When it comes to non-invasive ventilation the field has become a little more crowded in recent years at least in our institution. In the recent past if one decided to extubate an ELGAN the biggest decision was what CPAP pressure to use. These days we have the option of high frequency nasal ventilation (nHFOV) or non-invasive positive pressure ventilation (NIPPV) to choose from as additional options. Both of these modalities have their uses and I have written about nHFOV before as in Nasal High Frequency Oscillatory Ventilation For Preventing Intubation. On this post though I want to look at NIPPV which has actually been around longer as a modality. The gist of this mode is that one chooses a delta P, peep, Ti and rate much like you would on a conventional ventilator. When ventilating through a nasal interface the device provides ventilation although it is questionable I suppose how much of that is alveolar ventilation. The study we are going to talk about here caught my eye as the information gleaned from it gives me at least an idea of how this mode may work to help prevent reintubations.
The Effect of Rate in NIPPV
Authors from Haifa, Israel performed a fairly elegant study entitled The effect of changing respiratory rate settings on CO2 levels during nasal intermittent positive pressure ventilation (NIPPV) in premature infants.
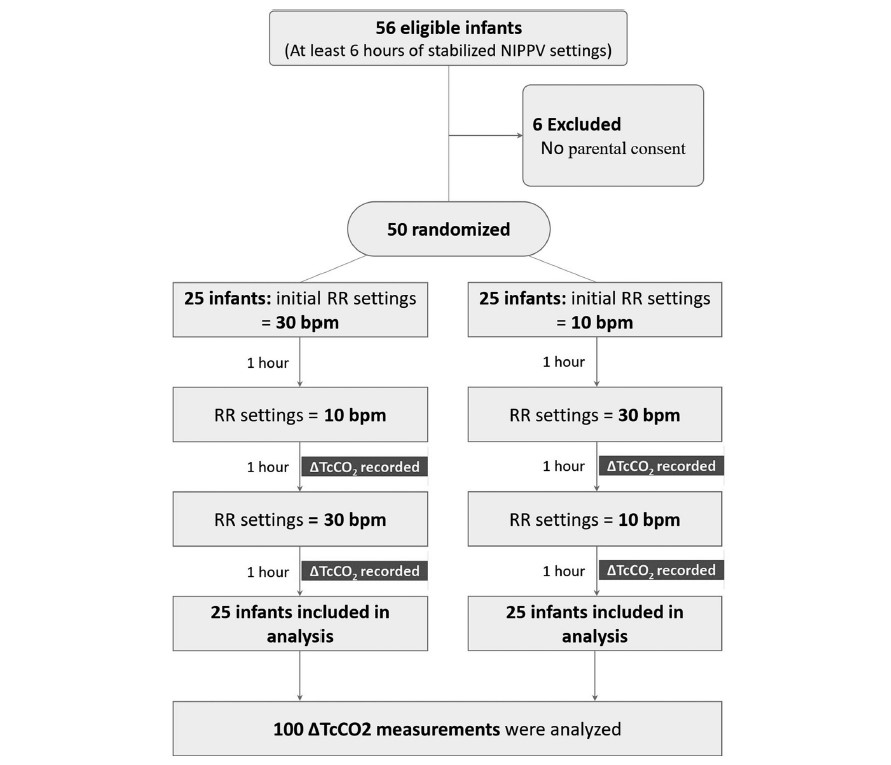
In this study each patient served as their own control and alternated between either a start of a rate of 10 BPM or a rate of 30 BPM as shown in the following diagram. The infants were all between 24 +0 and 32 +6 weeks gestation to be included in the study. Delivery of NIPPV was through the Leoni Ventilator using RAM cannulae and importantly the mode was non-synchronized. Each infant needed to be stable on their settings for at least 6 hours before being included. The authors hypothesis was that rate matters to clear carbon dioxide. To monitor CO2 levels they used transcutaneous CO2 measurements to allow for continuous measurement over each hour of the study. Given this belief, there was safety built into the protocol such that patients were excluded if on the set rate of 10 bpm the tcCO2-related pCO2 was <40 mmHg, or on NIPPV if the set rate of 30 bpm had a tcCO2-related-pCO2 is 60 mmHg, In other words, if rate matters and your tcCO2 was already less than 40 on a low rate then it would not be safe to blow off more CO2 and vice versa with high CO2 and low rates. To ensure that only rate affected the results “during the 3 h of the study no changes in PIP, PEEP or FiO2 were allowed
with the following exceptions: if spO2 was <90% or >95% for more than
20 s, an increase or decrease in FiO2 were allowed to keep spO2 90–94%,
and were documented”.
