This past week I was very appreciative of efforts by readers on my Facebook page and Twitter accounts who were able to secure a copy of an article that really grabbed my attention. I could only go by the abstract at the time but the post suggesting that the use of azithromycin could reduce BPD garnered a lot of attention. Now that I have had a chance to read the paper I believe there are some very big caveats to that claim. What was done in this study I find very interesting and the results yield even more questions and make for what I think will be a great discussion.
A little history
BPD is known to be a condition that develops at least in part due to the effects of inflammation on the preterm lung. The combination of infections, inflammation from mechanical ventilation and the susceptibility of the developing tissue to damage make for a cocktail with a foul taste in the end. Previous work by Ballard HO et al in 2011 Use of azithromycin for the prevention of bronchopulmonary dysplasia in preterm infants: a randomized, double-blind, placebo controlled trial found that the risk of death or BPD at 36 weeks PMA was no different in an RCT using azithromycin 10 mg/kg/day for 7 days followed by 5 mg/kg/day for a maximum of 6 weeks. There was a suggestion in this study that in those with ureaplasma urealyticum there might be an affect. Researchers from Calgary had also published Azithromycin and Other Macrolides for
Prevention of Bronchopulmonary Dysplasia: A Systematic Review and Meta-Analysis which suggested prophylaxis helps with a NNT of 10 to reduce BPD. In spite of this it just hasn’t grabbed hold so maybe a new study would add some strength to the concept.
What was done this time around?
In the most recent paper by Nunes CR et al Use of Azithromycin for the Prevention of Lung Injury in Mechanically Ventilated Preterm Neonates: A Randomized Controlled Trial, the authors set out again to test the effect of azithromycin on modulating risk for BPD. They used the results of the Ballard trial to determine a number needed in their power calculation and came up with 38 per group and achieved 40 so they were powered to find a difference. They incuded all neonates who met inclusion criteria (invasive MV within 72 h of birth and, necessarily, invasive ventilatory support for, at least, 12 h until randomization) who were born under 1500g and randomized them to five days of azithromycin vs placebo. The strength of the study was that they also measured cytokine levels before starting azithromycin and then at 5 days after treatment. It is the outcome of interest that really puzzles me. They chose oxygen dependency at 28 days as their outcome of interest rather than 36 weeks PMA which is the more modern choice of end point for BPD. They also chose a much shorter course of 5 days compared to the study by Ballard which had previously shown no difference in outcome which I find odd as well. The baseline characteristics given that this was a small study also revealed an important difference between the two groups.
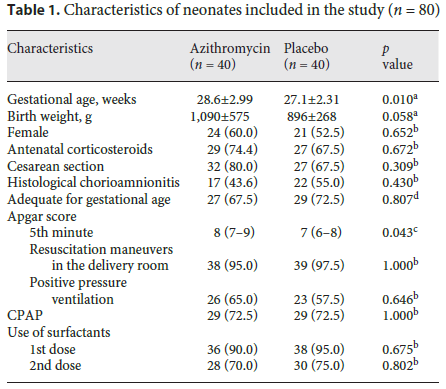
The babies in the treatment arm were on average 1.5 weeks more mature at birth which matters a great deal when you are alking about BPD. Additionally they were about 200g larger in size which was close to reaching statistical significance. Otherwise the infants were the same and the authors eventually control for these differences in the final analysis but to me at least this seems like a stark difference between groups favouring a higher expected risk of BPD from the outset regardless of treatment arm.
The main outcomes are where the authors lay claim to finding support for the intervention. At 28 days there was a statistically significant reduction in both oxygen dependency and oxygen dependency/death. As shown below though those differences did not extend to 36 weeks for either outcome.
