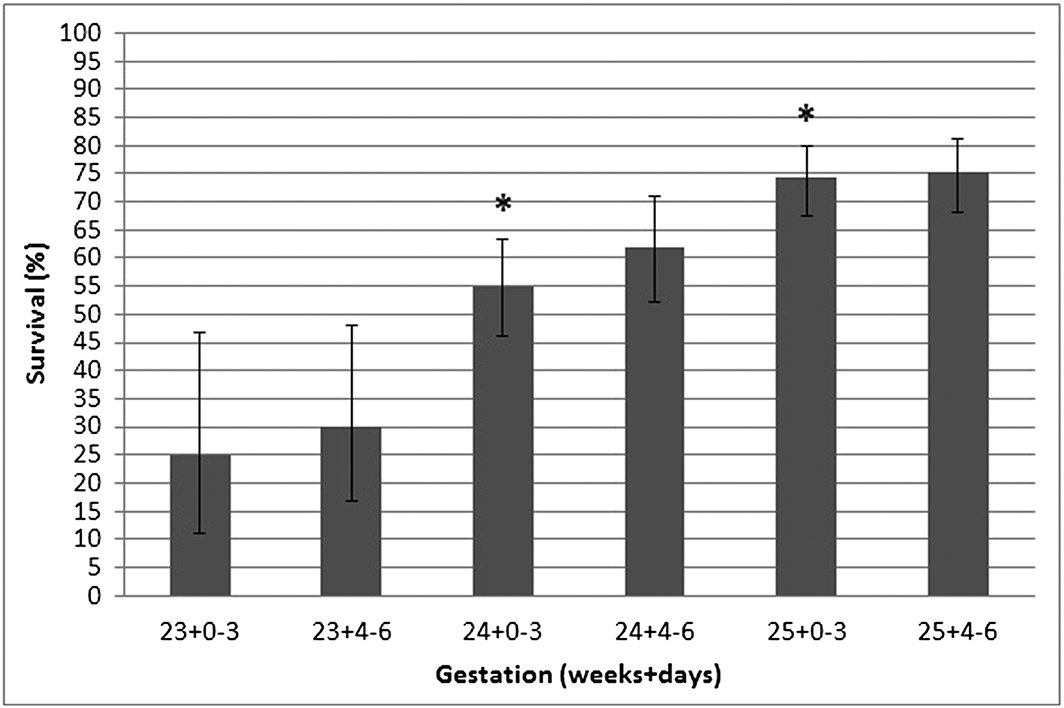
The asterisk over the two bars means that the improvement in survival was statistically significant between being born in the last half of the preceding week and the first half of the next week. In this study in other words days make a difference. A word of caution is needed here though. When you look at the variation in survival in each category one sees that while the means are statistically different the error bars show some overlap with the previous half week. At a population level we are able to say that for the average late 23 week infant survival is expected to be about 30% in this study and about 55% at 24 +0-3 days. What do you say to the individual parent though? I am not suggesting that this information is useless as it serves to provide us with an average estimate of outcome. It also is important I believe in that it suggests that dating on average is fairly accurate. Yes the dates may be off for an individual by 5 – 14 days but overall when you group everyone together when a pregnancy is dated it is reasonably accurate for the population.
Don’t become a slave to the number
The goal of this post is to remind everyone that while these numbers are important for looking at average outcomes they do not provide strict guidance for outcome at the individual level. For an individual, the prenatal history including maternal nutrition, receipt of antenatal steroids, timing of pregnancy dating and weight of the fetus are just some of the factors that may lead us to be more or less optimistic about the chances for a fetus. Any decisions to either pursue or forego treatment should be based on conversations with families taking into account all factors that are pertinent to the decision for that family. Age is just a number as people say and I worry that a graph such as the one above that is certainly interesting may be used by some to sway families one way or another based on whether the clock has turned past 12 AM. At 23 weeks 3 days and 23 hours do we really think that the patient is that much better off than at 24 weeks 4 days and 1 hour?

