by All Things Neonatal | Jun 4, 2015 | Neonatology, Prematurity, Vaccination
Ask any health care professional how our tinyest babies fare after an immunization and they will tell you “not well”. In fact the belief is so pervasive that we go out of our way to find excuses to delay immunizations. I have heard myself uttering such comments as “today is not a good day” or “let’s wait until there is greater respiratory stability” or simply “they are too sick”. Perhaps this tendency develops because we are shaped by our past experiences and if we have had a baby get intubated who was on CPAP after an immunization, we subconsciously say to ourselves “that won’t happen again”.
By no means am I writing an anti-vaccination piece but rather exploring our behaviours and trying to come up with a means of changing them. Adverse Events After Routine Immunization of ELBW Infants was published on this very topic this week and with nearly 14000 infants from 23 – 28 weeks included who received their first 2 month immunization, it certainly caught my attention!
The table indicates the risks of certain adverse events in the 3 days preceding the immunization to the 3 days afterwards. 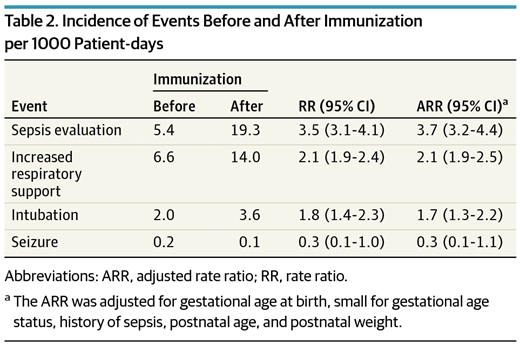 What you will note is that the evaluations for sepsis increased 4X, Respiratory support and intubation almost 2X, with no difference in seizures. It is important to note that the definitions for sepsis were based on two blood cultures being drawn rather than fever alone. Curiously with respect to sepsis there was an increase in the number of positive cultures as well from 2.1 to 3.8% in the evaluations that were done before and after. It is worth pointing out though that I can find no analysis of those results to determine if they were statistically different so at most it is an “interesting” finding.
What you will note is that the evaluations for sepsis increased 4X, Respiratory support and intubation almost 2X, with no difference in seizures. It is important to note that the definitions for sepsis were based on two blood cultures being drawn rather than fever alone. Curiously with respect to sepsis there was an increase in the number of positive cultures as well from 2.1 to 3.8% in the evaluations that were done before and after. It is worth pointing out though that I can find no analysis of those results to determine if they were statistically different so at most it is an “interesting” finding.
The figures below demonstrate the rate of the same adverse events before time zero and then afterwards for the same duration as in the table.
What you notice aside from the rise in adverse events is a sharp decline in the rate of adverse events just prior to the immunization and then a sharp rise after it is given. 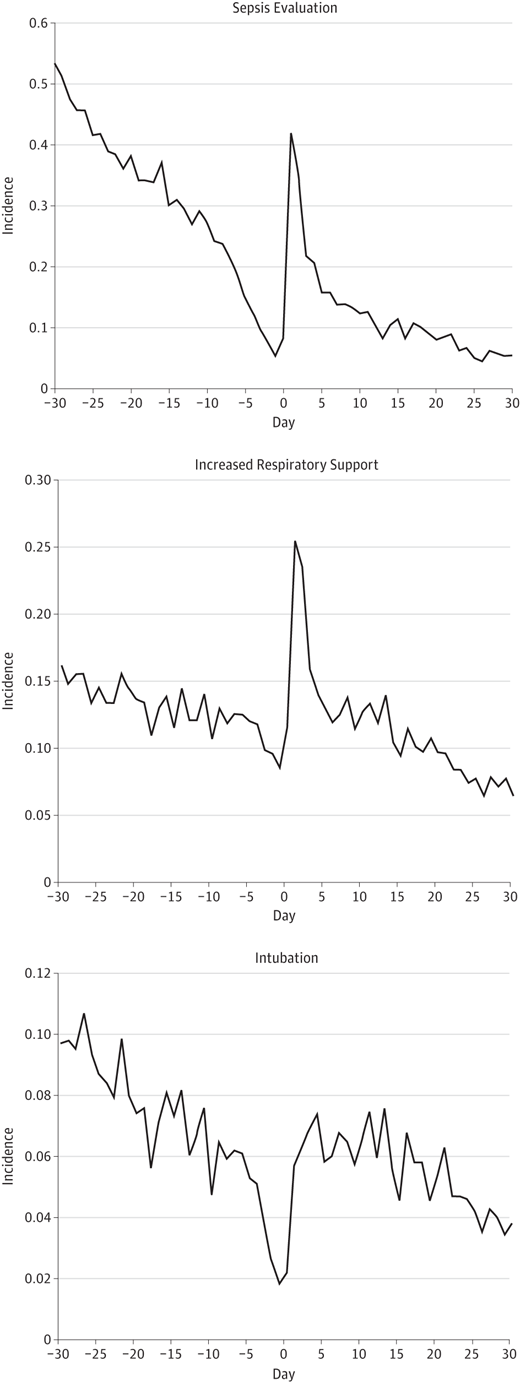 The steep decline just prior to immunization is known as the Healthy Vaccinee Effect. That is to say that we may see a higher rate of complications simply due to the fact that we wait for kids to be at their healthiest and when they have only had one or two days without apnea or are off their antibiotics that is when we choose to give the vaccine as we believe they can now “handle it”. What we have created is a special sample of patients that actually does not reflect the whole population. What I mean by this is that the response of all patients to their vaccines in this age group might be quite different with no increases in any adverse events if we paid no attention to our preconceived notions that the infant in our care is “too sick” to get their immunization. When we only immunize those kids that are at their best, the likelihood of them deteriorating is higher than when they were “worse”.
