by All Things Neonatal | Jul 9, 2016 | preemie, Prematurity, Uncategorized
Preterm infants born between 22 to 25 weeks gestational age has been a topic covered in this blog before.
I think it is safe to say that this topic stirs up emotions on both sides of the argument of how aggressive to be when it comes to resuscitating some of these infants, particularly those at 22 and 23 weeks. Where I work we have drawn a line at 23 weeks for active resuscitation but there are those that would point out the challenge of creating such a hard-line when the accuracy of dating a pregnancy can be off by anywhere from 5 – 14 days. Having said that, this is what we have decided after much deliberation and before entertaining anything further it is critical to determine how well these infants are doing not just in terms of survival but also in the long run. In the next 6 months our first cohort should be coming up for their 18 month follow ups so this will be an informative time for sure.
Do Days Matter?
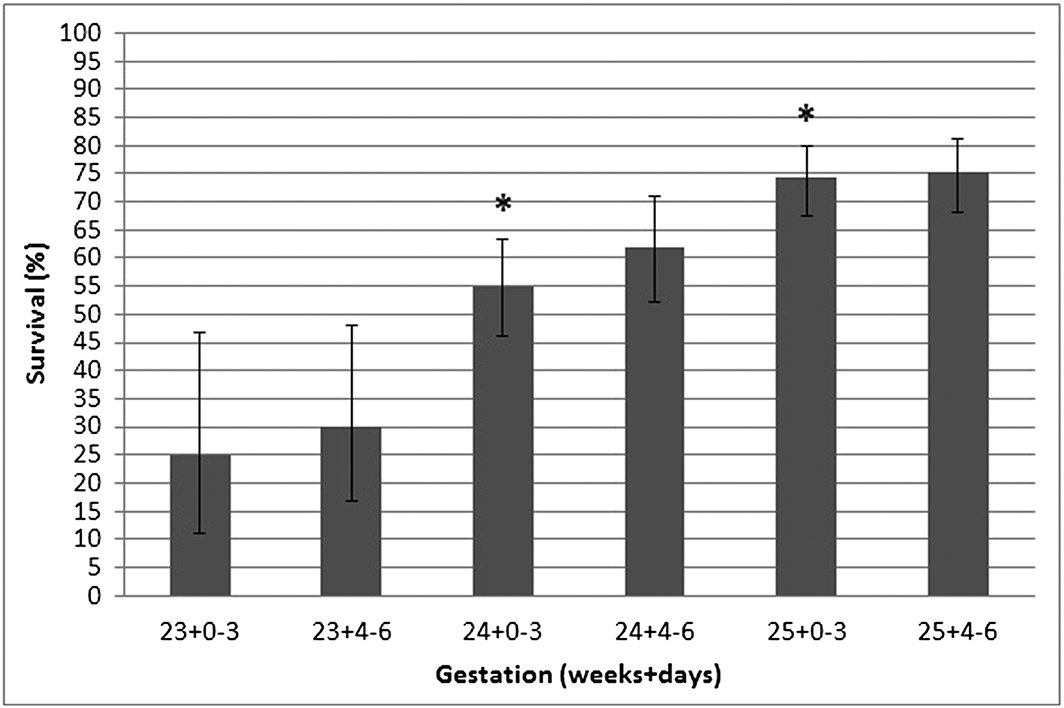
This is the subject of a short report out of Australia by Schindler T et al. In this communication they looked at the survival alone for preterm infants in a larger study but broke them down into 3 and four-day periods from 23 to 25 weeks as shown below.
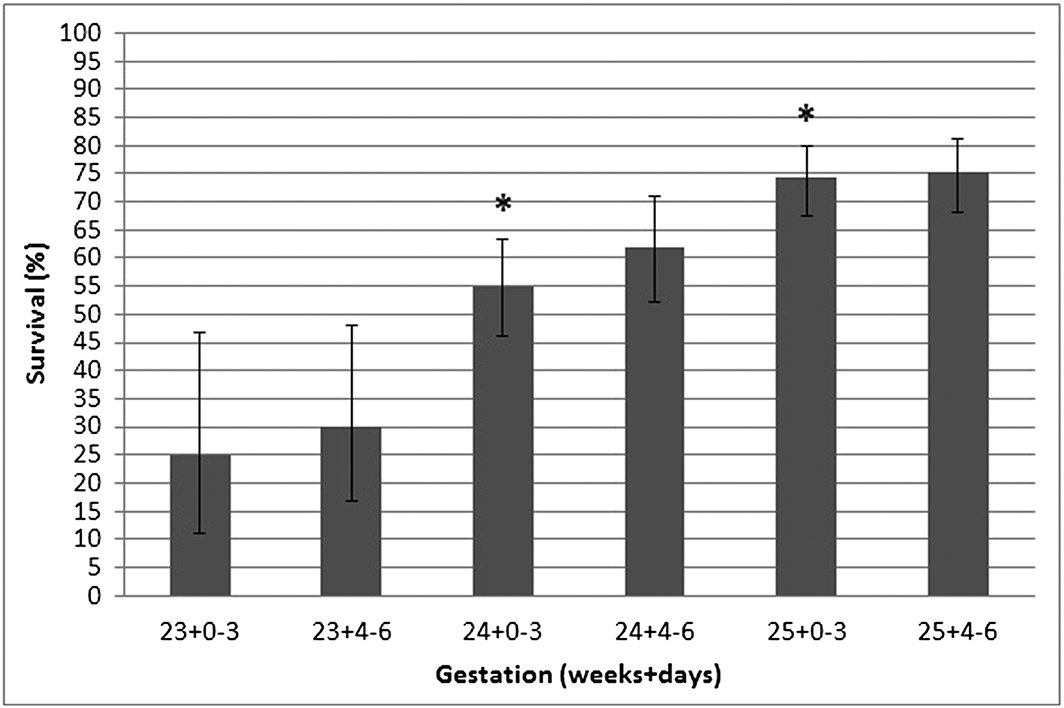
The asterisk over the two bars means that the improvement in survival was statistically significant between being born in the last half of the preceding week and the first half of the next week. In this study in other words days make a difference. A word of caution is needed here though. When you look at the variation in survival in each category one sees that while the means are statistically different the error bars show some overlap with the previous half week. At a population level we are able to say that for the average late 23 week infant survival is expected to be about 30% in this study and about 55% at 24 +0-3 days. What do you say to the individual parent though? I am not suggesting that this information is useless as it serves to provide us with an average estimate of outcome. It also is important I believe in that it suggests that dating on average is fairly accurate. Yes the dates may be off for an individual by 5 – 14 days but overall when you group everyone together when a pregnancy is dated it is reasonably accurate for the population.
Don’t become a slave to the number
The goal of this post is to remind everyone that while these numbers are important for looking at average outcomes they do not provide strict guidance for outcome at the individual level. For an individual, the prenatal history including maternal nutrition, receipt of antenatal steroids, timing of pregnancy dating and weight of the fetus are just some of the factors that may lead us to be more or less optimistic about the chances for a fetus. Any decisions to either pursue or forego treatment should be based on conversations with families taking into account all factors that are pertinent to the decision for that family. Age is just a number as people say and I worry that a graph such as the one above that is certainly interesting may be used by some to sway families one way or another based on whether the clock has turned past 12 AM. At 23 weeks 3 days and 23 hours do we really think that the patient is that much better off than at 24 weeks 4 days and 1 hour?

by All Things Neonatal | Feb 25, 2016 | preemie, Prematurity, Uncategorized
