I recall the shock waves through the neonatal community when ILCOR changed its recommendation to stop routine intubation of non-vigorous infants born through meconium. The rationale again was that for most practitioners it would be better to give bag valve mask ventilation and establish a functional residual capacity than try and intubate and start with a collapsed lung.
Oommen VI et al wrote a brief report on their experience in the UK with the change as recommended for these infants. Their brief publication has a large cohort that is looked at and one result in particular I found interesting enough to share with you today. The publication is Resuscitation of non-vigorous neonates born through meconium-stained amniotic fluid: post policy change impact analysis. The authors looked prospectively at the “new approach” group from October 2016-September 2017 and compared their outcomes to the retrospecitve cohort in the same hospital from August 2015-July 2016 as the “old approach” group.
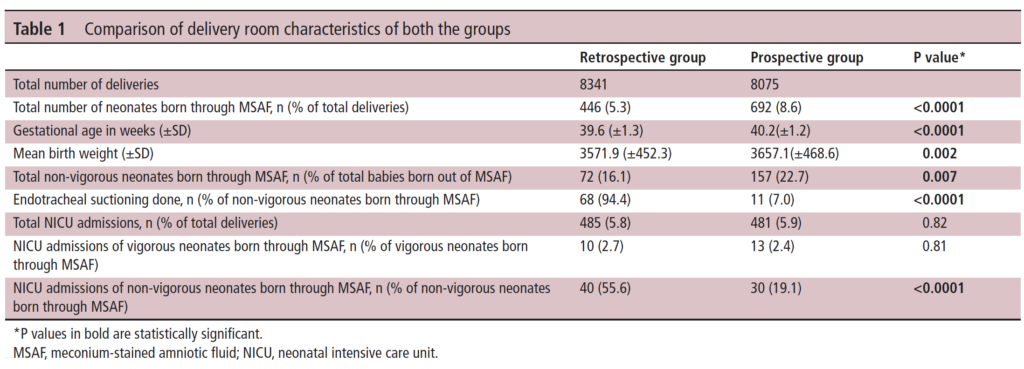
As you can see in Table 1 they saw a lot of deliveries during this time that were complicated by meconium. This gives us a good before and after comparison and while not all prospective and ensuring that practices were otherwise the same it is a pretty decent sample to look at. I like seeing that 7% of the group in the new approach still received endotracheal suctioning. It is worth remembering that what the recommendation says is to not do this routinely but if the resuscitation is not going well and the baby not responding to ventilation it is reasonable to apply suctioning as they would have done to see if there is any obstructive material in the airway.
It is the last comparison in Table 1 though that drew my attention. Over 50% of the non-vigorous babies needing routine suctioning in the retrospective arm needed NICU admission compared to 19.1% of the new approach group which was quite significant. More on this later.
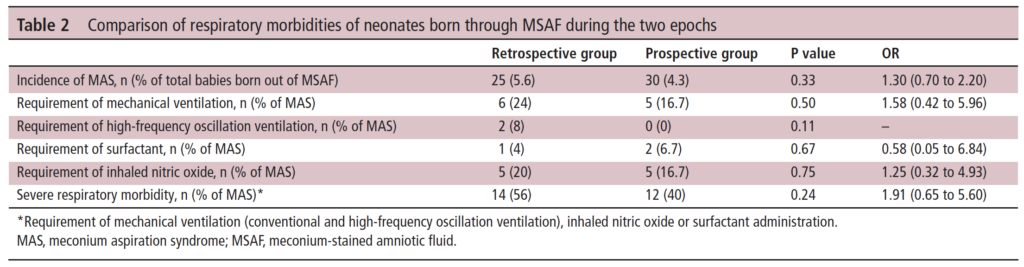
In Table 2 the authors compare the respiratory morbidities showing no difference in rates of ventilation, HFOV, surfactant or iNO. What they are demonstrating is that to the best of their abilities the babies were similar in terms of respiratory morbidiites in a binary sense. What I mean here is that when you ask the question did they need any of these aforementioned things it is a yes or no. What is not easy to pick up from the table is the quality of the respiratory disease. In the table they make it clear that severe respiratory disease was the same at 56% pre and 40% post and of course all of these babies would have needed admission. What we don’t know is what happened to the mild to moderate group.
A Theory
The whole point of giving PPV for the non-vigorous infant is to establish FRC. In the old approach it is conceivable that some of the infants could have lost volume during attempted intubation. The resultant delay in oxygenation could exacerabate any tendency to pulmonary hypertension. It could also turn a baby from one that could have had mild grunting to one that needed CPAP. Put another way it could have changed the outcome from a baby that needed observation and some prone positioning for a few hours to one that is committed to admission.
What these results show is basically what the intent of doing away with routine suctioning was supposed to do. The vast majority of severe disease in meconium aspiration syndrome is acquired in-utreo. Hypoxia and acidosis contribute to pulmonary hypertension while gasping respirations lead to inhalation of meconium deep into the airways. Suctioning after birth is not really going to help this cohort much. Providing positive pressure ventilation to the more mildly affected infants however may help open their lungs whereas delays in initiating would have the opposite effect.
In the end routine suctioning was a dogma that was in need of a challenge. The authors in the body of the paper go through other similar studies and in all but one the findings are similar. I commend the authors here for their humility as they do add at the end of the report all the potential shortcomings of the research. I for one don’t think it was necessary, as well designed research and thought went into taking down the dogma of routine suctioning. There is complete biological plausability for the findings presented here and I for one am glad to see that research in this case informed practice change that I believe was for the better.

