by All Things Neonatal | Apr 18, 2019 | BPD
Choosing to provide postnatal systemic steroids to preterm infants for treatment of evolving BPD has given many to pause before choosing to administer them. Ever since K Barrington published his systematic review The adverse neuro-developmental effects of postnatal steroids in the preterm infant: a systematic review of RCTs. and found a 186% increase in risk of CP among those who received these treatments, efforts have been made to minimize risk when these are given. Such efforts have included shortening the exposure from the length 42 day courses and also decreasing the cumulative dose of dexamethasone. Fortunately these efforts have led to findings that these two approaches have not been associated with adverse neurodevelopmental outcomes. Having said that, I doubt there is a Neonatologist that still doesn’t at least think about long term outcome when deciding to give dexamethasone. The systemic application certainly will have effects on the lung but the circulating steroid in the brain is what occupies our thoughts.
What About Applying it Directly to the Lung
If you wanted to prevent BPD the way to do it would be to minimize the time infants are exposed to positive pressure ventilation. Rather than giving steroids after a week or two maybe it would be best to give them early. Recent evidence supports this for systemic steroids and has been written about recently. Hydrocortisone after birth may benefit the smallest preemies the most! This still involves providing steroid systemically. Over the years, inhaled steroids have been tried as have intratracheal instillation of steroid with and without surfactant as a vehicle for distribution to the lung. This month colleagues of mine anchored by Dr. G. t’Jong  (a founding member of the “Tall Men of Pediatrics #TMOP) published a systematic review and meta-analysis of all such RCTs in their paper Efficacy and safety of pulmonary application of corticosteroids in preterm infants with respiratory distress syndrome: a systematic review and metaanalysis. The results of the study suggest that there may well be a role for this approach.
(a founding member of the “Tall Men of Pediatrics #TMOP) published a systematic review and meta-analysis of all such RCTs in their paper Efficacy and safety of pulmonary application of corticosteroids in preterm infants with respiratory distress syndrome: a systematic review and metaanalysis. The results of the study suggest that there may well be a role for this approach.
All of the included studies used a prophylactic approach of giving between the first 4 hours and the 14th day of postnatal age doses of pulmonary steroids with the goal of preventing death or BPD. The GA of enrolled infants ranged from 26 to 34 weeks, and the birth weight ranged from 801 to 1591 g. Out of 870 possible articles only 12 made the cut and compromised the data for the analysis.
Routes of steroid were by inhalation, liquid instillation though the endotracheal tube or by mixing in surfactant and administering through the ETT.
What Did They Find?
Using 36 weeks corrected age as a time point for BPD or death, the forrest plot demonstrated the following. A reduction in risk of BPD or death of 15% with a range of 24% to only a 4% reduction.

Looking at the method of administration though is where I find things get particularly interesting.

What this demonstrates is that how you give the steroids matters. If you use the inhalational or intratracheal instillation (without a vehicle to distribute the steroids) there is no benefit in reduction of BPD or death. If however you use a vehicle (in both Yeh studies it was surfactant) you find a significant reduction in this outcome. In fact if you just look at the studies by Yeh the reduction is 36% (CI 34 – 47%). In terms of reduction of risk these are big numbers. So big one needs to question if the numbers are real in the long run.
Why might this work though?
In the larger study by Yeh, budesonide was mixed with surfactant and delivered to intubated infants every 8 hours until FiO2 was less than 30%, they were extubated or a maximum of 6 doses were reached. We know that surfactant spreads throughout the lung very nicely so it stands to reason that the budesonide could have been delivered evenly throughout the lung. Compare this with inhalational steroid that most likely winds up on the plastic tubing or proximal airway. The anti-inflammatory nature of steroids should decrease damage in the distal airways offsetting the effects of positive pressure ventilation.
Future Directions
I am excited by these findings (if you couldn’t tell). What we don’t know though is whether the belief that the steroid stays in the lung is true. Are we just making ourselves feel better by believing that the steroid won’t be absorbed and move systemically. This needs to be tested and I believe results of such testing will be along in the near future.