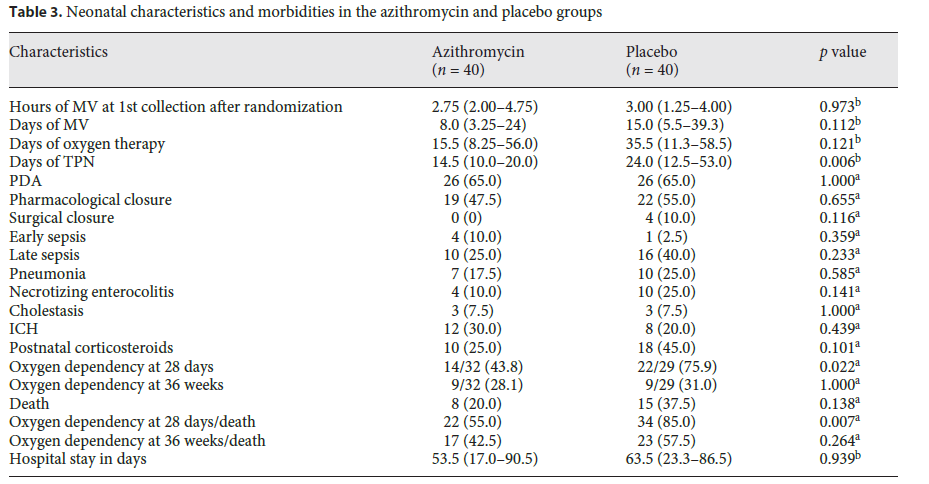
Not surprisingly there were other differences in the groups reflective of the younger patients in the placebo arm such as higher rates of postnatal steroid use and days of TPN. One strength I suppose here is that since both groups were exposed to mechanical ventilation durations that were not different when their cytokine profiles were checked the effect of invasive positive pressure might be similar between groups. What is not known however is the mean airway pressures between groups or for that matter if any were put on high frequency ventilation so we have quantity but not quality. One could postulate that while durations were similar over 5 days, the smaller and younger patients may have been exposed to much higher pressures and/or volumes which could of course influence degree of inflammation. Looking at the cytokine profiles is interesting nonetheless.
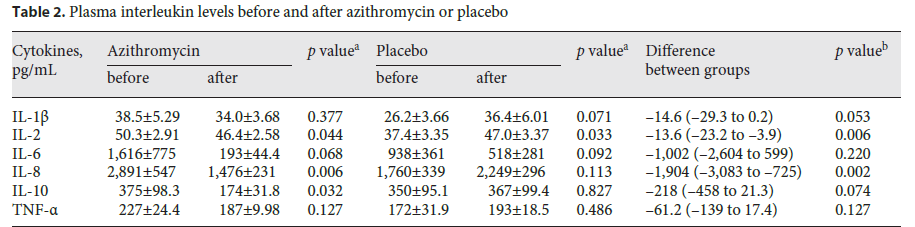
The cytokines IL-2 and 8 were found to be significantly lower in the treatment arm and in general all others at least trended in the same direction after completing treatment with azithromycin. With less inflammation it seems probable then that the reduction in need for O2 at 28 weeks might be real and after the autors controlled for such things as gestational age and weight the finding bore out but at 36 weeks (the more meaningful outcome) the difference was gone.
What can we take from the study
Am I ready to start azithromycin in all my infants under 1500g? Not yet. This study raises too many questions for this to become standard of care. It really troubles me that the authors here used a shorter duration of azithromycin than the Ballard study and then used a less meaningful outcome of 28 days to demonstrate their difference. While they did find a difference I am concerned that there is a bit of “smoke and mirrors” here in that there is a difference in an outcome that in todays world isn’t that meaningful. I cringe at saying this but what is really needed is a larger multicentre study in which hopefully the gestational ages and weights at the outset are balanced. Even if we didn’t see a big difference in outcome at 36 weeks for BPD I would wonder if the cytokine profiles showed similar trends whether other conditions such as ROP and PDAs which can also be influenced by inflammation would demonstrate a difference between groups. We need a larger sample size and balancing of factors such as tidal volumes and ventilator pressures though to answer this in a more conclusive manner.