So does rate matter?
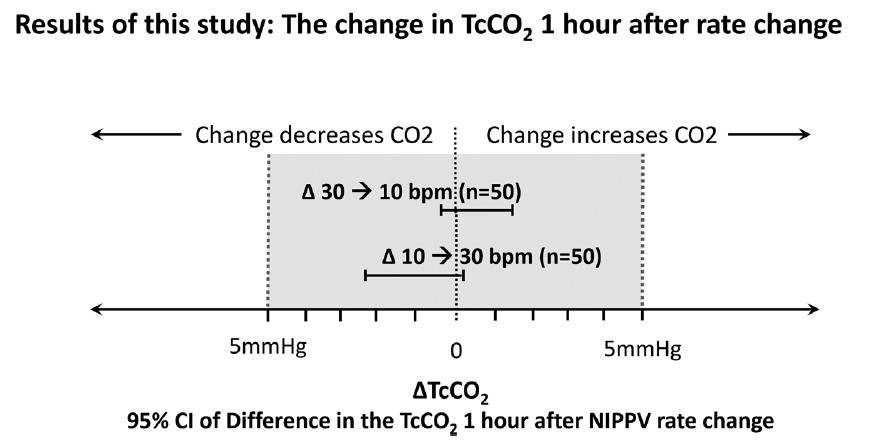
It turns out the authors found no difference in CO2 levels based on rate changes alone.
This of course is contrary to what the authors expected to find. The question is why this might be. What follows now is just speculation on my part but given the finding of no difference I can offer a few thoughts. The first is that NIPPV does not involve a distal delivery of gas like the situation of an endotracheal tube near the carina. With an endotracheal tube in place the delta P or pressure above the set peep is delivered to the gas exchanging areas of the lung. With NIPPV you are delivering the pressure at the nose and therefore there is a fair amount of dead space in between the exit of the gas into the baby and the lung. Might you just be really ventilating dead space for the most part?
Secondly, depending on the fit of the mask or the degree that the mouth was open how do we know how much of the non-invasive ventilation reached the infant? Lastly, in our own centre we have not been impressed with the RAM cannulae as we have found that whether the prongs are in or out of the nose the pressure being detected as being delivered seems to stay the same at least as the ventilator sees it. If the prongs were not in the nose properly and the atmosphere was being ventilated would one really know that the pressures weren’t really getting into the nose?
Lastly, the Leoni ventilator is not capable of delivering synchronized NIPPV. Now that there is the availability of synchronization on ventilators such as on the Puritan Bennett 980 ventilator it would be interesting to see the same study done again. If you are delivering non-synchronized breaths which are not in sync with the patient should we expect a change in CO2? What if half the breaths for example by chance are delivered on exhalation? Not much effect on CO2 I would think.
I am not saying that rate doesn’t matter at all but I suppose I am saying within the context of this study it doesn’t matter to CO2. My best guess as to how NIPPV works to prevent reintubation may be secondary to two things. The first would be by irritating the baby with the puffs of delta P. Think of it like intermittent stimulation. The second possibility is that the same puffs of air help keep the pharynx open and minimizes the obstructive portion of apnea of prematurity. Whatever the reason NIPPV appears to work to prevent reintubation in some infants!
I have no doubt the group here will look at the effect of delta P on CO2 soon enough and I wonder if we will see much difference there either. It also will be important to look at the effect of rate in a synchronized fashion! Time will tell.


Thank you for sharing. I have been a NICU nurse for 40 years, and will retire in September for health reasons. I will continue to follow your articles and share them with nurses I’ve taught over the years!