The steep decline just prior to immunization is known as the Healthy Vaccinee Effect. That is to say that we may see a higher rate of complications simply due to the fact that we wait for kids to be at their healthiest and when they have only had one or two days without apnea or are off their antibiotics that is when we choose to give the vaccine as we believe they can now “handle it”. What we have created is a special sample of patients that actually does not reflect the whole population. What I mean by this is that the response of all patients to their vaccines in this age group might be quite different with no increases in any adverse events if we paid no attention to our preconceived notions that the infant in our care is “too sick” to get their immunization. When we only immunize those kids that are at their best, the likelihood of them deteriorating is higher than when they were “worse”.
We know from previous literature that ELBW infants have higher rates of apnea and need for respiratory support after their vaccines. If we gave them an immunization when they were on CPAP or a higher dose of caffeine would we notice the impact as much? By waiting till they have weaned off CPAP or outgrown their dose of caffeine we are setting ourselves up for a setback.
Similarly perhaps the optimal time to give the vaccine is when they are actually on an antibiotic for a sepsis evaluation or have had a CRP for one reason or another in the preceding 24 hours. Would a mild fever after the vaccine trigger the same response to do a septic workup or would you take comfort in knowing your patient was already on antibiotics or had no signs of inflammation prior to the vaccine?
In summary I question if I have had it all wrong. I am not saying to give a vaccine to a patient who is on high frequency ventilation and inotropes due to septic shock but rather when they are recovering and off the inotropes but still ventilated what is the harm? They are already intubated, and covered with antibiotics. Seems to me to be the perfect conditions to prevent me from either escalating their respiratory support or doing a septic workup. They are already covered!
by All Things Neonatal | Mar 12, 2015 | General Comments

I would like to thank each and every one of you for your words of encouragement over the last three weeks since the inception of this blog. Today marked a significant event by surpassing 100 followers who receive an email with each blog post. As of tonight, there have also been almost 2000 viewings of these posts from at least 20 countries worldwide. I find these metrics informative as I really have no idea how many views happen on Facebook or Twitter but with the blog data I get a sense of how many of you are out there!