Secondly, we need a bigger study or at least another to add to the body of research being done. Such a study will also need long term follow-up to determine if this strategy does at least have equal neurodevelopmental outcomes to the children who don’t receive steroid. The meta-analysis above does show in a handful of studies that long term outcome was no different but given the history of steroids here I suspect we will need exceptionally strong evidence to see this practice go mainstream.
What I do believe is whether you choose to use steroids prophylactically using hydrocortisone or using intratracheal surfactant delivered budesonide, we will see one or both of these strategies eventually utilized in NICUs before long.
by All Things Neonatal | Jan 30, 2019 | ventilation
InSurE (Intubate, Surfactant, Extubate) has been the standard approach for some time when it comes to treating RDS. Less Invasive Surfactant Administration (LISA) or Minimally Invasive Surfactant Administration (MIST) have been growing in popularity as an alternative technique. More than just popular, the techniques have been shown to reduce some important short term and possibly long term outcomes when used instead of the InSurE approach. Aldana-Aquirre et al published the most recent systematic review on the topic in Less invasive surfactant administration versus intubation for surfactant delivery in preterm infants with respiratory distress syndrome: a systematic review and meta-analysis. They demonstrated that when looking at 6 RCTs with 895 infants, the overall results indicate that use of LISA instead of InSurE leads to a lower rate of death or bronchopulmonary dysplasia (BPD) at 36 weeks (risk ratio (RR)=0.75 (95% CI 0.59 to 0.94), p=0.01) and the need for mechanical ventilation within 72 hours of birth (RR=0.71 (0.53 to 0.96), p=0.02) or anytime during the patient stay in the NICU (RR=0.66 (0.47 to 0.93), p=0.02). This study has been out for two years this month and yet here we are at least in my centre still performing InSurE.
Why is that?
One reason likely has something to do with the expression “you can’t teach an old dog new tricks”. We know how to do InSurE and we are pretty good at it. Performing the LISA technique is not just about putting a catheter in the airway and instilling surfactant. There are several steps that need to be done in order to ensure that the surfactant goes where it is supposed to so there is training required