Here in Winnipeg we don’t use t-piece resuscitators for any resuscitation. I did use them in my past position in Edmonton and I came to appreciate them for their ease of use. For the majority of infants, setting a PIP and a PEEP and then using your finger to occlude and release offers a relatively simple and less difficult approach to ventilation than using a self inflating or jackson-rees bag. I say the majority of infants, as most infants are not born from 22-32 weeks but the lion’s share are born at gestations older than that. The larger more mature infants have lungs that are much more forgiving to excessive ventilation. For the smallest of infants though questions have remained for some time around the volumes delivered to the fragile lung when a fixed pressure is used in the presence of moment to moment changes in compliance.
Measuring Tidal Volume in Intubated At Risk Infants
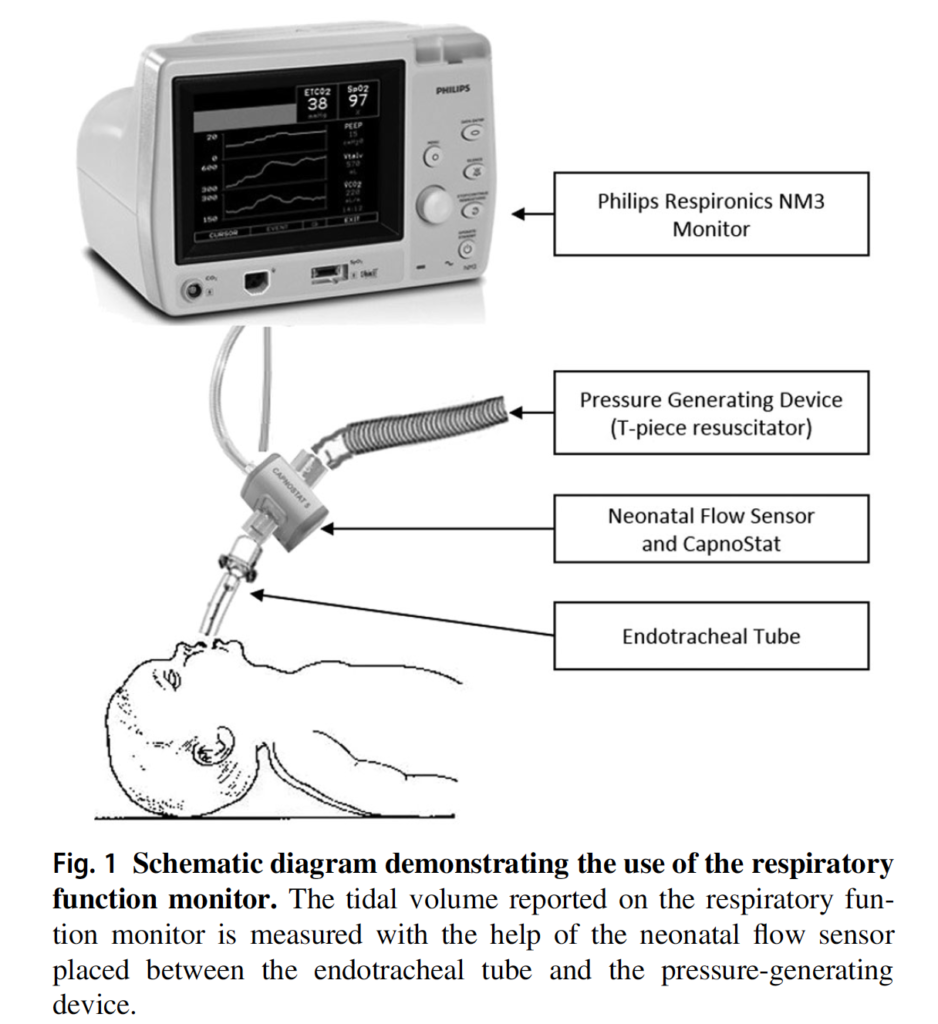
Vaidya R et al published Tidal volume measurements in the delivery room in preterm infants requiring positive pressure ventilation via endotracheal tube feasibility study in Journal of Perinatology. The prospective observational study looked at 10 infants born at < 32 weeks with a mean GA of 23.9(±1.5) weeks and mean BW 618.5(±155)g. A mean of 17.8 minutes of recordings were examined using the setup below and in total looked at 8175 individual breaths. All patients in the study were intubated with non-cuffed ETT but by only including intubated infants in the delivery room the issue of mask leak was avoided. As in many units the target Vt was 4-6 mL/kg. It wasn’t specified what criteria they use for setting initial pressures but the included patients had a mean PIP of 24.4±5 and PEEP of 5.9 ±2.4. Importantly, those providing ventilation with the t-piece resuscitator were blinded to the data on tidal volume measurements.
How Good Were They At Meeting Their Goal?