It is hard to believe but All Things Neonatal is a year old. When I started this little concept I had no idea what was to come but am delighted with where it has gone. While the Blog site itself has about 200 followers, the Facebook page is home to nearly 4200 followers with twitter accounting for over 500 more. What began as a forum for me to get some thoughts off my chest about neonatal topics or articles of interest has morphed into a place to create change. As I look back over the last year I thought I would update the readers of this page and other social media platforms what the outcome has been for some of the ideas that I have brought forward. We have implemented some of these suggestions into our own unit practices, so without further ado here are the updates for some (but not all!) of the changes we have introduced.
Articles pertaining to use of Telehealth in all aspects of medicine are becoming commonplace.  Locally we have seen expansion of rural sites that can connect with us and a strong desire by existing sites to connect via telehealth for a variety of reasons. While the thrust of the program was to deliver advice to rural practitioners and support our level I and II units we have found such support leading to possibilities we had not dreamed of. Initial discussions via telehealth and in person have occurred examining whether such treatments as CPAP stabilization and NG feedings could be done in these sites. Being able to provide such care will no doubt lead to more stable infants being transported to our site and moreover the possibility of moving the care for infants needing only gavage feeding back to their home communities. Who knows what the future will hold for us as we also look forward to the hiring of a telehealth coordinator for NICU!
Locally we have seen expansion of rural sites that can connect with us and a strong desire by existing sites to connect via telehealth for a variety of reasons. While the thrust of the program was to deliver advice to rural practitioners and support our level I and II units we have found such support leading to possibilities we had not dreamed of. Initial discussions via telehealth and in person have occurred examining whether such treatments as CPAP stabilization and NG feedings could be done in these sites. Being able to provide such care will no doubt lead to more stable infants being transported to our site and moreover the possibility of moving the care for infants needing only gavage feeding back to their home communities. Who knows what the future will hold for us as we also look forward to the hiring of a telehealth coordinator for NICU!
This has been one of my favourite topics to write about. The ability to sample CO2 from an area near the carina has been demonstrated to be accurate and to save pokes in the long run. 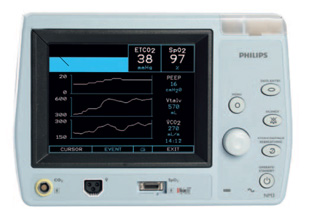 Since writing this piece we have tried it on several babies by using a double lumen tube and found the results to be as accurate as described in the Israeli papers. In practice though, secretions have proved difficult to handle for longer periods of use as they can travel up the sampling lines and damage the filters in the analyzers. A costly issue to deal with that we are currently trying to solve. Being able to continuously sample CO2 and adjust ventilation without drawing frequent blood gases is somewhat of a dream for me and we will continue to see how we can go about making this an established practice but there is work to be done!