by All Things Neonatal | Apr 8, 2016 | preemie, Uncategorized
It seems the expression “(insert a group) lives matter” is present everywhere these days so I thought I would join in after a moving experience I had today. For those of you who have been with the blog since the beginning you would have seen a number of posts that if you follow them in time, provide a glimpse into the transformation that Winnipeg has seen over the last year or so.
Prior to that point, 24 weeks was a cutoff for resuscitation that had been in place for some time and after a great amount of deliberation and thought was changed to 23 weeks. This did not come without a great deal of angst and a tremendous amount of education and teamwork that our nurse educators and clinical leads were so instrumental in helping to role out. The experience was outlined in a couple of posts that you may find interesting if you didn’t catch them the first time. The first was Winnipeg hospital now resuscitating all infants at 22 weeks! A media led case of broken telephone. and the second being Winnipeg Hospital About to Start Resuscitating Infants at 23 weeks!
Since these two posts we have certainly had our fair share of experience as we have seen far more babies than anticipated but the region has met the challenge head on and although the numbers are small we appear to have not only more survivors than expected but all but one infant had gone home without O2 and all have been demand feeding at discharge. While we await the 18 month outcomes, the results thus far appear reassuring.
A Special & Memorable Visit
Then today, a visit occurred from the first of such infants who is now just over a year of age. He was bright eyed, smiling, interactive and by his parent’s account, has normal tone and assessments thus far by physiotherapy. His presence in the NICU put smiles on faces and at least for myself made me think of the expression “Micropreemie Lives Matter”. He was a baby that everyone predicted would not survive and then when he did, that he would be grossly developmentally impaired which he does not appear to be in the least. His presence in the unit no doubt gives everyone who doubted the merits of moving down this path reason to pause.
Before you accuse me of wearing rose coloured glasses, make no mistake I know that he will not represent the outcome for everyone. In fact at one of our hospitals two of such infants have died while we await the 18 month outcomes for the other survivors. What his presence does though, is remind us or at least me that good outcomes are possible and in the case of our experience in Winnipeg may be more common that we thought they would be.
Black Swans and Human Nature
When I have spoken to audiences about the path forward when resuscitating such ELGANS I have often commented on the “Black Swan” effect. 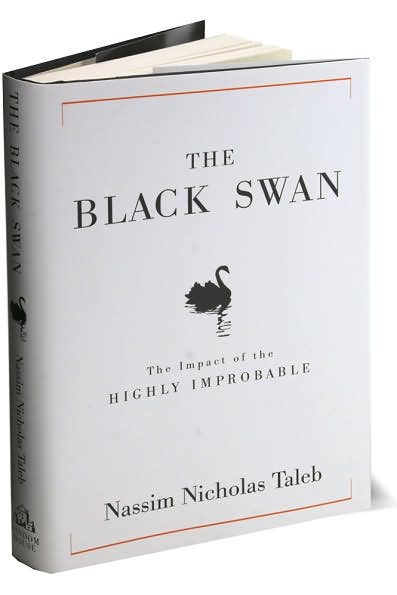 This was very nicely described by Nassim Taleb and described the human trait to react to unusual events with extreme reactions. An example is no one wanting to fly in the months after the world trade centre bombing when statistically this may have been the safest period in history to fly. Similarly, we as a team need to avoid the extreme reaction of saying that we should not be resuscitating such small infants when a bad outcome occurs. As I have told many people, we know these patients will not all survive, we know a significant number will have adverse development yet not all will and at least in our small sample thus far the babies would appear to be doing better overall than anticipated. If we know that bad outcomes will occur then why do we hear the questions come when they do such as “why are we doing this?”, “maybe we should rethink our position on 23 week infants”. It happens because we care and we hate seeing families and their babies go through such painful experiences. What we cannot do though for the sake of those such as our visitor today is react with a “Black Swan” reaction and steer the ship so to speak in the previous direction we were in. There are survivors and they may do well and that is why I say “Micropreemie Lives Matter”.
