As a health care provider, I am pulled in many different directions when caring for babies in the intensive care unit. Our front line staff doing the day to day or moment to moment care and procedures are often pulled to an even greater degree and need to make choices continually as to priorities for care. As the saying goes there are only 24 hours in a day or in this case a call shift although many institutions have shortened shifts to more humane 8, 10 or 12 hour days. When you are faced with so many different calls for assistance it does leave one in a predicament as to how all of the work will get done.
A Baby With Hypoglycemia
When it comes to hypoglycemia it is a common problem in those at risk. As per the Canadian Pediatric Society statement “Some 12% to 14% of well, AGA, breastfed newborns have a blood glucose level of <2.6 mmol/L in the first 72 hours after birth”. Add to this infants who are IUGR or SGA and you have the potential to see this again and again if you work in our field. Fortunately, most infants have one or two low blood sugars and then normalize but certainly not all. I recall a situation in which a physician had a terrible night on call. When I say they were busy it was the understatement of the century. They were managing multiple sick patients overnight and fielding several calls overnight about a baby who was well aside from a pesky problem of repeated episodes of hypoglycemia. When I arrived in the morning and was reviewing the charts of the patients I noted something both peculiar and concerning. The babies with complicated and high acuity care had ample documentation of the night’s events but the baby with low blood sugars had no notes at all. Now based on my conversation with the physician it sounded like he managed the patient extremely well and followed our guidelines but there was nothing to document that this had been done. All told there were 5 or 6 low blood glucoses overnight. Before leaving for his shift, I called him and insisted he return to document what happened with the “straightforward” baby with hypoglycemia. As per the title of this post my concern was that to not document was at his peril!
Litigation Risk
If most physicians are being honest, the knowledge that we could one day face litigation for something we did or didn’t do is something that is in the back of our minds. In Canada, after a personal injury there is a general limitation of 2 years to file a statement of claim for a personal injury. In the case of a newborn this means that after a period of persistent hypoglycemia a family has up to two years to file a claim. Imagine for a moment that after hundreds of patients later you were asked at a year out for the details of that one “innocuous” baby with low blood sugars. Would you remember? I doubt it. Now of course there would need to be an injury such as cerebral palsy, developmental delay or seizure disorder to sue. This is one reason why the story gets even more challenging in the medicolegal space. Since one needs to have injury to incur compensation you may not hear about a lawsuit until the former newborn is well into their mid to late teens. In terms of determining the true impact on a child’s life, questions about school performance and ability to live independently won’t be known for many years. So let’s ask the question again. What would you remember about a baby with hypoglycemia and your thoughts about them 15 years after the fact and 1000s of patients later. Not much if anything. Now you could perhaps fall back on the nursing records but they too might be faulty or if you actually deviated from the protocol in your unit even slightly you would have nothing to fall back on to jog your memory.
Why Don’t We Document?
We know we should but here are some reasons it doesn’t happen.
We are too busy. This is probably the most common thing that you hear when asked why it didn’t happen. This is often followed by “I know I should though” There is research in the field of documentation which suggests that this actually may not be a universal factor especially in a non-intensive care environment. An institutional survey in Ethiopia revealed some interesting findings in an attempt to answer this question. They looked at 415 respondents in the paper Health professionals’ routine practice documentation and its associated factors in a resource-limited setting: a cross-sectional study. Here is a summary of the findings.