Since writing this piece we have tried it on several babies by using a double lumen tube and found the results to be as accurate as described in the Israeli papers. In practice though, secretions have proved difficult to handle for longer periods of use as they can travel up the sampling lines and damage the filters in the analyzers. A costly issue to deal with that we are currently trying to solve. Being able to continuously sample CO2 and adjust ventilation without drawing frequent blood gases is somewhat of a dream for me and we will continue to see how we can go about making this an established practice but there is work to be done!
I think most people in Winnipeg would say the answer is yes. On this front two major positive changes have occurred in the last year in this regard.  The first is that through a generous donation and the blessing of our health region we have been able to expand the use of donor breast milk from < 1250g for a two week period to < 1500g for a one month period. This wonderful change came about after much effort and was celebrated in December as we not only expanded the eligibility criteria but partnered with the NorthernStar Mother’s Milk Bank to provide donor milk to Manitobans (Manitobans Now Able To Support Premature Infants Through Donor Milk Program!). The other change which the above post also spoke of was the potential to eliminate bovine milk altogether with the use of Prolacta (Human based human milk fortifier). While we don’t have the approval to use the product as traditionally indicated, we have used it as a “rescue” for those patients who demonstrate a clear intolerance of bovine fortifier. Such patients would traditionally receive inadequate nutrition with no other option available but now several have received such rescue and we look forward to analyzing the results of such a strategy shortly!
The first is that through a generous donation and the blessing of our health region we have been able to expand the use of donor breast milk from < 1250g for a two week period to < 1500g for a one month period. This wonderful change came about after much effort and was celebrated in December as we not only expanded the eligibility criteria but partnered with the NorthernStar Mother’s Milk Bank to provide donor milk to Manitobans (Manitobans Now Able To Support Premature Infants Through Donor Milk Program!). The other change which the above post also spoke of was the potential to eliminate bovine milk altogether with the use of Prolacta (Human based human milk fortifier). While we don’t have the approval to use the product as traditionally indicated, we have used it as a “rescue” for those patients who demonstrate a clear intolerance of bovine fortifier. Such patients would traditionally receive inadequate nutrition with no other option available but now several have received such rescue and we look forward to analyzing the results of such a strategy shortly!
Without question the most talked about change was the change in threshold for recommending resuscitation from 24 to 23 weeks.  The change took almost a year to roll out and could not have been done without a massive educational rollout that so many people (a special thank you to our nurse educators!) took part in. Looking back on the year we have now seen several infants at 23 weeks who survived with a small minority dying in the newborn period. It is too early to look at long term outcomes but I think many of us have been surprised with just how well many of these children have done. Moreover I believe we may be seeing a “creep effect” at work as the outcomes of infants under 29 weeks have also improved as we developed new guidelines to provide the best care possible to these vulnerable infants. Antenatal steroid use is up, IVH down and at least from January to September of last year no infants died at HSC under 29 weeks! I look forward to seeing our results in the future and cannot tell you how impressed I am with how our entire team came together to make this all happen!
The change took almost a year to roll out and could not have been done without a massive educational rollout that so many people (a special thank you to our nurse educators!) took part in. Looking back on the year we have now seen several infants at 23 weeks who survived with a small minority dying in the newborn period. It is too early to look at long term outcomes but I think many of us have been surprised with just how well many of these children have done. Moreover I believe we may be seeing a “creep effect” at work as the outcomes of infants under 29 weeks have also improved as we developed new guidelines to provide the best care possible to these vulnerable infants. Antenatal steroid use is up, IVH down and at least from January to September of last year no infants died at HSC under 29 weeks! I look forward to seeing our results in the future and cannot tell you how impressed I am with how our entire team came together to make this all happen!
What’s Next?
I wanted to share some of the initiatives that came forward or were chronicled on these pages over the last year to show you that this forum is not just a place for my mind to aimlessly wander. It is a place that can create change; some good, some great and no doubt some that won’t take. It has also been a place where ideas are laid out that have come from afar. From readers anywhere in the world who ask a question on one of the social media sites that get me thinking! I have enjoyed the past year and expect I will continue to enjoy what may spring forth from these pages for some time to come. Thank you for your contributions and I hope you get a little something out of this as well!

by All Things Neonatal | Jan 7, 2016 | Innovation, Neonatology, Prematurity
In the spirit of full disclosure I have to admit I have never placed a laryngeal mask airway (LMA) in a newborn of any gestational age. I have played with them in simulated environments and on many occasion mentioned that they are a great alternative to an ETT especially in those situations where intubation may not be possible due to the skill of the provider or the difficulty of the airway in the setting of micrognathia for example.