This was very nicely described by Nassim Taleb and described the human trait to react to unusual events with extreme reactions. An example is no one wanting to fly in the months after the world trade centre bombing when statistically this may have been the safest period in history to fly. Similarly, we as a team need to avoid the extreme reaction of saying that we should not be resuscitating such small infants when a bad outcome occurs. As I have told many people, we know these patients will not all survive, we know a significant number will have adverse development yet not all will and at least in our small sample thus far the babies would appear to be doing better overall than anticipated. If we know that bad outcomes will occur then why do we hear the questions come when they do such as “why are we doing this?”, “maybe we should rethink our position on 23 week infants”. It happens because we care and we hate seeing families and their babies go through such painful experiences. What we cannot do though for the sake of those such as our visitor today is react with a “Black Swan” reaction and steer the ship so to speak in the previous direction we were in. There are survivors and they may do well and that is why I say “Micropreemie Lives Matter”.
In the paper by Rysavy the overall finding at 23 weeks was that 1 out of 6 would survive without moderate or severe disability. What do we do as we increase our experience if the trend bears out that our outcomes are better? How will we counsel families? Will we continue to use the statistics from the paper or quote our own despite us being a medium sized centre?
The Big Questions
As our experience with such infants increases we will also no doubt see a change in our thoughts about infants at 24 weeks. I have seen this first hand already with a physician commenting today that 24 weeks is not such a big deal now! This brings me to the big question (which I will credit a nurse I work with for planting in my head in the last two weeks) which is for another time to answer as this post gets a little lengthy but is something to ponder. As our outcomes for 23 weeks improve and so do our results at 24 weeks (which is bound to happen with the more frequent team work in such situations) will our approach to infants at 24 weeks change. In our institution we generally follow the CPS guidelines for the management of infants at extremely low GA and offer the choice of resuscitation at 24 weeks. As outcomes improve at this GA will we continue to do so or will we reach a threshold where much like the case at 25 weeks we inform families that we will resuscitate their infant without providing the option of compassionate care?
It is too early to answer these questions conclusively but they are very deserving of some thought. Lastly, I would like to thank the parent who came by today for inspiring me and to all those who will follow afterwards.

by All Things Neonatal | Feb 25, 2016 | preemie, Prematurity, Uncategorized
It is hard to believe but All Things Neonatal is a year old. When I started this little concept I had no idea what was to come but am delighted with where it has gone. While the Blog site itself has about 200 followers, the Facebook page is home to nearly 4200 followers with twitter accounting for over 500 more. What began as a forum for me to get some thoughts off my chest about neonatal topics or articles of interest has morphed into a place to create change. As I look back over the last year I thought I would update the readers of this page and other social media platforms what the outcome has been for some of the ideas that I have brought forward. We have implemented some of these suggestions into our own unit practices, so without further ado here are the updates for some (but not all!) of the changes we have introduced.
Articles pertaining to use of Telehealth in all aspects of medicine are becoming commonplace.  Locally we have seen expansion of rural sites that can connect with us and a strong desire by existing sites to connect via telehealth for a variety of reasons. While the thrust of the program was to deliver advice to rural practitioners and support our level I and II units we have found such support leading to possibilities we had not dreamed of. Initial discussions via telehealth and in person have occurred examining whether such treatments as CPAP stabilization and NG feedings could be done in these sites. Being able to provide such care will no doubt lead to more stable infants being transported to our site and moreover the possibility of moving the care for infants needing only gavage feeding back to their home communities. Who knows what the future will hold for us as we also look forward to the hiring of a telehealth coordinator for NICU!
Locally we have seen expansion of rural sites that can connect with us and a strong desire by existing sites to connect via telehealth for a variety of reasons. While the thrust of the program was to deliver advice to rural practitioners and support our level I and II units we have found such support leading to possibilities we had not dreamed of. Initial discussions via telehealth and in person have occurred examining whether such treatments as CPAP stabilization and NG feedings could be done in these sites. Being able to provide such care will no doubt lead to more stable infants being transported to our site and moreover the possibility of moving the care for infants needing only gavage feeding back to their home communities. Who knows what the future will hold for us as we also look forward to the hiring of a telehealth coordinator for NICU!