but such training is available in videos posted on the internet or I am sure available from centres willing to share their methods. Still it takes someone declaring we need to change before anything will happen. The second reason for this insistence on the status quo has been the availability of only a large volume surfactant in Canada at 5 ml/kg while in European centres the volume administered was half that. Now a low volume surfactant is available in Canada but some centres have been slow to make a switch due to comfort with the current product. The drawback to the current product is the concern that you can’t use it for LISA techniques since the centres practicing this technique use the low volume form.
Can High Volume Be Used For Lisa?
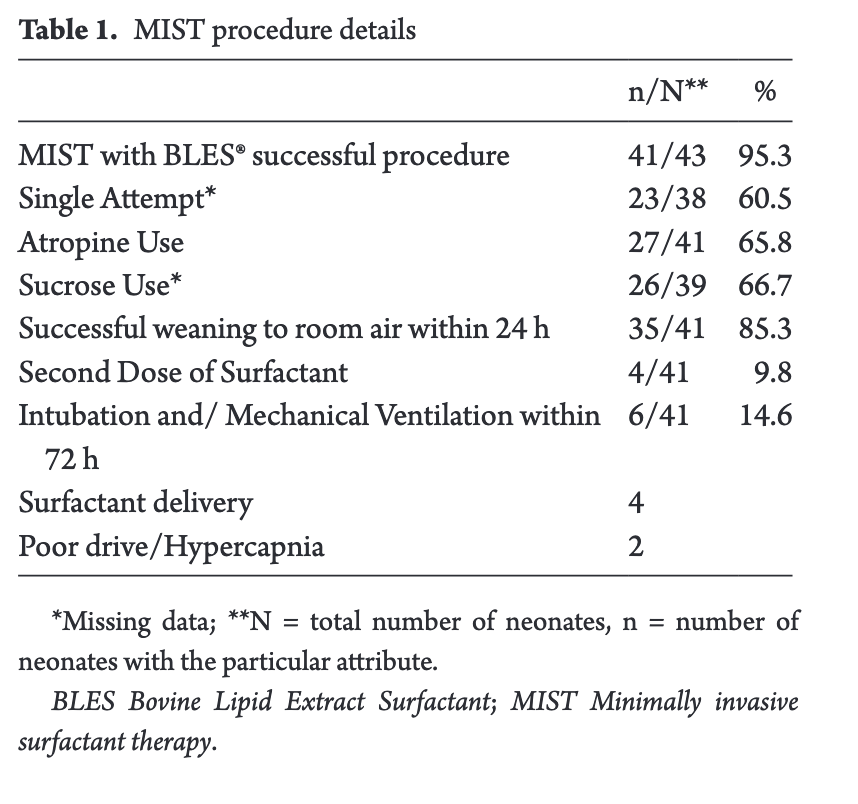
Researchers in London, Ontario performed a retrospective cohort study of 43 infants in their institution who underwent the MIST approach for surfactant administration in their study High-volume surfactant administration using a minimally invasive technique: Experience from a Canadian Neonatal Intensive Care Unit. In 2016, London instituted a change in practice to provide MIST for infants born at ≥28 weeks and/or with a birth weight ≥ 1,000 g with respiratory distress syndrome. Surfactant was provided over 1-3 minutes via a MAC catheter guided through the vocal cords with Magill forceps. What I like about this study is the reproducibility of it as the authors describe very nicely how the steps were done. What I also appreciate is the provision of sucrose and atropine prior to the procedure. Not a rapid sequence induction but it does do something to address the risk of bradycardia and discomfort with cannulation of the trachea. The results I think speak for themselves that this is indeed possible as 41/43 neonates underwent the procedure with successful instillation of surfactant confirmed by absence of recovered surfactant in aspirated stomach contents.
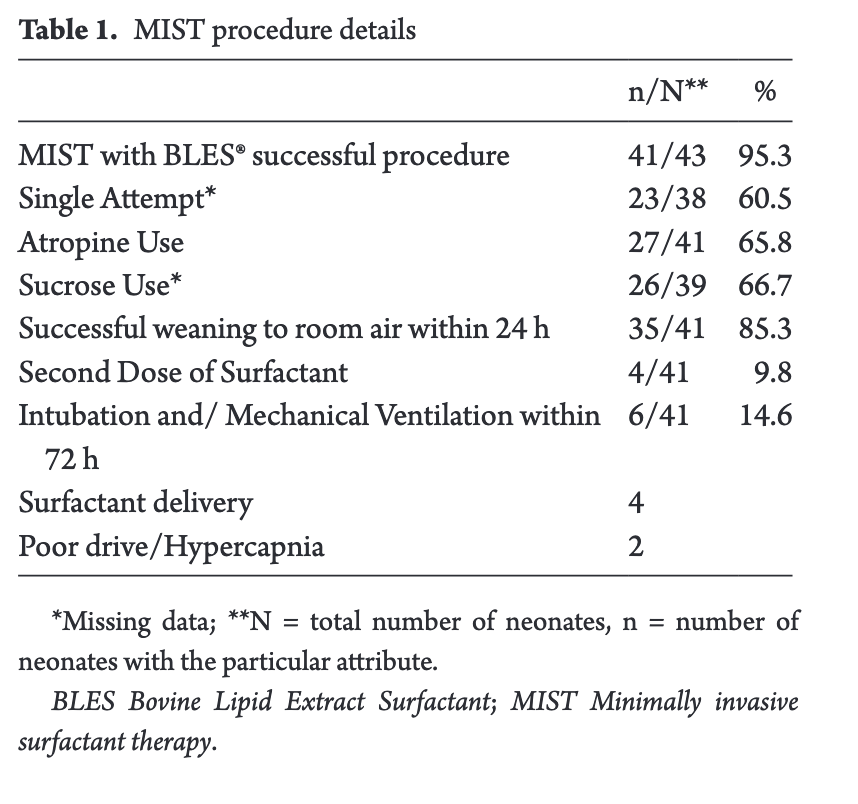
All of these infants qualified for BLES based on an oxygen requirement on non-invasive support of 40% or more. These patients are similar to our own in Winnipeg in terms of qualifying criteria for surfactant but perhaps a little higher tolerance of FiO2 before intubating. Additional evidence that surfactant was indeed received was the reduction to room air in 85% of patients within 24 hours and also the need for a second dose of surfactant in only 10%.