In recent years though we have heard of examples of surfactant delivery via these same devices although typically these were only case reports. More recently a small randomized study of 26 infants by Attridge et al demonstrated in the group randomized to surfactant administration through an LMA that oxygen requirements were reduced after dosing. This small pilot provides sufficient evidence to show that it is possible to provide surfactant and that at least some gets into the airway of the newborn. This proof of concept though while interesting, did not answer the question of whether such delivery of surfactant would be the same or better than through an ETT. As readers of my blog posts know, my usual stance on things is that the less invasive the better and as I look through the literature, I am drawn to concepts such as this to see if they can be added to our toolbox of non or less invasive strategies in the newborn.
A Minimally Invasive Technique For The Masses?
This past month, a small study by Pinheiro et al sought to answer this question by using 61 newborns between 29 0/7 – 36 6/7 weeks and greater than 1000g and randomizing them to either surfactant via the INSURE technique or LMA. I cannot stress enough so will get it out of the way at the start that this strategy is not for those <1000g as the LMA is not designed to fit them properly and the results (to be shown) should not be generalized to this population. Furthermore then study included only those infants who needed surfactant between 4 – 48 hours of age, were on CPAP of at least 5 cm H2O and were receiving FiO2 between 30 – 60%. All infants given surfactant via the insure technique were premedicated with atropine and morphine while those having an LMA received atropine only. The primary outcome of the study was need for subsequent intubation or naloxone within 1 hour of surfactant administration. The study was stopped early after an interim analysis (done as the fellow involved was finishing their fellowship – on a side note I find this an odd reason to stop) demonstrated better outcomes in the group randomized to the LMA.
Before we get into the results let’s address the possible shortcomings of the study as they might already be bouncing around your heads. This study could not be blinded and therefore there could be a significant bias to the results. The authors did have predetermined criteria for reintubation and although not presented, indicate that those participating stuck to these criteria so we may have to acknowledge they did the best they could here. Secondly the study did not reach their numbers for enrolment based on their power calculation. This may be ok though as they found a difference which is significant. If they had found no difference I don’t think I would be even writing this entry! Lastly this study used a dose of surfactant at 3 mL/kg. How well would this work with the formulation that we use BLES that requires 5 mL/kg?
What were the results?
| Intervention Failure |
LMA Group |
ETT group |
p |
| Any failure |
9 (30%) |
23(77%) |
<0.001 |
| Early failure |
1 (3%) |
20 (67%) |
<0.001 |
| Late failure |
8 (27%) |
3 (10%) |
0.181 |
What do these results tell us? The majority of failures occurred within an hour of delivery of surfactant in the ETT group? How does this make any sense? Gastric aspirates for those in the LMA group but not the INSURE group suggest some surfactant missed the lung in the former so one would think the intubation group should have received more surfactant overall however it would appear to be the premedication. The rate of needing surfactant afterwards is no different and in fact there is a trend to needing reintubation more often in the LMA group but the study was likely underpowered to detect this difference. Only two patients were given naloxone to reverse the respiratory depressive effects of morphine in those given the INSURE technique so I can’t help but speculate that if this practice was more frequent many of the reintubations might have been avoided. This group was quite aggressive in sticking to the concept of INSURE as they aimed to extubate following surfactant after 5 – 15 minutes. I am a strong advocate of providing RSI to those being electively intubated but if the goal is to extubate quickly then I believe one must be ready to administer naloxone soon after extubation if signs of respiratory depression are present and this did not happen effectively in this study. Some may argue those getting the INSURE technique should not be given any premedication at all but that is a debate that will go on for years I am sure but they may have a valid point given this data.
Importantly complications following either procedure were minimal and no different in either group.
Where do we go from here?
Despite some of the points above I think this study could prove to be important for several reasons. I think it demonstrates that in larger preterm infants it is possible to avoid any mechanical ventilation and still administer surfactant. Many studies using the minimally invasive surfactant treatment (MIST) approach have been done but these still require the skill of laryngoscopy which takes a fair bit of skill to master. The LMA on the other hand is quite easy to place and is a skill that can be taught widely. Secondly, we know that even a brief period of over distension from PPV can be harmful to the lung therefore a strategy which avoids intubation and direct pressure to the lung may offer some longer term benefit although again this was not the study to demonstrate that.
Lastly, I see this as a strategy to look at in more rural locations where access to highly skilled level III care may not be readily available. We routinely field calls from rural sites with preterm infants born with RDS and the health care provider either is unable to intubate or is reluctant to try in favour of using high flow oxygen via mask. Many do not have CPAP either to support such infants so by the time our Neonatal Transport team arrives the RDS is quite significant. Why not try surfactant through the LMA? If it is poorly seated over the airway and the dose goes into the stomach I don’t see them being in any worse shape than if they waited for the team to arrive. If some or all of the dose gets in though there could be real benefit.
Might this be right for your centre? As we think about outreach education and NRP I think this may well become a strong reason to spend a little more time on LMA training. We may be on to something!