I have thoroughly enjoyed writing these pieces and really appreciate the feedback on each topic. The last few weeks have included correspondence with someone from another country who was unaware that Propranolol could be used for hemangiomas and a practical suggestion for starting children on propranolol in a day clinic type of environment. I look forward to the opening of such a clinic in our hospital in the next year or so. There is no doubt that the topic that garnered the most attention was the use of breast milk by body builders. Although this was a more playful topic it did raise awareness of the use of donor breast milk and who knows whether or not a unit somewhere may look into this through the communication that the post generated. The Sympathetic Note to the Anti-Vaxxers caused an explosion on Twitter that left me exhausted after 3 days of exchanges with people opposed to vaccination. I have to say that although it was tiring, the amount of websites, articles and information from that side of the argument that I was provided is worthy of a post in and of itself! I learned a lot from individuals on the other side of the promoting health coin and I feel as if I am a better doctor for it as I now have better insight into the basis for many of their arguments.
I have to say the pinnacle of this experience however was an exchange with someone who attributed their child’s autism to the MMR vaccine. After a bit of a lengthy exchange I was sent a picture of her beautiful daughter with a thank you for having given them some relief after reading the post on MMR. Their daughter was lovely as was the knowledge that I had helped someone who I would have otherwise never met if it weren’t for this medium.
Your support has kept my enthusiasm for writing up and on a local front I also want to thank the doctors, nurses, dieticians, RRTs and others who have encouraged this medium for education. I have really enjoyed being stopped in the NICU, IMCN or hallways to chat further about this post or that. It means a lot!
Moving forward I look forward to many more opportunities to share with you. I would like to add that I have created a twitter feed at @NICU_musings to talk about these and other topics not on the blog for those of you who are more bent on Twitter. There is also now a Facebook page at https://www.facebook.com/allthingsneonatal where discussion can also take place if you are more of a Facebook fan.
I will leave you with this news story I read tonight which reminded me of the power of community generosity that many of you know we have been blessed with here. Charitable giving is a very special and important thing and this story seemed right to finish off on a high note.
http://www.yourerie.com/news/news-article/d/story/pay-it-forward-check-helps-neonatal-intensive-care/16215/VCOYMz8je0631nC0dShYQQ

by All Things Neonatal | Feb 26, 2015 | Vaccination
Sucrose given to newborns prior to anticipated painful procedures has been used for many years now. The pooled evidence as presented by the Cochrane Database of Systematic Reviews concludes that “Sucrose is safe and effective for reducing procedural pain from single painful events (heel lance, venepuncture).” As care providers for newborns in an Intensive care setting we have become accustomed to providing this sugar to infants prior to such procedures and there is no question that we note the benefit in both subjective assessment of pain and when using more objective scoring systems.
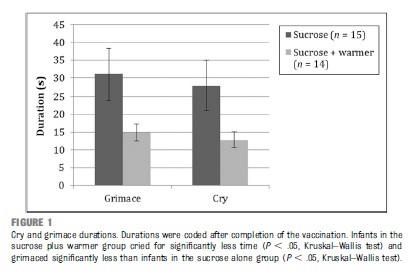
It is for this reason that I read with great interest the article by Gray L et al Pediatrics entitled Sucrose and Warmth for Analgesia in Healthy Newborns: An RCT. The study included 29 infants roughly half of which were randomized to sucrose 1 mL/kg of a 25% solution (Sweet-Ease) and the other to the same solution plus placement on an overhead warmer prior to Hepatitis B immunization. The results demonstrated a reduction in crying with both interventions compared to the sucrose alone as shown in the following figure.
An additional finding was that of a dampening of heart rate acceleration if the infant received warmth as well. There is no question that the combination of warmth and sucrose is superior to providing sucrose alone but is the study relevant today?
The infants in this paper were recruited in 2008 at a time when we as a profession were not as accustomed to Kangaroo Care or Skin to Skin care as it is also known. In the study the overhead warmer was used as a substitute for Skin to Skin care but in 2016 would we do this? Perhaps if the mother was unavailable but certainly not if we could put the infant against the mother’s chest and provide sucrose. While the study has its merits I think it fails a critical test in order to apply it in our own practice. The question must always be asked no matter what the size of an effect “Can the results of the study be applied to my patient population?”
