In an effort to reduce the incidence of IVH many patient care bundles in the last number of years have advocated for minimal handling. As part of approach to minimal handing an effort to keep the head straight and in some centres elevated has been postulated to help with enhancing venous outflow from the head. By reducing the passive gravity aided flow from the brain back into the thorax the theory would be that this would help minimize venous pressure in the draining cerebral system. Lowering pressure would in turn theoretically reduce the risk of IVH and hopefully the most severe types. The evidence to support this practice has largely been observational in the sense that those units practising this sort of intervention have published reductions in rates of severe IVH such as reported for small baby units. The fly in the ointment however is that many changes occur in the care of these infants so definitively attributing the difference in outcomes to just one intervention such as midline head positioning with elevation of the head can be challenging.
A Study to Sort It Out
Researchers in Iran sought to answer this question with an elegant study in which 39 patients served as their own controls and had NIRS monitoring through different head positions. This study entitled The effect of head positioning on brain tissue oxygenation in preterm infants: a randomized clinical trial study by Mohamammadie et al looked at these infants over the first 48 hours of life. Each infant went through NIRS monitoring and were randomly placed in six different positions as shown in the figure.
The infants studied were those who would be most vulnerable to IVH so were all <=32 weeks and < 1500g. The authors acknowledged that they would have liked to record over the first 72 hours as this has traditionally become the period of minimal handling in care bundles but claim that they did not have enough data past 48 hours to comment.
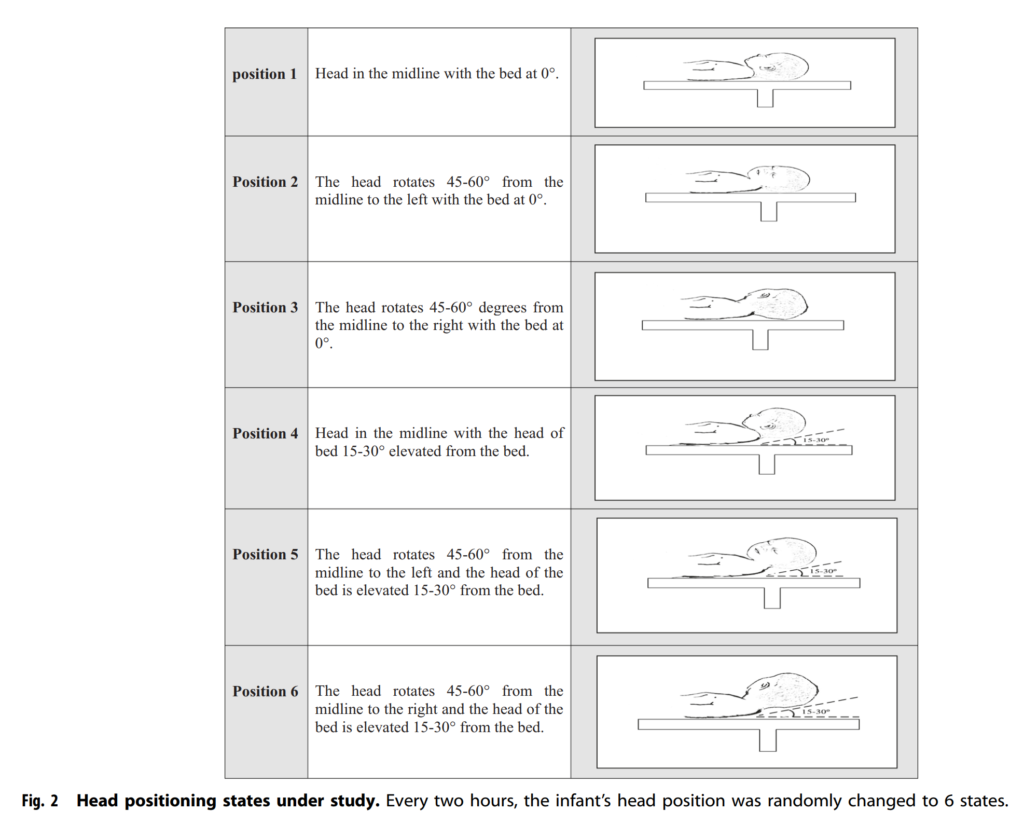
Prior to starting positional changes ten minutes of baseline recording was done in the midline position without elevation. Each position was used for a period of 2 hours during which NIRS monitoring was performed. The goal here was to see if the amount of oxygen extraction changed with different head positions and elevations. If the extraction increased in one head position it would be thought to reflect slowed return of venous blood with further extraction of oxygen from the brain.