by All Things Neonatal | Nov 17, 2015 | Neonatal, Neonatology, preemie, Prematurity, Uncategorized
Another year has passed and another World Prematurity Day is upon us. I thought about what to write for this day that draws attention to premature infants worldwide and was hit with many ideas which no doubt will form the basis for many posts to come. There was one thought that struck me though as being so important to think about as we push forward, striving to improve survival across the globe for our smallest patients. There is no doubt that you will have heard the expression “just because we can do something, should we?” In 2015 I don’t think this applies more than at this very moment.
At a Tipping Point
You see we are at a tipping point as Malcolm Gladwell explained so brilliantly in his book by the same name.  In April of 2015 Rysavy et al published the results of survival and morbidity data for infants born in 24 US hospitals between the ages of 22 – 26 weeks. The nearly 5000 infants included demonstrated two very important things. Firstly, survival is possible at 22 and 23 weeks and there is a chance, albeit less than 50% that these infants will survive without moderate or severe disability. Secondly, at these gestational ages 75% of hospitals included provided active resuscitation to these infants. Given that this is the largest study out there and shows that survival is possible and we can expect to see some good outcomes it would seem logical to move forward with universal resuscitation of these infants would it not?
In April of 2015 Rysavy et al published the results of survival and morbidity data for infants born in 24 US hospitals between the ages of 22 – 26 weeks. The nearly 5000 infants included demonstrated two very important things. Firstly, survival is possible at 22 and 23 weeks and there is a chance, albeit less than 50% that these infants will survive without moderate or severe disability. Secondly, at these gestational ages 75% of hospitals included provided active resuscitation to these infants. Given that this is the largest study out there and shows that survival is possible and we can expect to see some good outcomes it would seem logical to move forward with universal resuscitation of these infants would it not?
You Are Going To Practice on What?!
As the saying goes though, “Perfect Practice Makes Perfect”. Not all hospitals have equal performance at these gestational ages which is demonstrated in the ranges of outcomes across hospitals as shown in the Rysavy paper. To even suggest that we need to practice on premature babies will no doubt leave many of you feeling queasy but in essence that is what is truly needed to improve our outcomes further. An infant born at 22 – 24 weeks is vastly different than one born at a later gestational age. Their skin is extremely fragile and prone to breakage with resultant risk of infection. Their lungs are in a stage of development that has yet to produce any real abundance of gas exchanging alveoli and their brains lacking the sulci and gyri that are to come many weeks later. They are in need of meticulous “best practice” care and without that their outcomes are certainly to be influenced. Depending on the centre though, you may see 5, 10, 15, 20 patients a year at these ages. How can a team possibly gain enough experience in treating these children appropriately if they see 1 or 2 every two months? Add to this that you may have 10 different Neonatologists so on average each of you may take care of one patient a year at birth. This is a recipe prone to poor outcomes if you ask me.
The Evolution of the Small Baby Unit
The answer no doubt will lie in creating smaller teams; so called “Small Baby Units”. Such units have small groups of health care providers dedicated to treating such infants thereby increasing the frequency of individuals exposure to these babies. There is some recent evidence published in Pediatrics that supports this notion. Small Baby Unit Improves Quality and Outcomes in Extremely Low Birth Weight Infants. In this study a period of two years before and four years after opening such a unit were compared across a number of measures. The findings were as follows “There was a reduction in chronic lung disease from 47.5% to 35.4% (P = .097). The rate of hospital-acquired infection decreased from 39.3% to 19.4% (P < .001). Infants being discharged with growth restriction (combined weight and head circumference <10th percentile) decreased from 62.3% to 37.3% (P = .001). Reduced resource utilization was demonstrated as the mean number per patient of laboratory tests decreased from 224 to 82 (P < .001) and radiographs decreased from 45 to 22 (P < .001).” I hope you would agree that achievements such as these are worth the effort to create such an environment. Future studies I believe will confirm these findings although having the gold standard RCT may be difficult to achieve as I suspect we will have lost equipoise.
This brings me to the final point though and that is whether we are ready as a health care system for the increase patient load that this change will bring about. Based on an expected stay of 4 months for a baby born at this age and knowing the average number of such babies delivered per year, we would be looking at about 600 patient days per year added to each hospital’s occupancy in our two centres.  This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.
This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.
How do we educate families about what to expect in the long run?
How do we support these families when they make such difficult decisions either way?
How do we support our front line staff who may hold quite discrepant viewpoints about what is “right” yet expect them to function as one team moving clearly in a direction that supports the family?
How do we ensure that our focus on our smallest infants does not distract us from the attention needed by those born at later gestational ages?
I could go on but these are just some of the questions that I hope the next year begins to tackle. We are in the midst of an evolutionary point in Neonatology and we owe it to ourselves and the families we care for to navigate this change as best we can.