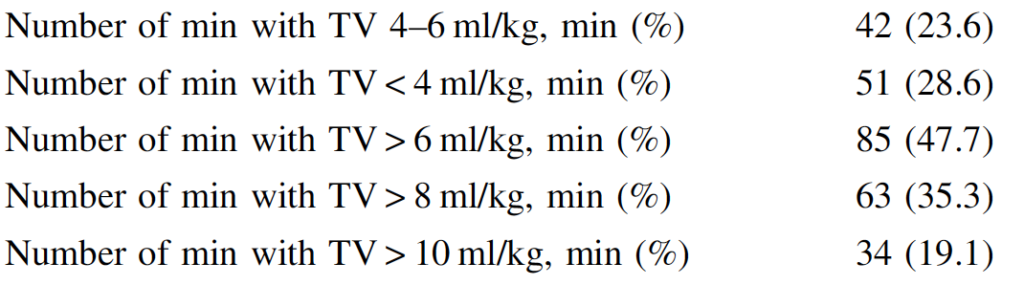
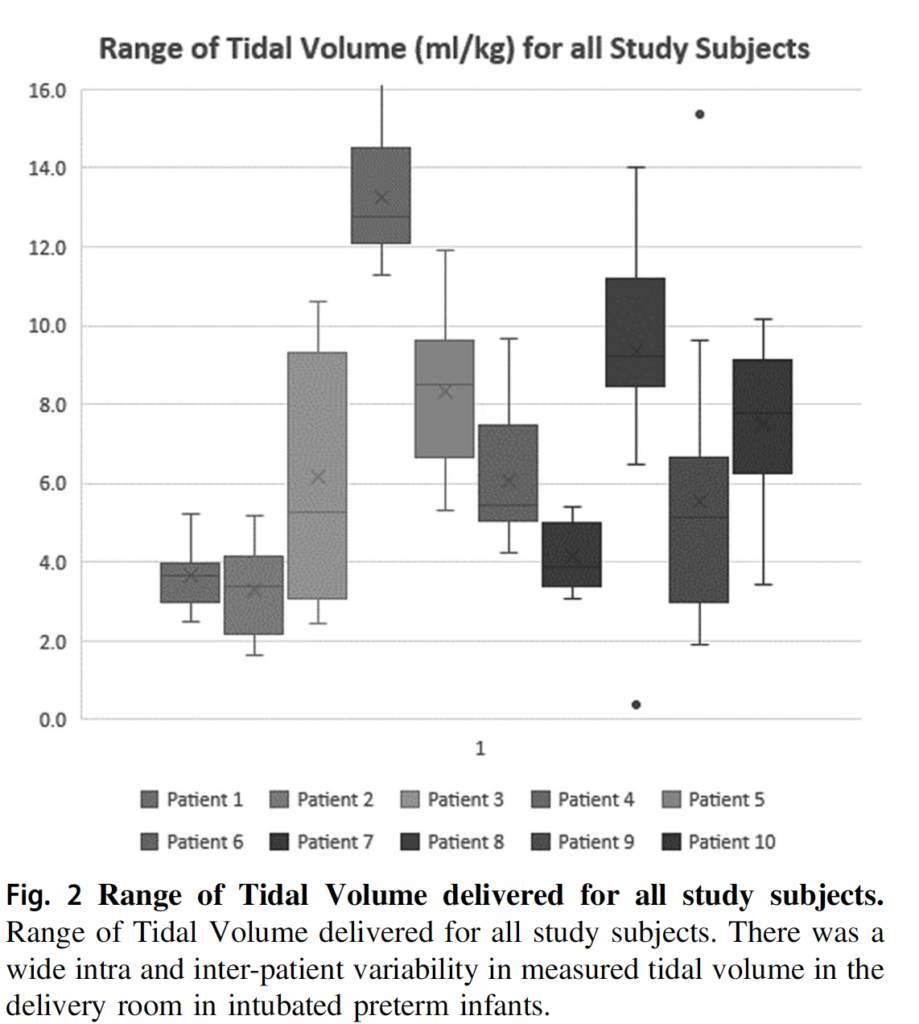
It turns out that they weren’t that great (I am not faulting them by the way) as it is a challenge to try and adjust pressures based on chest rise. We are not good at it at all. As shown in the figure below there was a wide range of volumes administered. In fact here is the breakdown. The goal Vt between 4-6 was only 25% of the time. In other words you are dealing with either a risk of atelectotrauma or volutrauma 75% of the time. It is worth noting that the neonatal flow sensor has a dead space of 1 mL. If that is the case and the infants on average were about 600g that is almost 2 mL/kg in non-ventilated space that this volume is going into. It doesn’t change the numbers that much if you factor that in but it does mean that some infants who were getting a measured 3 mL/kg were actually seeing under 2 mL/kg of lung ventilation. On the other hand those getting 7 mL/kg were actually seeing under 6 mL/kg so were in target. Bottom line though is that when using fixed pressure settings in the presence of changing compliance even if one is adjusting pressure in real time it is difficult to maintain stable volumes in target range. The authors also demonstrate in another graph that even in individual patients there is fluctuation as well.
Call to Action
I think this study is actually quite useful in confirming what I imagine many have always suspected. We just aren’t that great at assessing tidal volume when we watch the chest rise. As many have noted, the first 6 breaths at least in an animal model can damage the lungs. Imagine what excessive or low volumes can do to the lung over 18 minutes?!
What this study does is demonstrate especially in the smallest and most vulnerable infants that if ventilation is needed one should put the infant onto a volume guaranteed mode of ventilation ASAP. Ventilators should be in the resuscitation area as we have in our hospital and not have to be brought in should the baby be intubated. Hand bagging even with a t-piece resuscitator should be kept to a minimum. At risk is the development of BPD and knowing that even in experienced hands we just aren’t that good at delivering tidal volumes in a target range we need to strive to minimize the time that we expose our infants to such modalities. Ventilation isn’t always avoidable but when needed my advice is to control volume and allow pressures to fluctuate as resistance and compliance change. Especially after administration of surfactant the pulmonary mechanics are changing constantly and no matter how good you are you just won’t be able to keep pace. Let the ventilator do it!