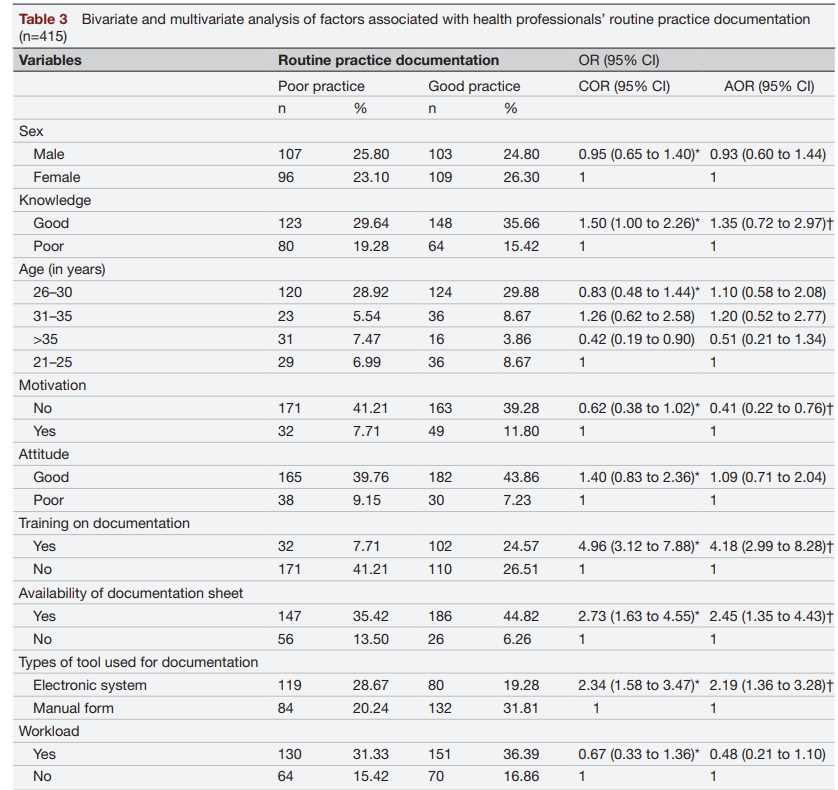
Looking at the final column representing the adjusted odds ratios what you see is that at least in this institution workload did not statistically bear out as an issue. Training on how to document carried a strong risk with the presence of specific training on how to document carrying a fourfold impact on good documentation. Having a formal documentation sheet for those using paper and using an electronic medical record also increased the chances of regular documentation. One thing that stands out though is motivation. Feeling unmotivated decreased the chance of documentation. As we have come out of the pandemic news stories abound of physician burnout. I can’t help but think that the lack of motivation for many physicians which goes against their background fear of litigation stems from burnout.
In a separate Australian study A qualitative investigation into clinical documentation: why do clinicians document the way they do? health care providers were interviewed to determine where the barriers were. What follows are some quotes from physicians that shed light into why this phenomenon of poor documentation persists.
“The things that influence whether you can or not, are the busyness of the shift. And look, you know, we’ve all got days– whether we have good days where we document everybody, and when you get complaint, you start documenting everything
left, right and centre, but that wears off after two days because you can’t get your job done.”
“Flow pressures, I think, impact significantly … if there’s a drive to move patients on …that compromises the quality of
the notes.”
“I think putting it down helps you to make the decision about what to do better. I don’t know that I could make a
decision without that, but I guess it makes me more confident in that decision. It doesn’t mean I have to write everything down, it means I need to just think about the relevant points for the decision that I’m involved in making. I just think it makes youmore confident in the decision that you’re making.”
The first quote speaks to human nature. We know we should be documenting, and we know that failure to do so is risky but time heals all wounds. Our brains lose that sense of concern, and we move on to the next patient. The second addresses the realities of working in a busy practice. The needs of the system and hospital are to achieve good patient flow which allows more patients to be seen, shorter wait times etc but the risk to this is that it leaves physicians with little time to document the patient journey. Lastly, the final quote brings an important concept to the discussion. The simple act of documentation may lead to improved care. As you lay out your thoughts other ideas or differential diagnoses or treatment options may spring forth.
Solving the Issue
I don’t want to disappoint but I don’t have a one size fits all solution to this. Working in intensive care my whole career I can see the barriers in my own field but how this compares to an office-based practice as a family doctor or in a psychiatrists office I don’t know. I suspect we all have some barriers in common and others completely foreign to one another. Electronic medical health records may help to increase efficiency in documentation but there are papers out there suggesting in some cases they can also slow people down (especially if you aren’t that tech savvy).
One thing that I hope is motivating is the realization that especially in the newborn space, it may be years before you hear about a baby that did not do well after discharge. In Neonatology we rarely find out what happens in the long run to babies after they leave our units which leads to these infants being further and further away from our minds. Knowing this and I hope this is generalizable to all health care providers there is no time like the present to document your findings and management. One possible solution however if available to you is if your hospital provides an option for secure remote computer access to the electronic health record. Many of us have busy lives outside the hospital so staying the extra hour to catch up on documentation when the shift is over may not be possible. If you have the option to go home, have a cup of tea before falling asleep and jotting down some notes in the EMR from the comfort of your home that might be an option to consider. To not document an encounter at all is to do so at your peril!

