Hypoxic Ischemic Encephalopathy or HIE is a condition in which a baby presents with cord blood gases, a gas at one hour of age, low apgar scores and neurological findings which point to an event occurring that has interrupted blood flow to the brain. The Canadian Pediatric Society further defines this by looking at who may benefit from whole body cooling to mitigate the risk of an abnormal outcome for these patients. The criteria are shown below from the CPS Guideline
Invariably when HIE has occurred and there is neurological injury, two predominant patterns appear on MRI. The first is of a subacute hypoxic injury that typically involves multiple areas of the brain such as the frontal, parietal and occipital lobes but in particular the cortex. When a sentinel event has occurred, which is defined as a sudden interruption of blood supply to the fetus, the pattern is decidedly different. This may occur in such situations as an acute abruption, or umbilical cord compression as with cord presentation. When this occurs, the pattern is more typically white matter injury along with involvement of deep brain structures such as the thalami and basal ganglia (putamen and globus pallidus as examples).
Can Bloodwork Give Us Clues As To When The Injury Occurred?
One of the questions that I am often asked is to determine when such injury occurred. Is this an injury that was sustained a day or two before birth or during labor minutes or hours prior to delivery. The timing of such injury is often difficult to determine. It is said that about 90% of such injuries do not occur during labor but that of course leaves 10% that do. Alternatively, the number might be greater than 10% but it is simply difficult to really determine timing but 10% is a best guess.
I had often relied on what I felt was a logical conclusion that in the presence of an acute and profound interruption of blood supply sufficient enough to cause neurological injury that there would be similar perturbations of blood work in the newborn. The absence of renal, hepatic or coagulation disturbance would mean one of two things. Either the injury was remote and while profound, the fetus had recovered and these disturbances resolved or absence indicated to look for another etiology.
Recently the following paper has led me to a different conclusion. Broni et al published Blood Biomarkers for Neonatal Hypoxic-Ischemic Encephalopathy in the Presence and Absence of Sentinel Events. The authors performed a retrospective analysis of all neonates with HIE admitted to their NICU with sentinel events in the first three days of life and compared them to those without. All infants met the criteria for whole body cooling and were cooled for three days. The goal was to see how those infants with a sentinel event compared to those without in terms of patterns of bloodwork. Presumably those with sentinel events since they were so severe might show a different pattern of bloodwork after birth.
What Did They Find?
The authors had 277 babies with HIE treated with whole body hypothermia. The blood used to look for biomarkers was discarded blood not used for regular sampling and in all there were 68.6% of babies that had such blood for analysis. Of the babies tested 40.5% had a sentinel event and 59.6% did not.
