One of the most common conditions afflicting ex-preterm infants is chronic lung disease. Through advances in antenatal steroids, surfactant and modern ventilation we have done what we can to try and prevent this condition from occurring yet despite our best efforts CLD remains a common problem among those born at less than 1500g as is shown in the 2018 Canadian Neonatal Network data.
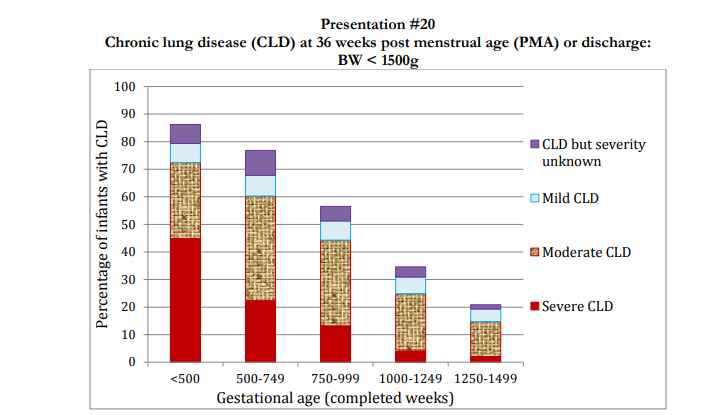
Primary prevention is of course the ideal strategy to reduce disease but when you try and your best and an infant still has chronic lung disease what is one to do? For now we bide our time focusing on nutrition and minimizing harm from ventilation. Something new is coming and I hope it comes soon.
Stem Cells to Heal BPD
My former colleague Bernard Thebaud has done much work already in this field. A recent review he was part of is a good starting point to bring you up to speed; Stem cell therapy for preventing neonatal diseases in the 21st century: Current understanding and challenges. As the field advances though and we continue to see additional animal trials such as the one I will discuss here, the interest in this field continues to grow. I was drawn to a recent paper on this topic as it is not dissimilar to another trial I wrote about in which stem cells were given via breastmilk intranasally to improve outcome after IVH; Can intranasal application of breastmilk cure severe IVH? In this new trial though instead of delivering stem cells in a cephalad direction they place the rat vertically to deliver the stem cells from wharton’s jelly to the trachea and damaged lung.
Stem cells from Wharton’s Jelly
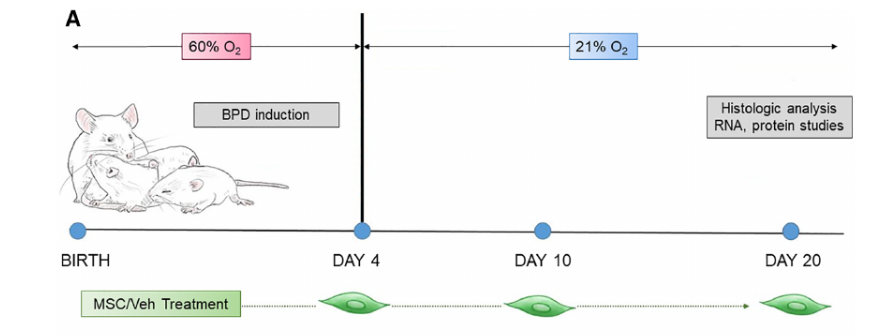
Moreira A et al published the following paper in Intranasal delivery of human umbilical cord Wharton’s jelly mesenchymal stromal cells restores lung alveolarization and vascularization in experimental bronchopulmonary dysplasia This study was done in four rats divided into 4 groups. Group A were rats born and raised in room air. Group B were exposed to 60% oxygen for four days to induce BPD. Group C was given experimental BPD as in Group B and then given the vehicle for stem cell delivery without stem cells. Group D then also had BPD was actually given stem cells. The timeline for the study is shown below.
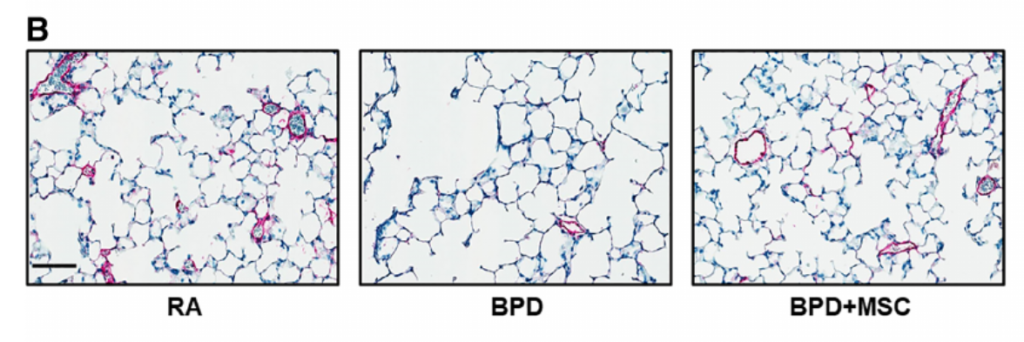
The results are quite impressive. Looking at the histology of the four different groups reveals the curative property of these types of cells.
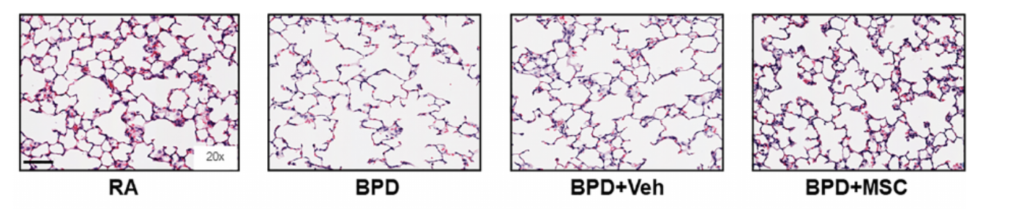
In essence the lung tissue architecture at the alveolar level looks almost identical to normal rat lung on the far left if the stem cells are provided through the intranasal route.
Moreover, when one looks at the impact on the blood vessels in the lung using Von Willebrand Factor staining similar healing is observed.
Lastly, not only were the numbers of blood vessels recovered but the thickness of the smooth muscle was reduced to that of normal rats without BPD after such treatment.
Why is this so important?
Past research has delivered stem cell treatment to the alveoli through an endotracheal tube. What this demonstrates is that rats held in a vertical position can have stem cells delivered into the lung where they are sorely needed. Could one take an infant on CPAP who is developing signs of CLD and do the same? The day may be coming when we prevent such infants from being reintubated just for CLD in the future.
The road is long though and the use of stem cells in humans has not begun yet. The effects seen in this rat model are dramatic but will they translate into the same thing in the human? I believe so and am waiting ever so patiently for such trials to start in humans. If you are looking for the next big leap in Neonatology I suspect this is what we are looking at. The question now is when.