This has been one of my favourite topics to write about. The ability to sample CO2 from an area near the carina has been demonstrated to be accurate and to save pokes in the long run. 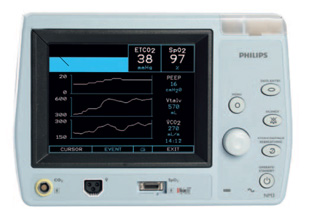 Since writing this piece we have tried it on several babies by using a double lumen tube and found the results to be as accurate as described in the Israeli papers. In practice though, secretions have proved difficult to handle for longer periods of use as they can travel up the sampling lines and damage the filters in the analyzers. A costly issue to deal with that we are currently trying to solve. Being able to continuously sample CO2 and adjust ventilation without drawing frequent blood gases is somewhat of a dream for me and we will continue to see how we can go about making this an established practice but there is work to be done!
Since writing this piece we have tried it on several babies by using a double lumen tube and found the results to be as accurate as described in the Israeli papers. In practice though, secretions have proved difficult to handle for longer periods of use as they can travel up the sampling lines and damage the filters in the analyzers. A costly issue to deal with that we are currently trying to solve. Being able to continuously sample CO2 and adjust ventilation without drawing frequent blood gases is somewhat of a dream for me and we will continue to see how we can go about making this an established practice but there is work to be done!
I think most people in Winnipeg would say the answer is yes. On this front two major positive changes have occurred in the last year in this regard.  The first is that through a generous donation and the blessing of our health region we have been able to expand the use of donor breast milk from < 1250g for a two week period to < 1500g for a one month period. This wonderful change came about after much effort and was celebrated in December as we not only expanded the eligibility criteria but partnered with the NorthernStar Mother’s Milk Bank to provide donor milk to Manitobans (Manitobans Now Able To Support Premature Infants Through Donor Milk Program!). The other change which the above post also spoke of was the potential to eliminate bovine milk altogether with the use of Prolacta (Human based human milk fortifier). While we don’t have the approval to use the product as traditionally indicated, we have used it as a “rescue” for those patients who demonstrate a clear intolerance of bovine fortifier. Such patients would traditionally receive inadequate nutrition with no other option available but now several have received such rescue and we look forward to analyzing the results of such a strategy shortly!
The first is that through a generous donation and the blessing of our health region we have been able to expand the use of donor breast milk from < 1250g for a two week period to < 1500g for a one month period. This wonderful change came about after much effort and was celebrated in December as we not only expanded the eligibility criteria but partnered with the NorthernStar Mother’s Milk Bank to provide donor milk to Manitobans (Manitobans Now Able To Support Premature Infants Through Donor Milk Program!). The other change which the above post also spoke of was the potential to eliminate bovine milk altogether with the use of Prolacta (Human based human milk fortifier). While we don’t have the approval to use the product as traditionally indicated, we have used it as a “rescue” for those patients who demonstrate a clear intolerance of bovine fortifier. Such patients would traditionally receive inadequate nutrition with no other option available but now several have received such rescue and we look forward to analyzing the results of such a strategy shortly!
Without question the most talked about change was the change in threshold for recommending resuscitation from 24 to 23 weeks.  The change took almost a year to roll out and could not have been done without a massive educational rollout that so many people (a special thank you to our nurse educators!) took part in. Looking back on the year we have now seen several infants at 23 weeks who survived with a small minority dying in the newborn period. It is too early to look at long term outcomes but I think many of us have been surprised with just how well many of these children have done. Moreover I believe we may be seeing a “creep effect” at work as the outcomes of infants under 29 weeks have also improved as we developed new guidelines to provide the best care possible to these vulnerable infants. Antenatal steroid use is up, IVH down and at least from January to September of last year no infants died at HSC under 29 weeks! I look forward to seeing our results in the future and cannot tell you how impressed I am with how our entire team came together to make this all happen!
The change took almost a year to roll out and could not have been done without a massive educational rollout that so many people (a special thank you to our nurse educators!) took part in. Looking back on the year we have now seen several infants at 23 weeks who survived with a small minority dying in the newborn period. It is too early to look at long term outcomes but I think many of us have been surprised with just how well many of these children have done. Moreover I believe we may be seeing a “creep effect” at work as the outcomes of infants under 29 weeks have also improved as we developed new guidelines to provide the best care possible to these vulnerable infants. Antenatal steroid use is up, IVH down and at least from January to September of last year no infants died at HSC under 29 weeks! I look forward to seeing our results in the future and cannot tell you how impressed I am with how our entire team came together to make this all happen!
