I had the opportunity recently to give a talk on strategies to reduce BPD in our preemie population. For the talk, I used as a springboard the recommendations for reducing BPD as laid out by the Evidence Based Practice for Improving Quality (EPIQ) group. There are far too many recommendations for optimal care to go through but the point of this post is to highlight one strategy that I think is deserving of discussion.
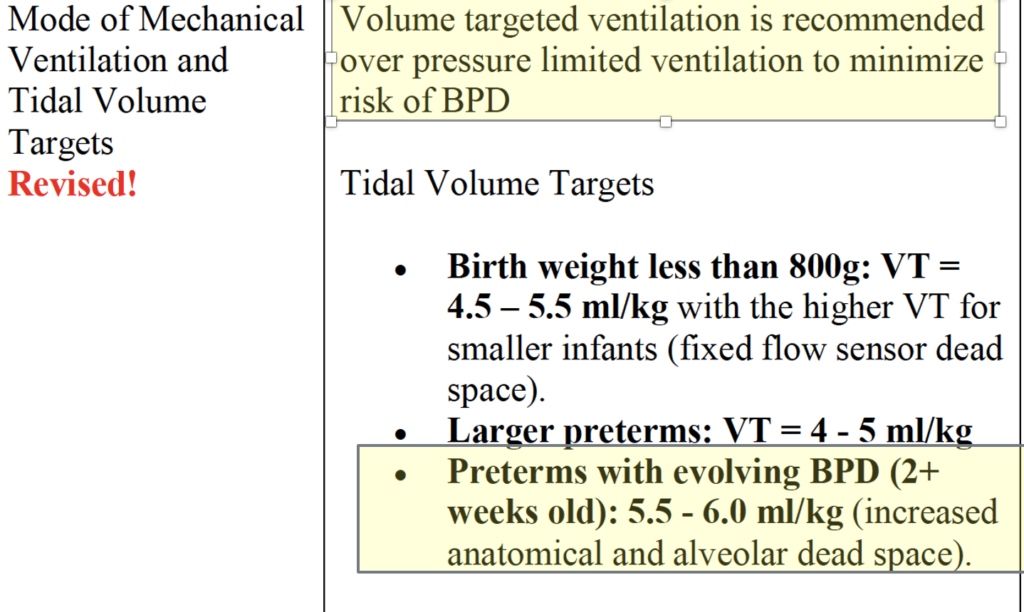
That volume targeted ventilation is recommended is no surprise. Setting a desired volume and allowing pressures to fluctuate rather than fixing a pressure and allowing volumes to fluctuate reduces the risk of both atelectotrauma and volutrauma. A recent paper Early volume targeted ventilation in preterm infants born at 22-25 weeks of gestational age has added further arguments in those at the smallest gestational ages by reducing episodes of hypocapnia and increasing likelihood of extubation by 24 hours compared to those on pressure limited ventilation.
Are Bigger Volumes Better With Time?
It is the second highlighted piece above that has left me scratching my head. Going way back to my residency I was taught that the ideal tidal volume is somewhere between 3.5 – 4.5 mL/kg and we should try and keep PIPs less than 35 cm H2O as an absolute maximum. In reality we typically would switch to the high frequency jet ventilator if pressures were increasing above 25 cm H2O in an effort to avoid volutrauma by increasing volumes further or barotrauma from excessive pressure. The main thrust of the argument was that big volumes hurt the lung so one is better off being gentle and inflating the lung with PEEP and then using the more gentle pulse of the HFJV after that. To be sure in the early stages of the neonatal course excessive volumes and pressure can commit the patient to a significant risk of BPD and meticulous attention to respiratory care is needed. The question for today is whether after 2 or 3 weeks of age, babies with developing lung injury need more volume on conventional ventilation or whether continuing on the HFJV is the way to go. I will let you in on a secret right away though. There is a systematic review on the subject.
The problem is it only includes one study from 1991 which is before antenatal steroids and surfactant as standards of care so not much to take from this paper.
Evidence for Bigger Volumes
The first paper showing some evidence for this is by Kezler M et al from 2009 Evolution of tidal volume requirement during the first 3 weeks of life in infants <800 g ventilated with Volume Guarantee. The study examined 26 infants with blood gas and Vt sets (828 in total). The Vt measurements included in the analysis were only those that were used when the blood gas was within a normal range for age using permissive hypercapnia to guide treatment.