by All Things Neonatal | Oct 1, 2015 | Prematurity
Its hard not to hear about probiotics these days. They are in our grocery aisles as supplements to yoghurt and other foods and can be purchased in health food stores or at your local pharmacy. They appear to be everywhere as word spreads about the importance of your microbiome in maintaining good overall health. The first food to have probiotics added to it was a Japanese drink called Yakult  and after that the concept took off with Danone’s Activa drink not being far behind. Medicine has studied the effects of probiotics for all sorts of conditions with a pubmed search for reviews of probiotics in humans coming up with over 1800 results. The concept is enticing for sure. Take bacteria which are known to populate healthy intestines and provide them either in food or in capsules to change the bacterial population in patients who for one reason or another have cause to believe their intestinal microbiome has shifted to something undesirable.
and after that the concept took off with Danone’s Activa drink not being far behind. Medicine has studied the effects of probiotics for all sorts of conditions with a pubmed search for reviews of probiotics in humans coming up with over 1800 results. The concept is enticing for sure. Take bacteria which are known to populate healthy intestines and provide them either in food or in capsules to change the bacterial population in patients who for one reason or another have cause to believe their intestinal microbiome has shifted to something undesirable.
Do Probiotics Reduce The Risk of Necrotizing Enterocolitis?
It didn’t take long for clinician scientists to turn their attention to the neonate who is at risk of necrotizing enterocolits (NEC). It has been known for some time that formula feeding versus breast milk plays a role in the development of NEC as premature infants fed formula repeatedly were found across studies to have a higher incidence of NEC. The evidence is so strong in fact that the Cochrane review on the subject states “Enteral supplementation of probiotics prevents severe NEC and all cause mortality in preterm infants. Our updated review of available evidence strongly supports a change in practice.” If you have read such reviews you know that they rarely come out this strong in their support of something! Furthermore, infants fed formula may have a different preponderance of more pathogenic bacteria in the colon and less lactobacillus and bifidobacterium species. The idea behind providing probiotics to neonates would therefore be to repopulate the intestine of these vulnerable infants with good bacteria and potentially reduce the incidence of a devastating condition like NEC.
If only it were that easy though. The issue of using Probiotics in preterm infants is a contentious one to say the least. While the evidence appears to indicate an overall benefit in terms of reducing rates of NEC there remain concerns regarding the safety of providing bacteria to this population even though the bacteria are thought to be beneficial. The people who urge caution in the use of probiotics say so due to a few reports of sepsis after the introduction of probiotics with the organism that the patient was provided or with a different species that was could be traced to a contaminated product. In fact the contamination need not be with bacteria as was found in 2014 when Rhizopus oryzae was found in a commonly used product as was described in the Forbes article here. What made this case garner widespread media attention was that the infant died and justifiably led people to start asking questions about safety.
How Certain Are We of The Quality of the Products?
As I mentioned in another post on Facebook and Twitter recently, these products fall under the category of a nutritional product rather than a medication with Health Canada and therefore are not subject to the same rigorous quality control standards as other comparable medications would be.
An additional challenge (emanating from the lack of rigorous quality control demanded by a product deemed a drug) is the certainty that what you believe you are administering is actually in the product on the label. I demonstrated above how there can be contaminants but shouldn’t the product actually have at least the bacteria that is on the bottle as well? The majority of probiotics destined for human consumption are meant to contain lactobacillus and/or bifidobacterium. The question however is whether they actually do when independent analysis is performed. Sadly independent studies have confirmed that this may not be the case. A 2004 study by Szajewska and colleagues found that only 3/5 products tests contained the bacteria that were labelled on the bottle. Similarly Toscano et al in 2013 examined products in the European market to determine quality. Interestingly a decade later their findings were the same in that 58% of 24 products contained what they claimed. Clearly just because it says it contains these bacteria on the bottle doesn’t necessarily mean that.
Hard To Argue About Sepsis?
Taking all of this theoretical concern into consideration, one has to acknowledge an additional and very important finding from a
recent systematic review. In a pooled analysis of 25 studies on the use of probiotics the risk of sepsis was reduced in the following manner:
1. risk of any sepsis (25 RCTs; RR 0.83, 95% CI 0.73-0.94; I = 26%)
2. bacterial sepsis (11 RCTs; RR 0.82, 95% CI 0.71-0.95; I = 0%),
3. fungal sepsis (6 RCTs; RR 0.57, 95% CI 0.41-0.78; I = 0%)
4. This beneficial effect remains in very low birth weight infants (<1500 g) (19 RCTs; RR 0.86, 95% CI 0.75-0.97; I = 18%), but not in extremely low birth weight infants (<1000 g) (3 RCTs; RR 0.73, 95% CI 0.45-1.19; I = 53%).
A reduction in sepsis is not anything to take lightly. Late onset sepsis in the NICU can be very damaging and may predict poorer development at 18 months and beyond. In this study, despite the aforementioned concerns regarding potential infection with the organism provided no such infections occurred.
Despite all the possible benefits, in the NICU much attention has moved towards donor milk and moreover establishing exclusive human milk diets. With this changing landscape the beneficial effects of probiotics may decrease over time. Given that the goal of probiotics is to change the microbiome to one that is closer to a breastfed infant will this still be needed? What we will need for sure is a repeating of trials in units that have high rates of human milk exposure to know for sure.
Whether to use probiotics or not becomes a tough question to answer and would be primarily based on your sense of trust in the quality control of the products at the moment I would think. The benefits appear to be real but the question is, are you willing to take the risk?