What’s Next?
I wanted to share some of the initiatives that came forward or were chronicled on these pages over the last year to show you that this forum is not just a place for my mind to aimlessly wander. It is a place that can create change; some good, some great and no doubt some that won’t take. It has also been a place where ideas are laid out that have come from afar. From readers anywhere in the world who ask a question on one of the social media sites that get me thinking! I have enjoyed the past year and expect I will continue to enjoy what may spring forth from these pages for some time to come. Thank you for your contributions and I hope you get a little something out of this as well!

by All Things Neonatal | Dec 2, 2015 | Breastmilk, donor milk, preemie, Uncategorized
What follows is a news release from today that begins a new chapter in supporting preemies here in Manitoba. There are far too many people to thank who made this possible but to all I say THANK YOU!
New Breast Milk Drop Site at the Birth Centre Benefits Premature and Sick Infants
DECEMBER 2, 2015 (WINNIPEG, MB) – The Winnipeg Regional Health Authority (WRHA) announced today a milk drop site is being established at the Birth Centre (603 St. Mary’s Road) in Winnipeg. Minister Blady announced the collaboration between Women’s Health Clinic and the NorthernStar Mother’s Milk Bank.
Registered donations of breast milk will be accepted by the Birth Centre in Winnipeg and transported for pasteurization at NorthernStar’s lab in Calgary. The pasteurized human milk from donors will be used to help premature and sick babies in neonatal intensive care units in hospitals, and in the community, across Canada.
“There can be a number of reasons why a mother may not be able to provide breast milk for her baby,” said Health Minister Sharon Blady. “This new Milk Drop site will help families ensure premature and sick babies get the best possible start in life by providing pasteurized donor human milk an infant needs to not only survive, but thrive.”
The minister noted that establishing a human milk drop supports recommendations made in the Manitoba Breastfeeding Strategy, released in 2013.
The WRHA purchased a freezer for the milk drop with funds provided by the Winnipeg-based Siobhan Richardson Foundation. The Birth Centre will house the freezer and ensure the safe handling and storage of donated human milk before it is shipped to Calgary for processing.
“My thanks and appreciation goes out to the Siobhan Richardson Foundation for supporting new moms as well as our tiniest patients,” said Dana Erickson, Chief Operating Officer, Health Sciences Centre and WRHA executive responsible for child health and women’s health. “This milk drop initiative in Manitoba is a reality because of their vision and generosity along with the commitment and hard work of our excellent health care team.”
Studies have shown premature infants who receive the nutrients of pasteurized human milk from donors, when their mother’s own milk is not available, have fewer long-term health needs. The use of pasteurized donor human milk instead of formula can reduce the risk of serious health complications in pre-term infants. Having a dedicated milk supply for these babies can save lives.
“Several health outcomes for preterm infants are improved when pasteurized donor human milk, rather than formula, is used in these high risk infants,” said Dr. Michael Narvey, section head of neonatology for the Winnipeg Regional Health Authority. “Pasteurized donor human milk has been proven to reduce the chances of an infant developing a serious condition of the bowel which can lead to lifelong and serious health consequences. Babies weighing less than 1500 grams are significantly less likely to develop this serious condition when they are given pasteurized human milk from donors as opposed to formula.”
Starting January 4, 2016, the Birth Centre will accept breast milk from donors approved by NorthernStar Mothers Milk Bank (formerly the Calgary Mothers Milk Bank). Women must first contact the NorthernStar Mothers Milk Bank to be screened prior to dropping off their donation at the Birth Centre. Women will then need to have further screening including blood tests by their primary care provider to confirm if they qualify as a donor. These donations will be sent to the milk bank’s lab in Calgary where the donor milk is tested, pasteurized, and then prioritized for premature and sick infants.