Aside from oxygen desaturation in about 50% during BLES administration the adverse effects were fairly limited and similar to what one would see with InSurE.
What now?
BLES can be administed via MIST despite concerns about the higher volume of surfactant. What many centres need to address I suspect is that while we think we are practicing InSurE, in many cases we are not. The goal of that procedure is to provide the surfactant over a few seconds and then get the ETT out right away. How often does that happen though in reality? Have you ever found yourself leaving the ETT in till the baby gets to NICU and extubating there? Seems safer right? What if in the elevator or hallway on the way to NICU the baby deteriorates and needs intubation? How long does the ETT stay in? Twenty minutes, 30, 45, 60 or longer? Thinking about that in a different way, what does that translate into in terms of number of PPV breaths? Well at a rate of 60 breaths a minute that means 1800, 2700, 3600 and more breaths before the ETT is removed. I have often wondered if this in itself explains why InSurE seems to be repeatedly identified as being inferior to MIST. If you intubated, gave the surfactant and pulled the ETT out right away in all cases might the two techniques actually be equivalent.
The question now really is how do we get past our tendencies and embrace a change in practice that by design will not allow us to delivery any positive pressure breaths?!

by All Things Neonatal | Aug 23, 2018 | intubation, surfactant, ventilation
A real change is coming and with this post you will get a glimpse into where the next big thing in Neonatology is likely to be. A catchy title for sure and also an exaggeration as I don’t see us abandoning the endotracheal tube just yet. There has been a lot of talk about less invasive means of giving surfactant and the last few years have seen several papers relating to giving surfactant via a catheter placed in the trachea (MIST or LISA techniques as examples). There may be a new kid on the block so to speak and that is aerosolized surfactant. This has been talked about for some time as well but the challenge had been figuring out how to aerosolize the fluid in such a way that a significant amount of the surfactant would actually enter the trachea. This was really a dream of many Neonatologists and based on a recently published paper the time may be now for this technique to take off.
A Randomized Trial of Aerosolized Surfacant
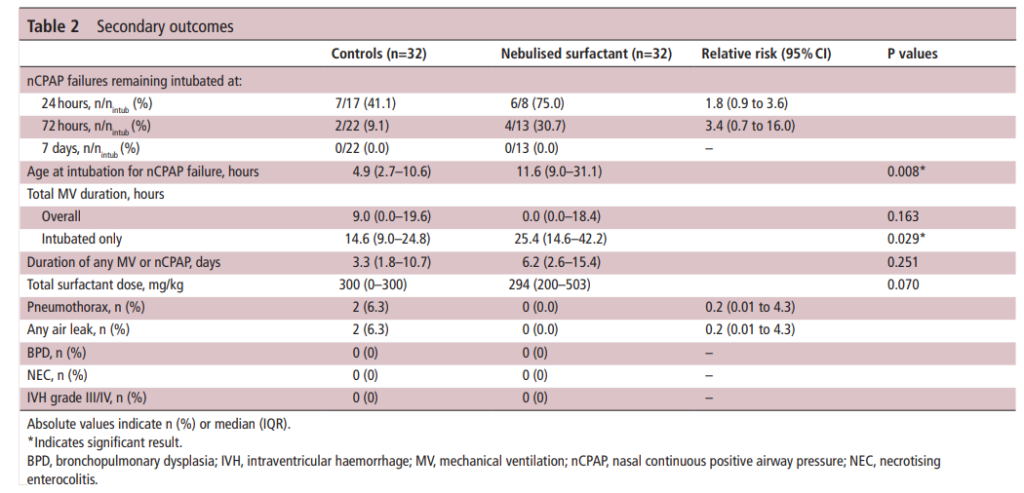
Minocchieri et al as part of the CureNeb study team published Nebulised surfactant to reduce severity of respiratory distress: a blinded, parallel, randomised controlled trial. This trial set out to obtain a sample size of 70 patients between 29 0/7 to 33 6/7 weeks to demonstrate a difference in need for intubation from 30% down to 5% in patients treated with CPAP (30% was based on the historical average). The authors recognizing that the babies in this GA bracket might behave differently, further stratified the randomization into two groups being 29 0/7 – 31 6/7 weeks and 32 0/7 to 33 6/7 weeks. Those babies who were on CPAP and met the following criteria for intubation were either intubated in the control group and given surfactant (curosurf) using the same protocol as those nebulized or had surfactant delivered via nebulisation (200 mg/kg: poractant alfa) using a customised vibrating membrane nebuliser (eFlow neonatal). Surfactant nebulisation(100 mg/kg) was repeated after 12 hours if oxygen was still required. The primary dichotomous outcome was the need for intubation within 72 hours of life, and the primary continuous outcome was the mean duration of mechanical ventilation at 72 hours of age.