by All Things Neonatal | Sep 8, 2015 | Neonatal, Neonatology, Prematurity
My friend Nick Hall asked a very important question on Linkedin today in the following post
Nick is a tremendous advocate for premature infants and their families everywhere and as President and Co-Founder of Graham’s Foundation certainly puts himself front and centre. For more information on the incredible work he and his team are doing please see their website at and if you are in the New York area please consider attending their charity benefit to help raise some funds to continue the work that they do.
As it pertains to his question though it did get me thinking. How does a National body like the AAP determine best practice suggestions for a country with 50 states in which roughly 320 million people reside? Using 2013 USA census data ,showing 23.1% of it’s citizens are under 18 this equates to nearly 74 million children. This is a daunting task no doubt and due to regional variation in terms of expertise and available resources not all policies or guidelines are possible to implement equally or at all.
The article that is being addressed in his question of the day is from Med City News which addresses the latest statement from the AAP on managing an anticipated birth before 25 weeks. For the actual statement that the article refers to please see this link which will direct you to the actual paper.
When the Canadian Pediatric Society (CPS) reaffirmed their statement in January 2015 it drew a fair bit of criticism from Canadian Neonatologists and others from abroad due to it’s draconian approach to infants at 22 and 23 weeks gestation. In the CPS statement the following was written in the recommendations section with respect to these two gestational ages which also encompassed 24 weeks as well.
“At 22 weeks’ GA since survival is uncommon, a non-interventional approach is recommended with focus on comfort care”
“At 23 and 24 weeks’ GA active treatment is appropriate for some infants”
What drew the ire of these health care providers was the apparent limitation of resuscitation based on gestational age. It did not seem that consideration was being given to potential inaccuracies with gestational age dating which at best in the first trimester are +/- a few days and in the second trimester may be off up to 1-2 weeks. Furthermore no mention was made of accounting for other factors such as the findings on an ultrasound which if very discrepant might suggest an older fetus or perhaps equally important the wishes of the parents. What were their past experiences, religious beliefs or lengths to which they had tried for this pregnancy. The 16 year old single mother who conceived via rape might be expected to have a vastly different perspective than the mother at 43 who has tried 5 rounds of IVF and has finally conceived her first baby. Many of these points were highlighted in a response by a large group of care providers in a paper entitled “CPS position statement for prenatal counselling before a premature birth: Simple rules for complicated decisions.”
Now we have a new statement from the American Academy of Pediatrics which I have to complement as it addresses a number of concerns that the above group had with the Canadian version.
1. Fetal gestational age, as currently estimated, is an imprecise predictor of neonatal survival, but 22 weeks of gestation is generally accepted as the lower threshold of viability.
2. Although most infants delivered between 22 and 24 weeks’ gestation will die in the neonatal period or have significant long-term neurodevelopmental morbidity, outcomes in individual cases are difficult to predict.
3. Outcomes of infants delivered at 22 to 24 weeks of gestation vary significantly from center to center.
4. Because of the uncertain outcomes for infants born at 22 to 24 weeks’ gestation, it is reasonable that decision-making regarding the delivery room management be individualized and family centered, taking into account known fetal and maternal conditions and risk factors as well as parental beliefs regarding the best interest of the child.
The first four points address the issues of uncertainty in dates, variable outcomes and the importance of taking a family centred approach. On the surface this seems like the perfect statement but I have highlighted the third point as it really gets to what Nick Hall is referring to (or at least my interpretation). We know that there is a great variability in outcomes from 22-26 weeks across the US based on the recent study by Rysavy et al. In this study which involved 24 hospitals with tertiary care centres, the median survival across all hospitals at 22 weeks (who actively resuscitated infants) ranged from 0 – 14.6% and at 23 weeks 23.8 – 37.1%. Imagine you are a parent at a centre that has a zero percent survival rate at 22 weeks. Should the hospital inform you of that and if after hearing that you still want “everything done” should the Neonatal team resuscitate your infant? There is no doubt that the parental wishes as outlined in point 4 are important but I would counter that there is also little point in putting a family through a futile exercise.
Vince Lombardi the former head coach of the Green Bay Packers produced the following quote that has been used many times since his heyday in the 1960s. “Practice does not make perfect. Only perfect practice makes perfect” 
This could not be more applicable to the situation in many centres thoughout the US. Resuscitating 22 and 23 week infants can be done and in a manner of speaking is a form of practice. Should centres though who have not “perfected” their approach by having rigorous audits of their practice, a “golden hour” approach and lastly the best equipment for resuscitation continue to offer families who wish to “do everything” just that? I would say no. While the AAP certainly endorses this type of approach centres need to be honest and disclose their success with such resuscitations. If you have zero survivors and know that there is a non standard approach at delivery of such patients and substandard equipment such as the absence of blenders to allow less than 100% O2 resuscitation do you not have a moral and ethical obligation to draw the line and say no?