“We are excited to see Manitoba’s first Milk Drop opening in Winnipeg,” said Janette Festival, Executive Director, NorthernStar Mothers Milk Bank. “This Milk Drop is a testament to cooperation of multiple groups who believe in the medical power of donor human milk for babies in need. We hope this new ‘drop’ will encourage women in the Winnipeg area to consider becoming a milk donor.”
Women’s Health Clinic operates the Birth Centre facility and community programming, and will be collecting the donations and shipping them to the milk bank for testing and pasteurizing.
“Women and families come to the Birth Centre every day for a range of maternal health and wellness services, making it an ideal location for the new Milk Drop site,” said Joan Dawkins, Executive Director of Women’s Health Clinic. “Women who are interested in donating can get the process underway now by contacting NorthernStar Mothers Milk Bank.”
To donate, mothers can contact the milk bank at 1-403-475-6455 or visit NorthernStarmilkbank.ca.
For more information contact:
Melissa Hoft
Winnipeg Regional Health Authority
P: (204) 926-7180 C: (204) 299-0152 E: [email protected]
Amy Tuckett
Women’s Health Clinic (Birth Centre)
P: (204) 947-2422 ext. 147 C: (204) 996-6289 E: [email protected]
Janette Festival
NorthernStar Mothers Milk Bank
P: (403) 475-6455 E: [email protected]

by All Things Neonatal | Nov 17, 2015 | Neonatal, Neonatology, preemie, Prematurity, Uncategorized
Another year has passed and another World Prematurity Day is upon us. I thought about what to write for this day that draws attention to premature infants worldwide and was hit with many ideas which no doubt will form the basis for many posts to come. There was one thought that struck me though as being so important to think about as we push forward, striving to improve survival across the globe for our smallest patients. There is no doubt that you will have heard the expression “just because we can do something, should we?” In 2015 I don’t think this applies more than at this very moment.
At a Tipping Point
You see we are at a tipping point as Malcolm Gladwell explained so brilliantly in his book by the same name.  In April of 2015 Rysavy et al published the results of survival and morbidity data for infants born in 24 US hospitals between the ages of 22 – 26 weeks. The nearly 5000 infants included demonstrated two very important things. Firstly, survival is possible at 22 and 23 weeks and there is a chance, albeit less than 50% that these infants will survive without moderate or severe disability. Secondly, at these gestational ages 75% of hospitals included provided active resuscitation to these infants. Given that this is the largest study out there and shows that survival is possible and we can expect to see some good outcomes it would seem logical to move forward with universal resuscitation of these infants would it not?
In April of 2015 Rysavy et al published the results of survival and morbidity data for infants born in 24 US hospitals between the ages of 22 – 26 weeks. The nearly 5000 infants included demonstrated two very important things. Firstly, survival is possible at 22 and 23 weeks and there is a chance, albeit less than 50% that these infants will survive without moderate or severe disability. Secondly, at these gestational ages 75% of hospitals included provided active resuscitation to these infants. Given that this is the largest study out there and shows that survival is possible and we can expect to see some good outcomes it would seem logical to move forward with universal resuscitation of these infants would it not?
You Are Going To Practice on What?!
As the saying goes though, “Perfect Practice Makes Perfect”. Not all hospitals have equal performance at these gestational ages which is demonstrated in the ranges of outcomes across hospitals as shown in the Rysavy paper. To even suggest that we need to practice on premature babies will no doubt leave many of you feeling queasy but in essence that is what is truly needed to improve our outcomes further. An infant born at 22 – 24 weeks is vastly different than one born at a later gestational age. Their skin is extremely fragile and prone to breakage with resultant risk of infection. Their lungs are in a stage of development that has yet to produce any real abundance of gas exchanging alveoli and their brains lacking the sulci and gyri that are to come many weeks later. They are in need of meticulous “best practice” care and without that their outcomes are certainly to be influenced. Depending on the centre though, you may see 5, 10, 15, 20 patients a year at these ages. How can a team possibly gain enough experience in treating these children appropriately if they see 1 or 2 every two months? Add to this that you may have 10 different Neonatologists so on average each of you may take care of one patient a year at birth. This is a recipe prone to poor outcomes if you ask me.
