If you work in Neonatology you talk about caffeine endlessly whether addressing your own consumption or that of your patients. Our unit like many others typically starts caffeine early in a prophylactic fashion for babies under 32 weeks. The reason for this is due to the high incidence of apnea (AOP) in this population. The incidence of AOP follows an inverse relationship with GA, affecting 50% of those born at 30 weeks versus 7% at 34-35 weeks. Using caffeine in a more therapeutic approach is certainly sensible for babies older than 32 weeks given the lower likelihood of events. People who argue for a prophylactic strategy cite lower incidence of BPD and PDA from the CAP study while those on the side of reserving treatment for those who really need it put more emphasis on potential adverse effects such as polyuria, tachycardia and electrolyte disturbances. I have already revealed my bias as our centre takes a prophylactic approach but the question is whether it is still right given that the CAP study was many years ago now. A new study emerged this week that was shared on Twitter and generated some interesting discussion. So interesting in fact that I thought there was no better place to discuss this paper than here.
Head to Head Comparison
Elmowafi M et al published Prophylactic versus therapeutic caffeine for apnea
of prematurity: a randomized controlled trial this month. This trial included 90 infants in the prophylactic arm (caffeine started < 72 hours of age) vs 91 in the therapeutic arm (only started in presence of apnea or if a baby needed mechanical ventilation and all infants were under 32 weeks of age at birth. Unfortunately, while the study was prospecitve it was not blinded although the authors state that in the therapeutic arm a neonatologist who was not part of the study team made the diagnosis of AOP. Caffeine dosing was standardized using the citrate form at 20 mg/kg as a load and with 10 mg/kg maintenance dosing (divide by 2 for base equivalents).
The primary outcome was total duration of oxygen support and a sample size was chosen based on a previous pilot RCT and the expectation that they could show a reduction in O2 requirement of 7 days in the prophylactic group. Looking at the baseline characteristics of the groups the only difference was the median day of starting caffeine which for the prophylactic group was day 1 and for therapeutic day 3.
Results
What happened in both groups and the reasons for starting caffeine are shown in teh following diagram.
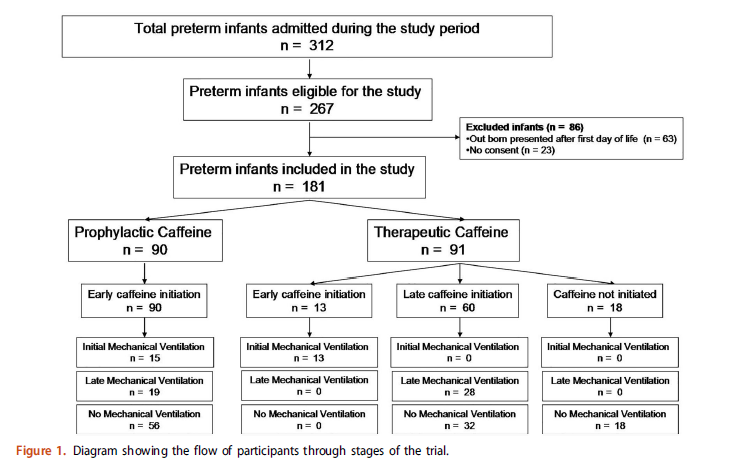
As you can see, 13 patients were started due to need for initial mechanical ventilation, 28 for late mechanical ventilation with the rest being apnea as a reason except for 18 patients who never needed caffeine. When looking at the whole patient population the primary outcome was no different between the groups using an intention to treat analysis.
What the authors did next is where the controversy comes from but has some interesting data nonetheless. They did a “per-protocol analysis” on the whole group and found the following:
Per protocol analysis showed that prophylactic caffeine therapy was associated with a significant reduction in the duration of oxygen therapy compared to therapeutic initiation among included preterm infants [median and IQR of 28 (18–36) days versus 34 (23–51) days, p¼.005 respectively].
Essentially what this means is they said let’s exclude those babies who never needed caffeine and just compare babies that all received caffeine in either arm. Now they see a difference of 6 days which is pretty close to the 7 days expected . Purests will note though that by doing so you can’t claim that the groups were balanced in terms of risk factors since the presented baseline characteristics are not necessarily still the same.
They went further though and asked the question. “What about a subgroup of <29 weeks?”. These babies are undoubedly higher risk for AOP and ventilation. Is the problem that the inclusion of babies 30-31 weeks diluted a potential benefit? Here is what they found.
