If there is a country that leads this site in terms of mentions it has to be Sweden. This isn’t just because I happen to know some Neonatologists from there who are fine people but because of the fantastic research that spills forth from their national registry of births. Surfactant is one of the oldest treatments we have in Neonatology and we know that in babies with RDS giving it early within 2 hours has benefits such as reduction in pneumothorax. The reality though is that as we have become familiar with the therapy its use has spilled over to other conditions. Years ago use of surfactant in meconium aspiration syndrome was shown to reduce need for ECMO. It has also been shown to imrove clinical condition in babies with pneumonia. Interestingly as a fellow I was criticised one call night for wanting to give a three day old baby with a history of RDS and high FiO2 requirements a repeat dose of surfactant. That was in 2001 and at that time no one could believe I was suggesting such an odd thing to give a dose after 48 hours yet now this is commonplace. Again as we have become more comfortable with surfactant such “off label” use spreads. I am not being critical of my colleagues back in 2001 as that was what the “conventional wisdom” was with respect to surfactant but that was then and this is now.
What Are The Swedes Doing With Surfactant?
A lot of good work it turns out! The observational study being reviewed here was published in JAMA Network Open by Callis P et al and entitled Association of Adherence to Surfactant Best Practice Uses With Clinical Outcomes
Among Neonates in Sweden
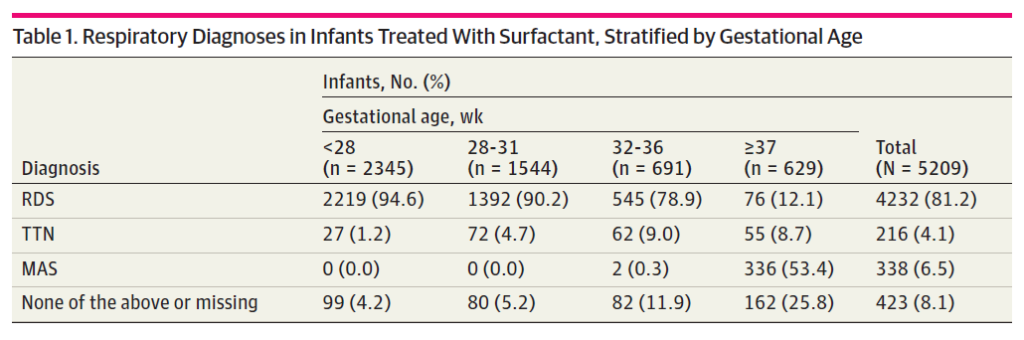
Looking at their registry data for 97377 infants born from 2009-2018 they found 7980 surfactant administrations to 5209 infants. The reasons for surfactant administration are shown in the table 1 below from the paper. Clearly and not surprisingly the bulk of surfactant administration is for RDS especially as gestational age declines. Given that so few preterm infants will pass meconium in-utero it also is understandable why MAS clusters in the more mature babies.
When it comes to multiple surfactant administrations they found 59.2% received 1 administration,
25.8% received 2, 7.3% had 3, and 2.8% had 4 or more administrations. Not surprisingly the more immature infants were more likely to receive multiple administrations. I have to say at this point that I feel vindicated with that suggestion for late surfactant administration all those years ago as these extra doses would have been given up to days after the first dosing.
Now Here Comes The Interesting Part
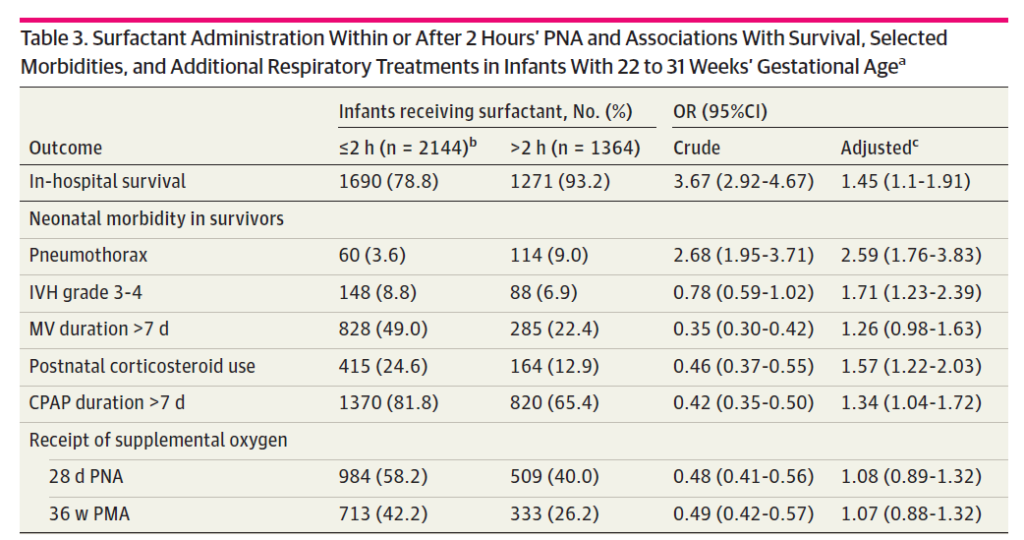
Much like previous work before this study, delivery of surfactant within the first 2 hours of age was associated with a reduction in very important outcomes of pneumothorax, IVH and need for ventilation beyond 7 days.. In short, improving compliance has a lot of benefits! The surprise was the in-hospital survival which favoured giving surfactant late. Put another way, if you receive surfactant in the first two hours you are more likely to die in hospital.