What did the authors find?
Since I am reporting the findings it shouldn’t surprise you that they found something here. What might surprise you though is the actual difference in what they found. If one would have to guess before sharing the results it would seem that laying the head of the bed flat would not help with venous drainage as much as a 15-30 degree elevation so let’s guess that they would find that. Also, based on a belief that the jugular veins might be kinked if you turn your head to one side or the other let’s guess that midline head positioning does make a difference. Looking at the results below, let’s see if this actually happened.
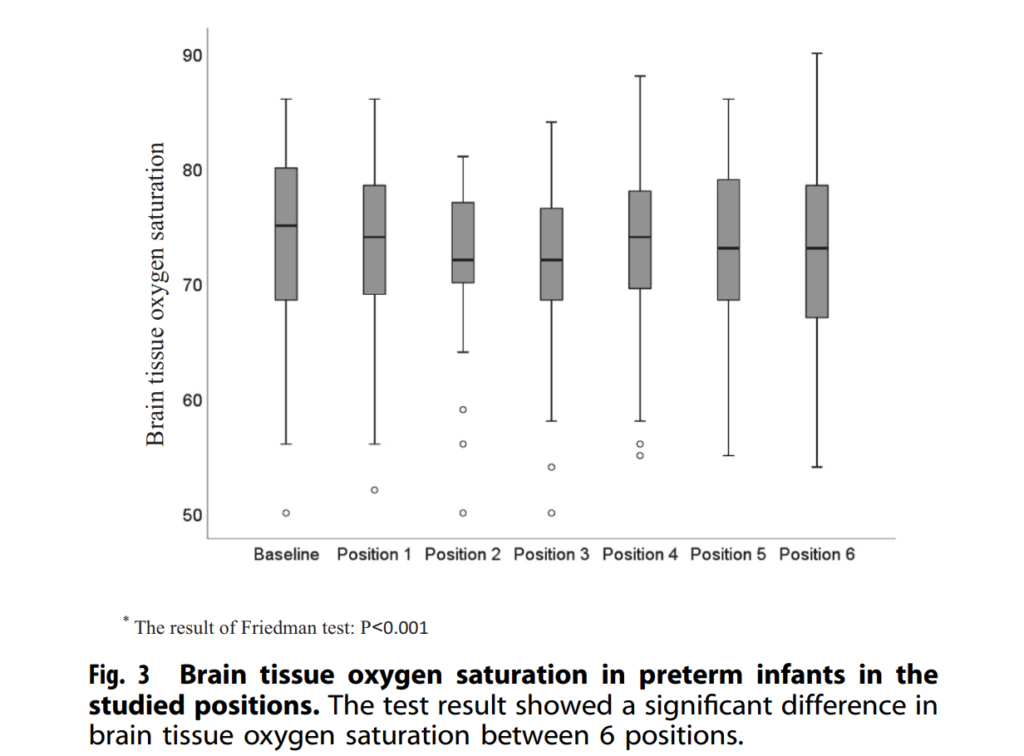
As you can see the highest NIRS recordings were found in the baseline position and in general the three positions with the head of bed elevated (Position 4-6) and when flat in the midline (Position 1). It would seem then that the anticipated benefit was shown! From a statistical standpoint the third position was found to be different as was the fourth compared to the first position.
What does it all mean though?
A statistically different finding was achieved which shows the 3rd and 4th positions are not as good as baseline for sure but what about clinical significance. The lower limit of normal for NIRS readings is about 60. The means for all of these positions were in the 70s. In fact the difference between the mean of the 3rd and 4th positions and the others were only about 2%. Is this enough to make a difference? I honestly am not sure. There is a difference that reaches statistical significance so if we accept that there may have been some disruption of venous flow is this enough evidence to totally explain the reductions in IVH that have been seen with bundles for minimal handling with positioning? There were a lot of variables here that could not be controlled such as time of day that a baby was in one position or another since it was random. Was there a lot of noise in the unit at the time of one position or another? Depending on circadian rhythms what would the cortisol levels be and might mild changes in blood pressure explain the findings since they are so small?
I don’t want to totally dismiss the findings but suspect that it isn’t just the positioning that is leading to reductions in IVH. The same units that promote small baby care are also pushing breastfeeding rates up, skin to skin care and trying to harmonize other aspects of care. If we are seeing reductions in IVH which is a wonderful thing is it all related to this? Probably not but what this study does in my mind is support the theories about enhancing venous drainage through positioning and I see no reason not to continue this practice and try to keep these infants in the mid line and avoid bothering them as much as possible as they transition from the in-utero to ex-utero environment.