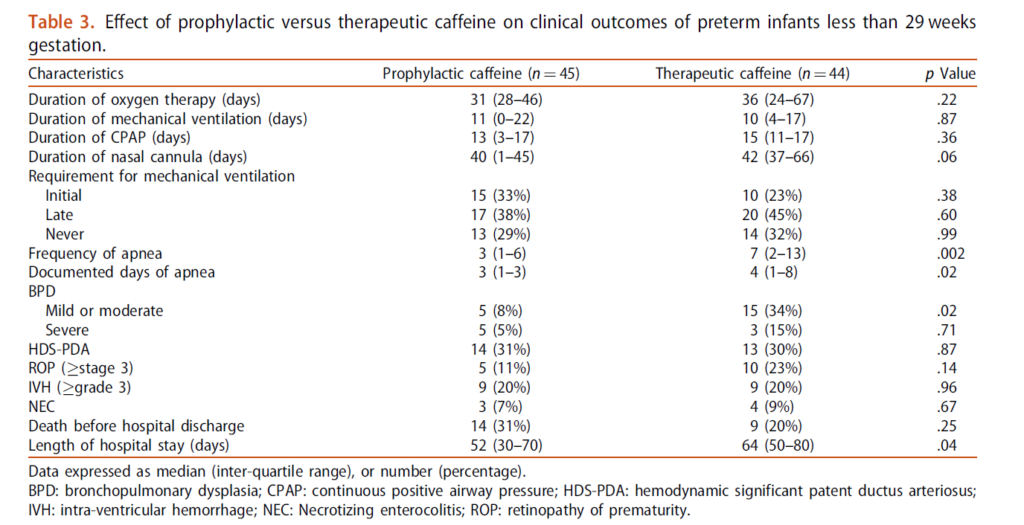
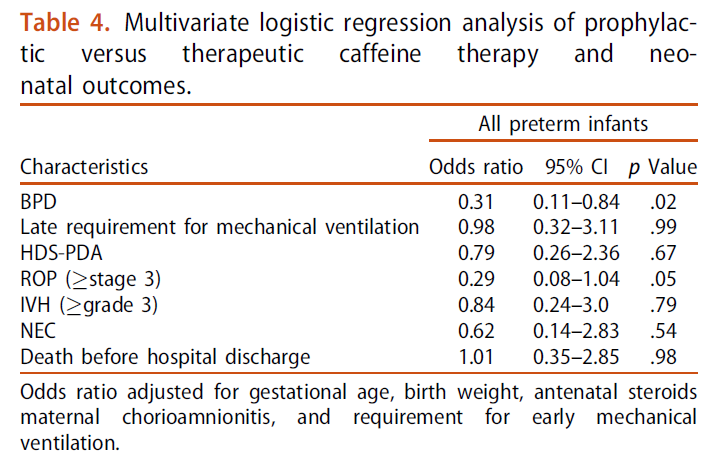
The main two things to draw your attention to are the marked reduction in mild to moderate BPD and shorter length of stay in hospital. Moreover when they looked at risk of BPD for the whole group they found a reduction in risk. Importantly there was no difference in adverse effects from caffeine use in either arm of concern.
What Can We Take From This?
Any discussion about adverse effects needs to acknowledge that these are short term outcomes we are looking at. Do babies who have never received caffeine do better in the long run? The CAP study did not suggest that was the case but it was a different time with different babies. Do I think caffeine is harmful? No I don’t, especially in the babies who would otherwise experience multiple apneic events or prolonged ventilation.
What this study does raise in my mind though is whether a change in approach to prophylactic caffeine is warranted. The authors don’t specify (I don’t think) but I suspect the bulk of the babies who did not need caffeine were in the 30-31 week group. We know that positive pressure ventilation is harmful to the developing preterm lung. Providing caffeine in the first few hours of life in the hopes of avoiding invasive ventilation or shortening the course of ventilation is the main reason that we likely see consistent reductions in BPD with its use. Under 29 weeks I would certainly favour giving caffeine early but above that as the risk of BPD drops considerably is a watch a wait approach a reasonable one to take? As this study was unblinded it is possible the babies were treated differently with respect to ventilation and apnea managment but I do think the risk is low. If the attendings caring for the babies were not part of the study and knew they were free to give caffeine if needed there may be less risk of bias.
In the end the results of this study in essence are supportive of my practice. I suspect they support many others as well. To answer the question really about side effects I suspect we would need much larger sample sizes than this with adequate power to detect differences but for now I will continue to say “give it and give it early!”