Criteria for intubation
1. FiO2 >0.35 over more than 30 min OR FiO2 >0.45 at
anytime.
2. More than four apnea/hour OR two apnea requiring BVM
3. Two cap gases with pH <7.2 and PaCO2 >65 mm Hg (or) >60 mm Hg if arterial blood gas sample).
4. Intubation deemed necessary by the attending physician.
Did It Work?
Eureka! It seemed to work as 11 of 32 infants were intubated in the surfactant nebulisation group within 72 hours of birth vs.22 out of 32 infants receiving CPAP alone (RR (95% CI)=0.526 (0.292 to 0.950)). The reduction though was accounted for by the bigger babies in the 32 0/7 to 33 6/7 weeks group as only 1 of 11 was intubated when given nebulized surfactant compared to 10 of 13 managed with CPAP. The duration of ventilation in the first 72 hours was not different between the groups: the median (range) 0 (0–62) hour for the nebulization group and 9 (0–64) hours for the control group (p=0.220). It is important in seeing these results that the clinicians deciding whether infants should be intubated for surfactant administration were blind to the arm the infants were in. All administration of curosurf via nebulization or sham procedures were done behind a screen.
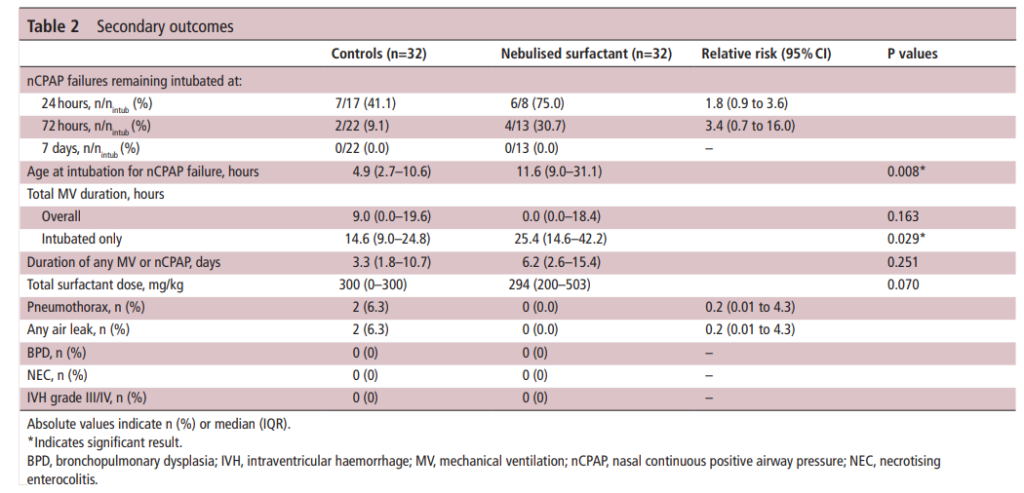
The total number of infants randomized were 66 so they did fall shy of the necessary recruitment but since they did find a difference the results seem valid. Importantly, there were no differences in complications although I can’t be totally confident there really is no risk as this study was grossly underpowered to look at rarer outcomes.