How can that possibly be if provision of surfactant has all those benefits outlined in table 3? More on that in a bit.
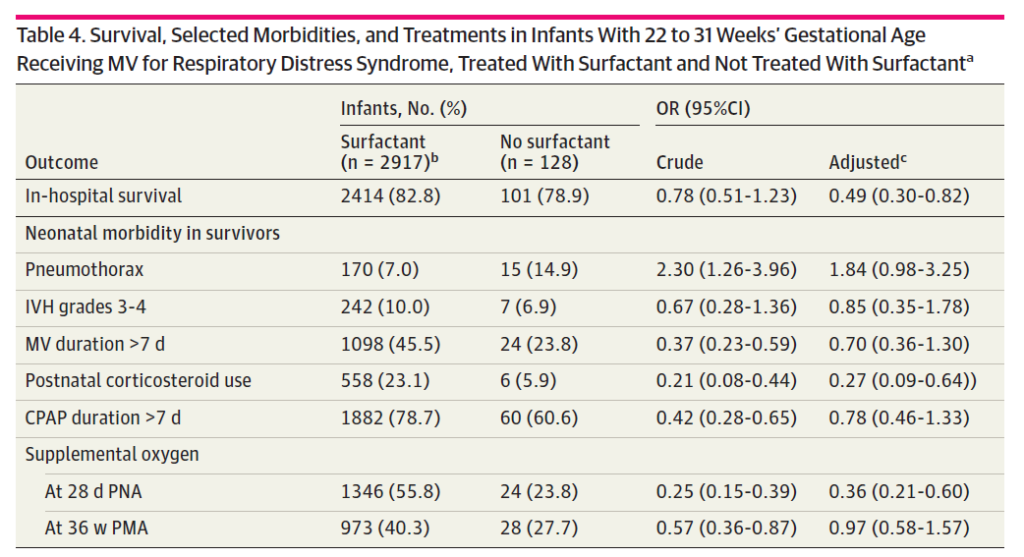
The next table addresses another question which is what if you don’t get surfactant at all? Interestinly the in-hospital survival is better for that group as well. On the other hand no difference exists for pneumothorax or IVH and ventilation beyong 7 days is improved with no surfactant at all!
The Difference Between Association and Causation
Ultimately that is what I think is at play here. You could look at the information quickly and conclude that giving surfactant late or not at all improves your chances of survival! Maybe aggressive use of surfactant isn’t such a good thing after all. I think you would be wrong there though based on prospective randomized trials. What is happening here is that the baseline characteristics are not likely equal and you are really looking at three different groups of patients.
Group 1 – These are the ones who get surfactant early within 2 hours of life. My suspicion is that the number of babies in this group that are really sick who may also have other comorbid issues is higher. There might be some babies with servere IUGR, pulmonary hypoplasia, meconium aspiration or pleural effusions that made the resuscitating team so nervous that they in advance of delivery had surfactant thawing and ready to go. Yes overall this group might benefit from better compliance and have less pneumothoraces for example but their comorbid conditions put them at higher risk of death.
Group 2 – Surfactant given after 2 hours of age. These are likely babies who are not as sick as group 1. Maybe they are babies initially managed with CPAP or NIPPV who due to escalating FiO2 requirements get surfactant. Much less likely to die.
Group 3 – No surfactant needed at all. The reason there might not be a difference in the major morbidities is that while they have RDS, TTN or MAS they are mild in nature. Clearly very low risk of death here and for that matter complications.
It might have been helpful to have some meaures of acuity documented such as SNAPPE-II (Score for Neonatal Acute Physiology with Perinatal Extension-II) used as it would help us in figuring out such differences.
Overall I think the message remains the same. Give surfactant early for those with significant lung disease. What I think it adds is an awareness that repeat dosing even if off-label is being done in Neonatology. The next question will be whether this repeat dosing makes the babies better or just us!