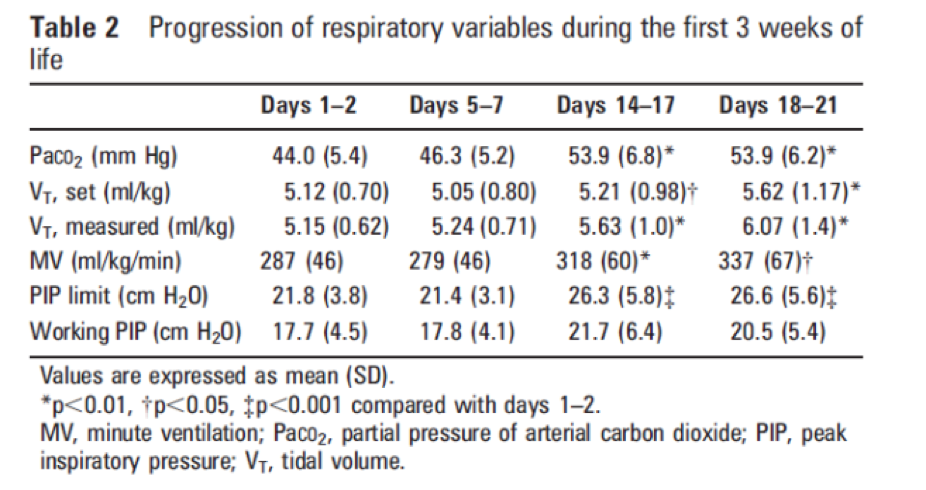
As shown in the table above the needed tidal volumes rise over time. The PIPs remain acceptable (below the set limits) but the volumes rise to close to 6 mL/kg by three weeks of age. If these results are generalizable to our own population this would mean that using our units current levels of 3.5 – 4.5 mL/kg would leave these older infants short. If so is it any wonder we see high pCO2 triggering a need for HFJV. The authors conclude here that the progressive dilation of the trachea and proximal bronchi over time from ventilation increase dead space and are responsible for the rise in needed Vt.
The next study Volume targeting levels and work of breathing in infants with evolving or established bronchopulmonary dysplasia was published in 2019 by Hunt et al. This study looked at 18 infants less than 32 weeks and randomly assigned them once older than one week of age and still ventilated to 20 minute periods on 4,5,6 and 7 mL/kg of Vt in random fashion. The median GA was 26 weeks and day of study 18 days. The outcome of interest was measurement of work of breathing using the Pressure-time product of the diaphragm (PTPdi). The findings are below.
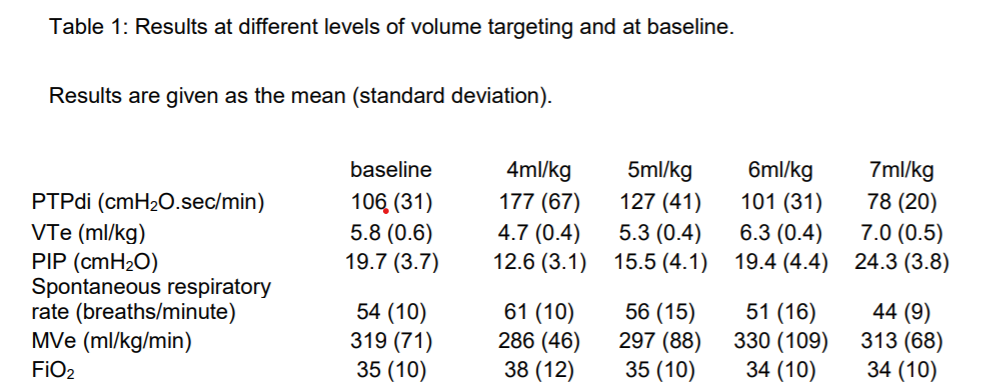
One did not see a significant improvement in work of breathing until 7 mL/kg was reached and you can see a progressive rise in minute ventilation needed to maintain normocapnia over time. This study supports the previous one in suggesting that over time there is an increase in dead space and if we want to reduce air hunger which could be represented by work of breathing we need to consider higher volumes.
The Damage is Done
Its an imperfect science that we are looking at and there is no doubt there will be readers of this post that will cringe at the volumes being discussed. I think what this really comes down to is whether you think the damage is done by 2-3 weeks. We of course don’t officially classify babies as having BPD until 36 weeks but if we are being honest we often know or can predict which ones are destined to get it. Is it better for the babies to be put on high frequency ventilation for weeks or to be given some larger volumes on conventional ventilation? Hard to say based on the evidence as there really isn’t much to go by. One thing that does need to be considered is long term high frequency ventilation and the need for sedation. Many of our kids on weeks of such therapy need progressively more sedation and what effect does that have on the developing brain. On the other hand if excessive volumes even at 2-3 weeks lead to increased damage to the lungs are you risking a prolongation on the ventilator or increasing the need at some point for a tracheostomy?
In the end I don’t think at the moment anyone knows. If you move from one center to another though and see completely different approaches I hope that by reading this post you will at least understand where the differences in practice come from.
In the end we are all just trying to do what we believe is best for the baby.