In terms of baseline characteristics, the groups were similar with the exception (not surprisingly) that there were 32 women with abruptions in the sentinel event group and none in the no sentinel event group. Also, meconium was present at delivery about 2.5 times as common with the subacute patients than the sentinel event group.
The goal of the study was to look at biomarkers.
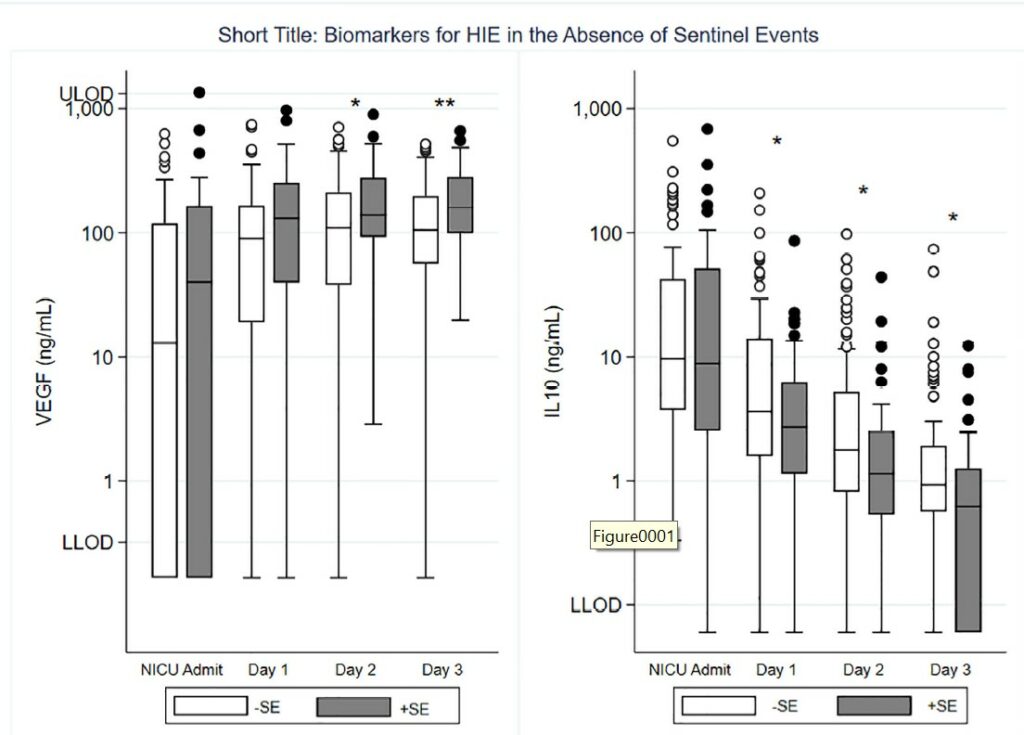
The authors examined a wide range of them but the only two that showed a significant difference in babies with and without sentinel events were vascular endothelial growth factor (VEGF) and IL-10. VEGF levels increase in the presence of hypoxia related to placental secretion of the factor. IL-10 levels increase during hypoxia and is protective since it inhibits secretion of IL-1β, IL-8 and TNF-α. This interrupts the production of leukocyte aggregation, and reduces inflammatory responses in the brain. Looking at the first figure you can see that VEGF levels were higher in those with sentinel events on day 2 and 3 while IL-10 levels were lower on days 1-3 in those with sentinel events. In other words, in the presence of a sentinel event there higher VEGF levels are present after hypoxia and protective IL-10 levels are lower.
Looking at Figure 2, other than initial glucose being lower in those with sentinel events (but not clinically relevant as still above normal) one cannot discern any differences between those with and without a sentinel event.
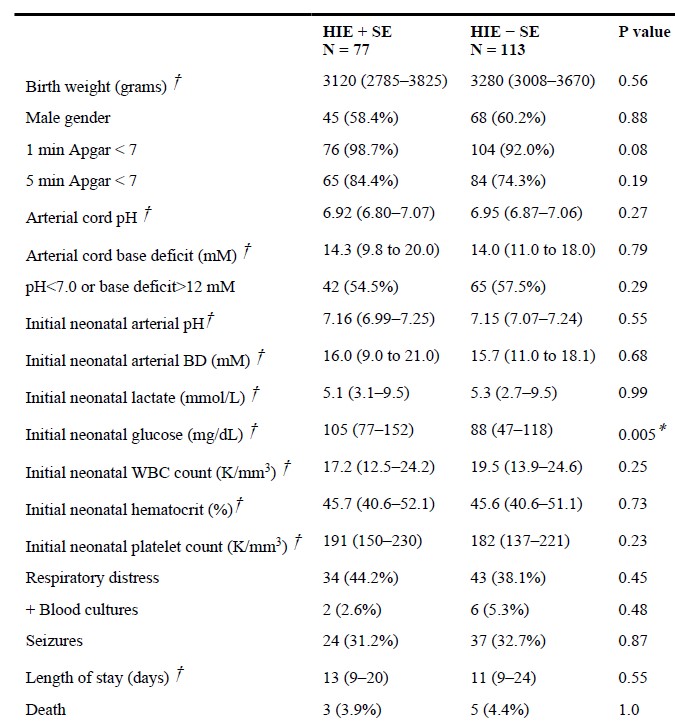
Possibly even more surprising is that my long held belief that those with a sentinel event should have significant multiorgan system involvement doesn’t appear to be true. Such things as platelet counts, white blood cell counts and initial blood gases show no difference between groups.
Putting it all together
The authors here have shown that two biomarkers display different patterns in babies born after a sentinel event than those with a subacute hypoxic course. It is possible that had they been able to test blood from all babies instead of 68.6% the results may have been different but there is biological plausibility to a more acute and severe event having this pattern of greater hypoxic injury since these babies are also at risk for significant neurological impairment later on. These tests are not routinely done but, in the future, might there be a role for drawing IL-10 and VEGF levels when trying to determine etiology?
What was also surprising was the fact that not all babies with sentinel events show a clear pattern of that demonstrates they fall into that group. The clinical appearance alone does not differ between the two groups of patients with HIE. While liver, renal and coagulation systems were not individually reported here, the lack of difference at one hour in terms of blood gases, lactates and platelet counts suggests that it would be unlikely to see a difference in those end organs. If measures of perfusion are no different as measured by gases and lactates then why would organ injury be different?
At least for me my conclusion is that laboratory measures are not able to discern whether a sentinel event occurred or not. Additionally, those who believe that the absence of laboratory markers indicate that an injury occurred remotely and the baby recovered should be careful in making such conclusions solely based on laboratory data. It will be interesting to see if anyone begins testing IL-10 and VEGF levels routinely in such patients but I guess time will tell.