I fear in this case the answer is no for most of our infants. The paper serves as a good reminder that while results of a study may be valid, they might just not be useful in your own practice.
Antipyretics or Sucrose for Vaccine Related Pain?
Future questions though that come to mind are whether sucrose analgesia may be useful in older children at 2,4 and 6 months. Previous research has demonstrated that while fever may be effectively treated with prophylactic antipyretics the additional finding is that of reduced antibody production to some vaccine antigens. While a reduction has been noted, even with reduced levels protection remains as the threshold for immunity is not crossed. This has been evaluated in a systematic review in 2014 pertaining to the same topic. As some practitioners though now advise against such prophylaxis might sucrose be the replacement? This has been studied in 16-19 month olds receiving a series of vaccinations and found to be an effective pain reliever as demonstrated in the paper Oral sucrose administration to reduce pain response during immunization in 16-19-month infants: a randomized, placebo-controlled trial. While the results of the study demonstrate effectiveness to reduce pain the effect on the immune response remains unanswered.
What the future will hold I don’t know but if you are looking for another option for pain relief other than acetaminophen or ibuprofen you may wish to ask your practitioner about a little sugar next time.
by All Things Neonatal | Feb 25, 2015 | Vaccination

What?! A doctor speaking out against pro-vaccination? No I haven’t switched to the other side but a recent headline caught my eye due to its potential to create a social crisis.
Imagine you have just had a baby and friends of yours who you know have not vaccinated her children want to come by for a visit. (see link) Do you freak out and deny them entry as Kristin Bell would suggest or do you ask a few questions (more delicately than “do your children have measles” and allow the visit to happen?
It seemed like a good opportunity to calm people’s nerves by reminding them of why it is that your Pediatrician will not offer the MMR vaccine prior to the age of 1 year. If you have been vaccinated as a child then you generally will have lifelong immunity to measles. The Centre For Disease Control claims that the immunity is 95% after one dose and virtually 100% after the booster dose to measles, mumps and rubella. If the vaccine though is so effective why not give it before a year to protect your vulnerable infant? The answer lies in the natural immunity that is passed from mother to fetus in the form of IgG antibodies that cross the placenta. These antibodies offer protection to the fetus and then newborn and may circulate in the infants bloodstream until 1 year of age. In essence your infant is protected from measles by virtue of your parents being sensible and vaccinating you when you were a child. The benefits of breastfeeding by passing on further antibody protection are additive (see link)!
So before anyone accuses me of being careless let me restate that I would not expose my own child under a year of age to a child that was suspected of having measles but I often worry about the effect of one celebrity sharing information such as this and the social isolation that may ensue for those parents who choose for whatever reason not to immunize. Let us also not forget that there are legitimate reasons for not immunizing your children and should these children be ostracized?
Links:
http://www.huffingtonpost.com/2015/02/17/kristen-bell-vaccinations_n_6699368.html
http://www.ncbi.nlm.nih.gov/pubmed/19133867

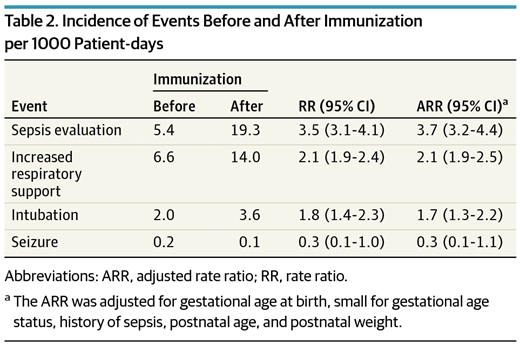 What you will note is that the evaluations for sepsis increased 4X, Respiratory support and intubation almost 2X, with no difference in seizures. It is important to note that the definitions for sepsis were based on two blood cultures being drawn rather than fever alone. Curiously with respect to sepsis there was an increase in the number of positive cultures as well from 2.1 to 3.8% in the evaluations that were done before and after. It is worth pointing out though that I can find no analysis of those results to determine if they were statistically different so at most it is an “interesting” finding.