The AAP offers the best approach to resuscitation from 22-25 weeks that I have seen but I don’t believe it is for every centre at the moment. Only those centres who believe that they have all the infrastructure and processes in place to achieve “perfect practice” should be routinely resuscitating infants at 22 and 23 weeks. To continue to offer these families everything and perform less than perfect practice will not lead to any improvements in their rate of success and do the families that come to their hospitals a disservice.
The first step in medicine is to pledge to do no harm. I would hope that hospitals would be honest with themselves and if they don’t have everything in place to achieve great results will spare families the experience of false hope when the only outcome will be the inevitable loss of a child.



 Locally we have seen expansion of rural sites that can connect with us and a strong desire by existing sites to connect via telehealth for a variety of reasons. While the thrust of the program was to deliver advice to rural practitioners and support our level I and II units we have found such support leading to possibilities we had not dreamed of. Initial discussions via telehealth and in person have occurred examining whether such treatments as CPAP stabilization and NG feedings could be done in these sites. Being able to provide such care will no doubt lead to more stable infants being transported to our site and moreover the possibility of moving the care for infants needing only gavage feeding back to their home communities. Who knows what the future will hold for us as we also look forward to the hiring of a telehealth coordinator for NICU!
Locally we have seen expansion of rural sites that can connect with us and a strong desire by existing sites to connect via telehealth for a variety of reasons. While the thrust of the program was to deliver advice to rural practitioners and support our level I and II units we have found such support leading to possibilities we had not dreamed of. Initial discussions via telehealth and in person have occurred examining whether such treatments as CPAP stabilization and NG feedings could be done in these sites. Being able to provide such care will no doubt lead to more stable infants being transported to our site and moreover the possibility of moving the care for infants needing only gavage feeding back to their home communities. Who knows what the future will hold for us as we also look forward to the hiring of a telehealth coordinator for NICU!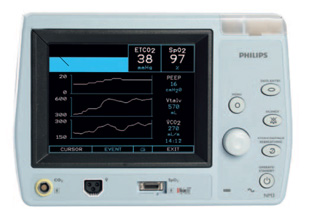 Since writing this piece we have tried it on several babies by using a double lumen tube and found the results to be as accurate as described in the Israeli papers. In practice though, secretions have proved difficult to handle for longer periods of use as they can travel up the sampling lines and damage the filters in the analyzers. A costly issue to deal with that we are currently trying to solve. Being able to continuously sample CO2 and adjust ventilation without drawing frequent blood gases is somewhat of a dream for me and we will continue to see how we can go about making this an established practice but there is work to be done!
Since writing this piece we have tried it on several babies by using a double lumen tube and found the results to be as accurate as described in the Israeli papers. In practice though, secretions have proved difficult to handle for longer periods of use as they can travel up the sampling lines and damage the filters in the analyzers. A costly issue to deal with that we are currently trying to solve. Being able to continuously sample CO2 and adjust ventilation without drawing frequent blood gases is somewhat of a dream for me and we will continue to see how we can go about making this an established practice but there is work to be done! The first is that through a generous donation and the blessing of our health region we have been able to expand the use of donor breast milk from < 1250g for a two week period to < 1500g for a one month period. This wonderful change came about after much effort and was celebrated in December as we not only expanded the eligibility criteria but partnered with the NorthernStar Mother’s Milk Bank to provide donor milk to Manitobans (
The first is that through a generous donation and the blessing of our health region we have been able to expand the use of donor breast milk from < 1250g for a two week period to < 1500g for a one month period. This wonderful change came about after much effort and was celebrated in December as we not only expanded the eligibility criteria but partnered with the NorthernStar Mother’s Milk Bank to provide donor milk to Manitobans ( The change took almost a year to roll out and could not have been done without a massive educational rollout that so many people (a special thank you to our nurse educators!) took part in. Looking back on the year we have now seen several infants at 23 weeks who survived with a small minority dying in the newborn period. It is too early to look at long term outcomes but I think many of us have been surprised with just how well many of these children have done. Moreover I believe we may be seeing a “creep effect” at work as the outcomes of infants under 29 weeks have also improved as we developed new guidelines to provide the best care possible to these vulnerable infants. Antenatal steroid use is up, IVH down and at least from January to September of last year no infants died at HSC under 29 weeks! I look forward to seeing our results in the future and cannot tell you how impressed I am with how our entire team came together to make this all happen!
The change took almost a year to roll out and could not have been done without a massive educational rollout that so many people (a special thank you to our nurse educators!) took part in. Looking back on the year we have now seen several infants at 23 weeks who survived with a small minority dying in the newborn period. It is too early to look at long term outcomes but I think many of us have been surprised with just how well many of these children have done. Moreover I believe we may be seeing a “creep effect” at work as the outcomes of infants under 29 weeks have also improved as we developed new guidelines to provide the best care possible to these vulnerable infants. Antenatal steroid use is up, IVH down and at least from January to September of last year no infants died at HSC under 29 weeks! I look forward to seeing our results in the future and cannot tell you how impressed I am with how our entire team came together to make this all happen!

 In April of 2015
In April of 2015  This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.
This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.