Breaking down the results
This study has me excited as what it shows is that “it kind of works“. Why would larger babies be the ones to benefit the most? My guess is that some but not a lot of surfactant administered via nebulization reaches the alveoli. Infants with lesser degrees of surfactant deficiency (32 0/7 to 33 6/7) weeks might get just enough to manage without an endotracheal tube. Those infants (in particular less than 32 0/7 weeks) who have more significant surfactant deficiency don’t get enough and therefore are intubated. Supporting this notion is the overall delay in time to intubation in those who were intubated despite nebulization (11.6 hours in the nebulization group vs 4.9 hours in the control arm). They likely received some deposition in the distal alveoli but not enough to completely stave off an endotracheal tube.
One concerning point from the study though had to do with the group of infants who were intubated despite nebulization of surfactant. When you look at total duration of ventilation (hours) it was 14.6 (9.0–24.8) in the control arm vs 25.4 (14.6–42.2) p= 0.029*. In other words infants who were intubated in the end spent about twice as long intubated as those who were intubated straight away. Not a huge concern if you are born at 32 weeks or more but those additional thousands of positive pressure breaths are more worrisome as a risk for CLD down the road.
As it stands, if you had an infant who was 33 weeks and grunting with an FiO2 of 35% might you try this if you could get your hands on the nebulizer? It appears to work so the only question is whether you are confident enough that the risk of such things as pneumothorax or IVH isn’t higher if intubation is delayed. It will be interesting to see if this gets adopted at this point.
The future no doubt will see a refinement of the nebulizer and an attempt to see how well this technique works in infants below 29 weeks. It is in this group though that prolonging time intubated would be more worrisome. I don’t want to dismiss this outright as I see this as a pilot study that will lead the way for future work that will refine this technique. If we get this right this would be really transformative to Neonatology and just might be the next big leap.

by All Things Neonatal | Feb 16, 2018 | intubation, surfactant
A common concern in the NICU these days is the lack of opportunity to intubate. A combination of an increasing pool of learners combined with a move towards a greater reliance on non-invasive means of respiratory support is to blame in large part. With this trend comes a declining opportunity to practice this important skill and with it a challenge to get a tube into the trachea when it really counts. One such situation is a baby with escalating FiO2 requirements who one wishes to provide surfactant to. Work continues to be done in the area of aerosolized surfactant but as of yet this is not quite ready for prime time. What if there was another way to get surfactant to where it was needed without having to instill it directly into the trachea whether through a catheter (using minimally invasive techniques) or through an endotracheal tube?
Installation of surfactant into the trachea
Lamberska T et al have published an interesting pilot study looking at this exact strategy. Their paper entitled Oropharyngeal surfactant can improve initial stabilisation and reduce rescue intubation in infants born below 25 weeks of gestation takes a look at a strategy of instilling 1.5 mL of curosurf directly into the pharynx for infants 22-24 weeks through a catheter inserted 3-4 cm past the lips as a rapid bolus concurrent with a sustained inflation maneuver (SIM) of 25 cm of H2O for 15 seconds. Two more SIMs were allowed of the heart rate remained < 100 after 15 seconds of SIM. The theory here was that the SIM would trigger an aspiration reflex as the pressure in the pharynx increased leading to distribution of surfactant to the lung. The study compared three epochs from January 2011 – December 2012 when SIM was not generally practiced to July 2014 – December 2015 when SIM was obligatory. The actual study group was the period in between when prophylactic surfactant with SIM was practiced for 19 infants.
A strength of the study was that resuscitation practices were fairly standard outside of these changes in practice immediately after delivery and the decision to intubate if the FiO2 was persistently above 30% for infants on CPAP. A weakness is the size of the study with only 19 patients receiving this technique being compared to 20 patients before and 20 after that period. Not very big and secondly no blinding was used so when looking at respiratory outcomes one has to be careful to ensure that no bias may have crept in. If the researchers were strongly hoping for an effect might they ignore some of the “rules around intubation” and allow FiO2 to creep a little higher on CPAP as an example? Hard to say but a risk with this type of study.
What did they find?
The patients in the three epochs were no different from one and other with one potentially important exception. There were higher rates of antenatal steroid use in the study group (95% vs 75 and 80% in the pre and post study epochs). Given the effect of antenatal steroids on reducing respiratory morbidity, this cannot be ignored and written off.