What you will note is that the evaluations for sepsis increased 4X, Respiratory support and intubation almost 2X, with no difference in seizures. It is important to note that the definitions for sepsis were based on two blood cultures being drawn rather than fever alone. Curiously with respect to sepsis there was an increase in the number of positive cultures as well from 2.1 to 3.8% in the evaluations that were done before and after. It is worth pointing out though that I can find no analysis of those results to determine if they were statistically different so at most it is an “interesting” finding.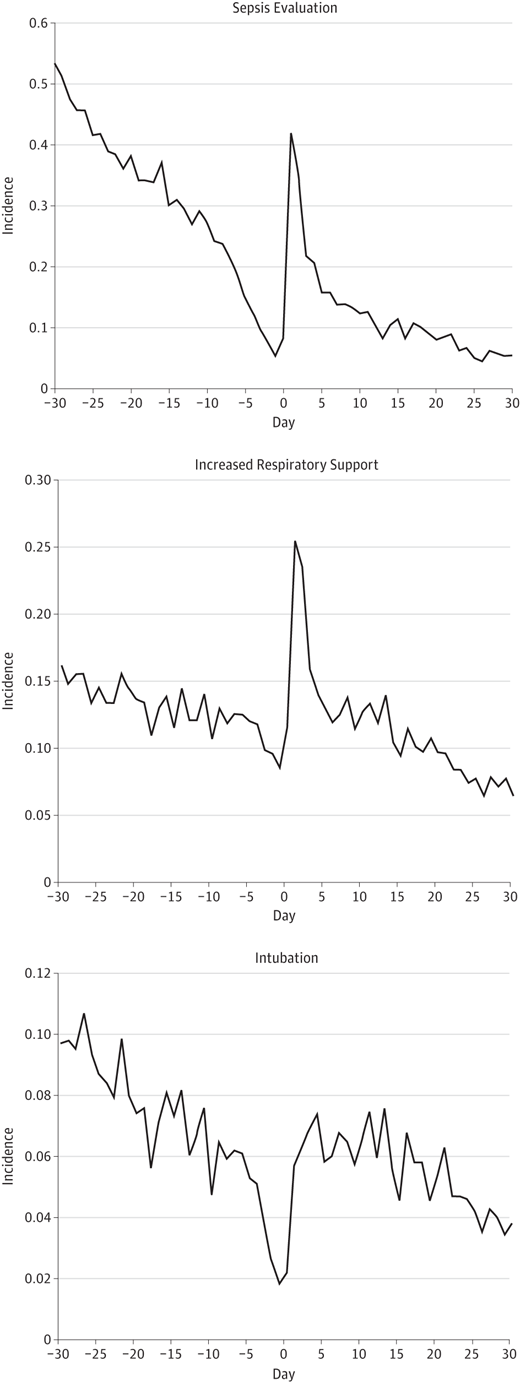 The steep decline just prior to immunization is known as the Healthy Vaccinee Effect. That is to say that we may see a higher rate of complications simply due to the fact that we wait for kids to be at their healthiest and when they have only had one or two days without apnea or are off their antibiotics that is when we choose to give the vaccine as we believe they can now “handle it”. What we have created is a special sample of patients that actually does not reflect the whole population. What I mean by this is that the response of all patients to their vaccines in this age group might be quite different with no increases in any adverse events if we paid no attention to our preconceived notions that the infant in our care is “too sick” to get their immunization. When we only immunize those kids that are at their best, the likelihood of them deteriorating is higher than when they were “worse”.
The steep decline just prior to immunization is known as the Healthy Vaccinee Effect. That is to say that we may see a higher rate of complications simply due to the fact that we wait for kids to be at their healthiest and when they have only had one or two days without apnea or are off their antibiotics that is when we choose to give the vaccine as we believe they can now “handle it”. What we have created is a special sample of patients that actually does not reflect the whole population. What I mean by this is that the response of all patients to their vaccines in this age group might be quite different with no increases in any adverse events if we paid no attention to our preconceived notions that the infant in our care is “too sick” to get their immunization. When we only immunize those kids that are at their best, the likelihood of them deteriorating is higher than when they were “worse”.