The Evolution of the Small Baby Unit
The answer no doubt will lie in creating smaller teams; so called “Small Baby Units”. Such units have small groups of health care providers dedicated to treating such infants thereby increasing the frequency of individuals exposure to these babies. There is some recent evidence published in Pediatrics that supports this notion. Small Baby Unit Improves Quality and Outcomes in Extremely Low Birth Weight Infants. In this study a period of two years before and four years after opening such a unit were compared across a number of measures. The findings were as follows “There was a reduction in chronic lung disease from 47.5% to 35.4% (P = .097). The rate of hospital-acquired infection decreased from 39.3% to 19.4% (P < .001). Infants being discharged with growth restriction (combined weight and head circumference <10th percentile) decreased from 62.3% to 37.3% (P = .001). Reduced resource utilization was demonstrated as the mean number per patient of laboratory tests decreased from 224 to 82 (P < .001) and radiographs decreased from 45 to 22 (P < .001).” I hope you would agree that achievements such as these are worth the effort to create such an environment. Future studies I believe will confirm these findings although having the gold standard RCT may be difficult to achieve as I suspect we will have lost equipoise.
This brings me to the final point though and that is whether we are ready as a health care system for the increase patient load that this change will bring about. Based on an expected stay of 4 months for a baby born at this age and knowing the average number of such babies delivered per year, we would be looking at about 600 patient days per year added to each hospital’s occupancy in our two centres.  This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.
This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.
How do we educate families about what to expect in the long run?
How do we support these families when they make such difficult decisions either way?
How do we support our front line staff who may hold quite discrepant viewpoints about what is “right” yet expect them to function as one team moving clearly in a direction that supports the family?
How do we ensure that our focus on our smallest infants does not distract us from the attention needed by those born at later gestational ages?
I could go on but these are just some of the questions that I hope the next year begins to tackle. We are in the midst of an evolutionary point in Neonatology and we owe it to ourselves and the families we care for to navigate this change as best we can.



 This was very nicely described by Nassim Taleb and described the human trait to react to unusual events with extreme reactions. An example is no one wanting to fly in the months after the world trade centre bombing when statistically this may have been the safest period in history to fly. Similarly, we as a team need to avoid the extreme reaction of saying that we should not be resuscitating such small infants when a bad outcome occurs. As I have told many people, we know these patients will not all survive, we know a significant number will have adverse development yet not all will and at least in our small sample thus far the babies would appear to be doing better overall than anticipated. If we know that bad outcomes will occur then why do we hear the questions come when they do such as “why are we doing this?”, “maybe we should rethink our position on 23 week infants”. It happens because we care and we hate seeing families and their babies go through such painful experiences. What we cannot do though for the sake of those such as our visitor today is react with a “Black Swan” reaction and steer the ship so to speak in the previous direction we were in. There are survivors and they may do well and that is why I say “Micropreemie Lives Matter”.
This was very nicely described by Nassim Taleb and described the human trait to react to unusual events with extreme reactions. An example is no one wanting to fly in the months after the world trade centre bombing when statistically this may have been the safest period in history to fly. Similarly, we as a team need to avoid the extreme reaction of saying that we should not be resuscitating such small infants when a bad outcome occurs. As I have told many people, we know these patients will not all survive, we know a significant number will have adverse development yet not all will and at least in our small sample thus far the babies would appear to be doing better overall than anticipated. If we know that bad outcomes will occur then why do we hear the questions come when they do such as “why are we doing this?”, “maybe we should rethink our position on 23 week infants”. It happens because we care and we hate seeing families and their babies go through such painful experiences. What we cannot do though for the sake of those such as our visitor today is react with a “Black Swan” reaction and steer the ship so to speak in the previous direction we were in. There are survivors and they may do well and that is why I say “Micropreemie Lives Matter”.
 Locally we have seen expansion of rural sites that can connect with us and a strong desire by existing sites to connect via telehealth for a variety of reasons. While the thrust of the program was to deliver advice to rural practitioners and support our level I and II units we have found such support leading to possibilities we had not dreamed of. Initial discussions via telehealth and in person have occurred examining whether such treatments as CPAP stabilization and NG feedings could be done in these sites. Being able to provide such care will no doubt lead to more stable infants being transported to our site and moreover the possibility of moving the care for infants needing only gavage feeding back to their home communities. Who knows what the future will hold for us as we also look forward to the hiring of a telehealth coordinator for NICU!