Despite this difference it is hard to ignore the difference in endotracheal intubation in the delivery room with only 16% needing this in the study group vs 75 and 55% in the other two time periods. Interestingly, all of the babies intubated in the delivery area received surfactant at the same percentages as above. The need for surfactant in the NICU however was much higher in the study period with 79% receiving a dose in the study group vs 20 and 35% in the pre and post study groups. Other outcomes such as IVH, severe ROP and BPD were looked at with no differences but the sample again was small.
What can we take from this?
Even taking into account the effect of antenatal steroids, I would surmise that some surfactant did indeed get into the trachea of the infants in the study group. This likely explains the temporary benefit the babies had in the delivery suite. I suspect that there simply was not a big enough dose to fully treat their RDS leading to eventual failure on CPAP and a requirement for intubation. Is all lost though? Not really I think. Imagine you are in a centre where the Neonatologist is not in house and while he/she is called to the delivery they just don’t make it in time. The trainee tries to intubate but can’t get the tube in. Rather than trying several times and causing significant amounts of airway trauma (as well as trauma to their own self confidence) they could abandon further attempts and try instilling some surfactant into the pharynx and proving a SIM. If it works at all the baby might improve enough to buy some time for them to be stabilized on CPAP allowing time for another intubater to arrive.
While I don’t think there is enough here to recommend this as an everyday practice there just might be enough to use this when the going gets tough. No doubt a larger study will reveal whether there really is something here to incorporate into the tool chest that we use to save the lives of our smallest infants.

by All Things Neonatal | Dec 28, 2017 | preemie, Prematurity, technology, ventilation
Intubation is not an easy skill to maintain with the declining opportunities that exist as we move more and more to supporting neonates with CPAP. In the tertiary centres this is true and even more so in rural centres or non academic sites where the number of deliveries are lower and the number of infants born before 37 weeks gestational age even smaller. If you are a practitioner working in such a centre you may relate to the following scenario. A woman comes in unexpectedly at 33 weeks gestational age and is in active labour. She is assessed and found to be 8 cm and is too far along to transport. The provider calls for support but there will be an estimated two hours for a team to arrive to retrieve the infant who is about to be born. The baby is born 30 minutes later and develops significant respiratory distress. There is a t-piece resuscitator available but despite application the baby needs 40% oxygen and continues to work hard to breathe. A call is made to the transport team who asks if you can intubate and give surfactant. Your reply is that you haven’t intubated in quite some time and aren’t sure if you can do it. It is in this scenario that the following strategy might be helpful.
Surfactant Administration Through and Laryngeal Mask Airway (LMA)
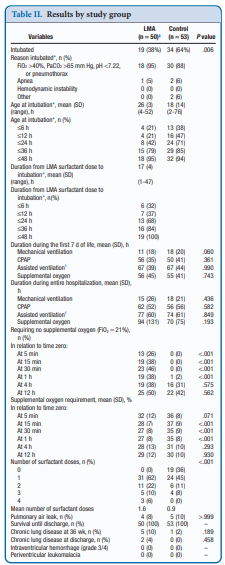
Use of an LMA has been taught for years in NRP now as a good choice to support ventilation when one can’t intubate. The device is easy enough to insert and given that it has a central lumen through which gases are exchanged it provides a means by which surfactant could be instilled through a catheter placed down the lumen of the device. Roberts KD et al published an interesting unmasked but randomized study on this topic Laryngeal Mask Airway for Surfactant Administration in Neonates: A Randomized, Controlled Trial. Due to size limitations (ELBWs are too small to use this in using LMA devices) the eligible infants included those from 28 0/7 to 35 6/7 weeks and ≥1250 g. The infants needed to all be on CPAP +6 first and then fell into one of two treatment groups based on the following inclusion criteria: age ≤36 hours,
(FiO2) 0.30-0.40 for ≥30 minutes (target SpO2 88% and 92%), and chest radiograph and clinical presentation consistent with RDS.