Locally we have seen expansion of rural sites that can connect with us and a strong desire by existing sites to connect via telehealth for a variety of reasons. While the thrust of the program was to deliver advice to rural practitioners and support our level I and II units we have found such support leading to possibilities we had not dreamed of. Initial discussions via telehealth and in person have occurred examining whether such treatments as CPAP stabilization and NG feedings could be done in these sites. Being able to provide such care will no doubt lead to more stable infants being transported to our site and moreover the possibility of moving the care for infants needing only gavage feeding back to their home communities. Who knows what the future will hold for us as we also look forward to the hiring of a telehealth coordinator for NICU!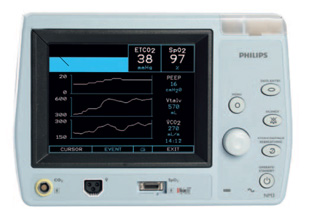 Since writing this piece we have tried it on several babies by using a double lumen tube and found the results to be as accurate as described in the Israeli papers. In practice though, secretions have proved difficult to handle for longer periods of use as they can travel up the sampling lines and damage the filters in the analyzers. A costly issue to deal with that we are currently trying to solve. Being able to continuously sample CO2 and adjust ventilation without drawing frequent blood gases is somewhat of a dream for me and we will continue to see how we can go about making this an established practice but there is work to be done!
Since writing this piece we have tried it on several babies by using a double lumen tube and found the results to be as accurate as described in the Israeli papers. In practice though, secretions have proved difficult to handle for longer periods of use as they can travel up the sampling lines and damage the filters in the analyzers. A costly issue to deal with that we are currently trying to solve. Being able to continuously sample CO2 and adjust ventilation without drawing frequent blood gases is somewhat of a dream for me and we will continue to see how we can go about making this an established practice but there is work to be done! The first is that through a generous donation and the blessing of our health region we have been able to expand the use of donor breast milk from < 1250g for a two week period to < 1500g for a one month period. This wonderful change came about after much effort and was celebrated in December as we not only expanded the eligibility criteria but partnered with the NorthernStar Mother’s Milk Bank to provide donor milk to Manitobans (
The first is that through a generous donation and the blessing of our health region we have been able to expand the use of donor breast milk from < 1250g for a two week period to < 1500g for a one month period. This wonderful change came about after much effort and was celebrated in December as we not only expanded the eligibility criteria but partnered with the NorthernStar Mother’s Milk Bank to provide donor milk to Manitobans ( The change took almost a year to roll out and could not have been done without a massive educational rollout that so many people (a special thank you to our nurse educators!) took part in. Looking back on the year we have now seen several infants at 23 weeks who survived with a small minority dying in the newborn period. It is too early to look at long term outcomes but I think many of us have been surprised with just how well many of these children have done. Moreover I believe we may be seeing a “creep effect” at work as the outcomes of infants under 29 weeks have also improved as we developed new guidelines to provide the best care possible to these vulnerable infants. Antenatal steroid use is up, IVH down and at least from January to September of last year no infants died at HSC under 29 weeks! I look forward to seeing our results in the future and cannot tell you how impressed I am with how our entire team came together to make this all happen!
The change took almost a year to roll out and could not have been done without a massive educational rollout that so many people (a special thank you to our nurse educators!) took part in. Looking back on the year we have now seen several infants at 23 weeks who survived with a small minority dying in the newborn period. It is too early to look at long term outcomes but I think many of us have been surprised with just how well many of these children have done. Moreover I believe we may be seeing a “creep effect” at work as the outcomes of infants under 29 weeks have also improved as we developed new guidelines to provide the best care possible to these vulnerable infants. Antenatal steroid use is up, IVH down and at least from January to September of last year no infants died at HSC under 29 weeks! I look forward to seeing our results in the future and cannot tell you how impressed I am with how our entire team came together to make this all happen!

 In April of 2015
In April of 2015  This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.
This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.