Exclusion criteria included prior mechanical ventilation or surfactant administration, major congenital anomalies, abnormality of the airway, respiratory distress because of an etiology other than RDS, or an Apgar score <5 at 5 minutes of age.
Procedure & Primary Outcome
After the LMA was placed a y-connector was attached to the proximal end. On one side a CO2 detector was placed and then a bag valve mask in order to provide manual breaths and confirm placement over the airway. The other port was used to advance a catheter and administer curosurf in 2 mL aliquots. Prior to and then at the conclusion of the procedure the stomach contents were aspirated and the amount of surfactant determined to provide an estimate of how much surfactant was delivered to the lungs. The primary outcome was treatment failure necessitating intubation and mechanical ventilation in the first 7 days of life. Treatment failure was defined upfront and required 2 of the following: (1) FiO2 >0.40 for >30
minutes (to maintain SpO2 between 88% and 92%), (2) PCO2 >65 mmHg on arterial or capillary blood gas or >70 on venous blood gas, or (3) pH <7.22 or 1 of the following: (1) recurrent or severe apnea, (2) hemodynamic instability requiring pressors, (3) repeat surfactant dose, or (4) deemed necessary by medical provider.
Did it work?
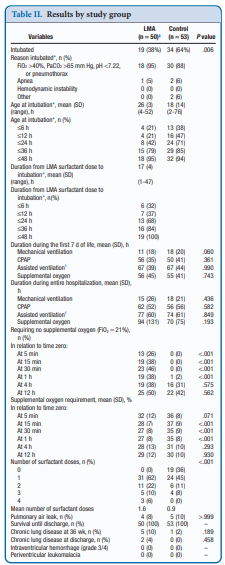
It actually did. Of the 103 patients enrolled (50 LMA and 53 control) 38% required intubation in the LMA group vs 64% in the control arm. The authors did not reach their desired enrollment based on their power calculation but that is ok given that they found a difference. What is really interesting is that they found a difference in the clinical end point despite many infants clearly not receiving a full dose of surfactant as measured by gastric aspirate. Roughly 25% of the infants were found to have not received any surfactant, 20% had >50% of the dose in the stomach and the other 50+% had < 10% of the dose in the stomach meaning that the majority was in fact deposited in the lungs. I suppose it shouldn’t come as a surprise that among the secondary outcomes the duration length of mechanical ventilation did not differ between two groups which I presume occurred due to the babies needing intubation being similar. If you needed it you needed it so to speak. Further evidence though of the effectiveness of the therapy was that the average FiO2 30 minutes after being treated was significantly lower in the group with the LMA treatment 27 vs 35%. What would have been interesting to see is if you excluded the patients who received little or no surfactant, how did the ones treated with intratracheal deposition of the dose fare? One nice thing to see though was the lack of harm as evidenced by no increased rate of pneumothorax, prolonged ventilation or higher oxygen.
Should we do this routinely?
There was a 26% reduction in intubations in te LMA group which if we take this as the absolute risk reduction means that for every 4 patients treated with an LMA surfactant approach, one patient will avoid intubation. That is pretty darn good! If we also take into account that in the real world, if we thought that little of the surfactant entered the lung we would reapply the mask and try the treatment again. Even if we didn’t do it right away we might do it hours later.
In a tertiary care centre, this approach may not be needed as a primary method. If you fail to intubate though for surfactant this might well be a safe approach to try while waiting for a more definitive airway. Importantly this won’t help you below 28 weeks or 1250g as the LMA is too small but with smaller LMAs might this be possible. Stay tuned as I suspect this is not the last we will hear of this strategy!
 (a founding member of the “Tall Men of Pediatrics #TMOP) published a systematic review and meta-analysis of all such RCTs in their paper Efficacy and safety of pulmonary application of corticosteroids in preterm infants with respiratory distress syndrome: a systematic review and metaanalysis. The results of the study suggest that there may well be a role for this approach.
(a founding member of the “Tall Men of Pediatrics #TMOP) published a systematic review and meta-analysis of all such RCTs in their paper Efficacy and safety of pulmonary application of corticosteroids in preterm infants with respiratory distress syndrome: a systematic review and metaanalysis. The results of the study suggest that there may well be a role for this approach.