This post is special to me. A redemption of sorts. When I was a fellow in Edmonton in the early 2000s my fellowship project was to see whether heliox (helium/oxygen) given to piglets with meconium aspiration syndrome (MAS) would improve ventilation and measures of pulmonary hypertension vs controls. Why heliox? There had been work done with this gas for other conditions and the lower viscosity of the gas (who hasn’t sucked on a helium balloon to see the effect of helium) means that the flow of the gas in a tube is more linear that regular air. Turbulent flow as with air/oxygen mixtures creates more resistance to flow than linear flow with heliox. Imagine if you will this linear flow slipping more easily past particles of meconium partially blocking airways and you get the idea of why heliox might work. One thing to bear in mind though is that as your FiO2 goes up the percentage of helium drops so the properties described work best at low FiO2 so flow is more linear.
I collected meconium from diapers in the NICU and created a NS slurry of meconium and then instilled it into the trachea’s of these piglets through a tracheostomy (they were too small to intubate for me at least). A flow probe was put around the pulmonary artery to look for evidence of pulmonary hypertension. We saw some interesting trends but the paper never saw the light of day for a variety of reasons that I won’t go in to here. Originally I had wanted to do the study as a small RCT in humans but I was advised that although heliox is an inert gas I should do the animal study first. That was the end of the heliox story as far as I was concerned as I hadn’t thought much about it since that time. I will admit though that anytime I had a baby with bad meconium aspiration syndrome though the thought did pop into my head.
The Study Has Arrived
Imagine my surprise when this week an RCT from China entitled A randomized single‐center controlled trial of synchronized intermittent mandatory ventilation with heliox in newborn infants with meconium aspiration syndrome came across my inbox. The authors used a power calculation based on some previous work in RDS using heliox to determine they needed 28 neonates in each arm to show a difference. In the end they managed 71 total with 35 in the heliox and 36 in the control arm. Inclusion criteria were a diagnosis of MAS on x-ray, GA ≥37 weeks and ≤42 weeks, need for intubation due to a pH <7.2/PCO2 >60 mmHg. The study could not be blinded as one would not be able to hide the large tanks for heliox so for any study like this it would be unavoidable. One thing that differs in terms of management from my own practice is that the authors in this study used SIMV pressure limited ventilation as the ventilatory strategy as opposed to AC/VG that my unit would typically use. Initial ventilator PIP of 15–28 cmH2O, PEEP of 4–10 cmH2O, and RR of 15–45 breaths/min; FiO2 of 0.21 to 1 to reach the target oxygen saturation (SpO2) of 90%–95%. The intervention group received heliox for 6 hours and then switched over to air/oxygen while the control group was ventilated with air/oxygen from the start. The extubation criteria included PIP ≤15 cmH2O, gradually enhanced effective spontaneous breathing, a ventilator breathing frequency ≤10/min, and normal blood gas analysis results. The main outcomes were PaO2/FiO2 (P/F), the extubation time and the hospital length of stay in the NICU. Aside from measuring the ventilatory responses and time of extubation the authors also examined the effect of heliox as an anti-inflammatory agent based on previous results demonstrating markers of inflammation can be attenuated by use of the gas.
The Results
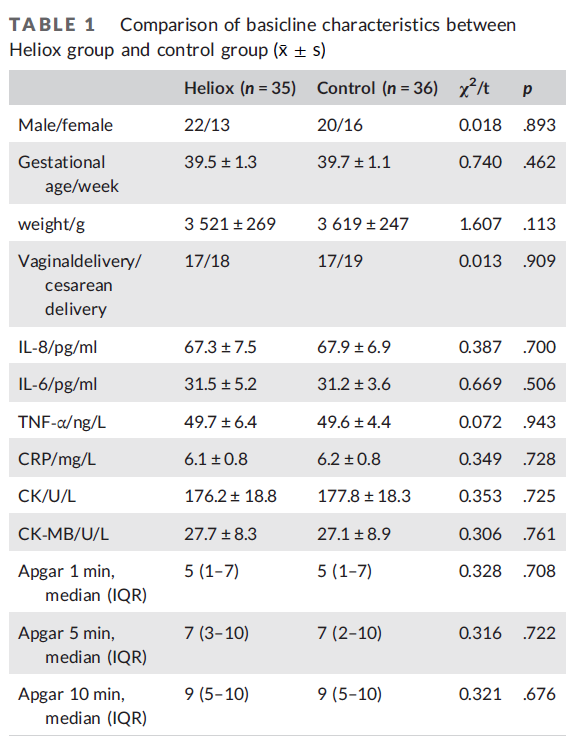
To start with, the babies in both arms were equivalent at the start of the study in terms of inflammatory markers and some clinical variables.
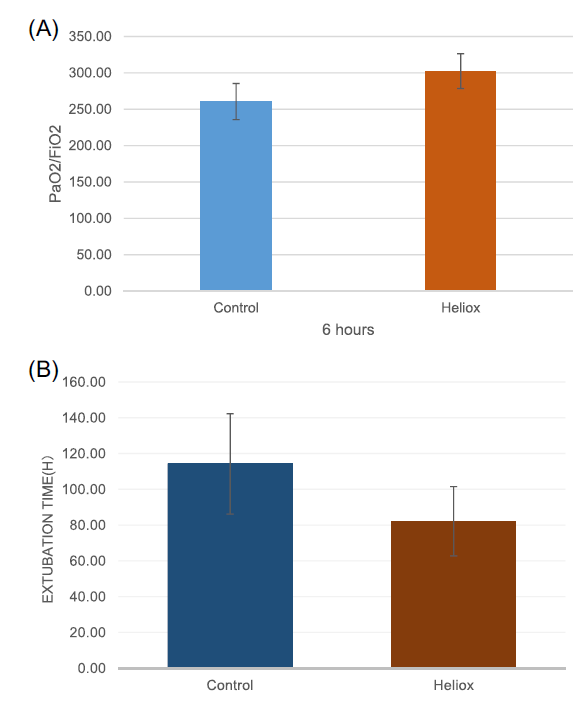
As you will see from the following figures a number of important findings are noted. The main marker of oxygenation used for this study was the PaO2/FiO2 ratio and this was statistically different (301 ± 22 vs. 260.64 ± 24.83, p < .001). Secondly, extubation time (78 ± 30 vs. 114 ± 28.07, p < .001 and length of hospital stay in days were also shorter 15.3 ± 4.2 vs. 19.11 ± 4.01, p < .001.
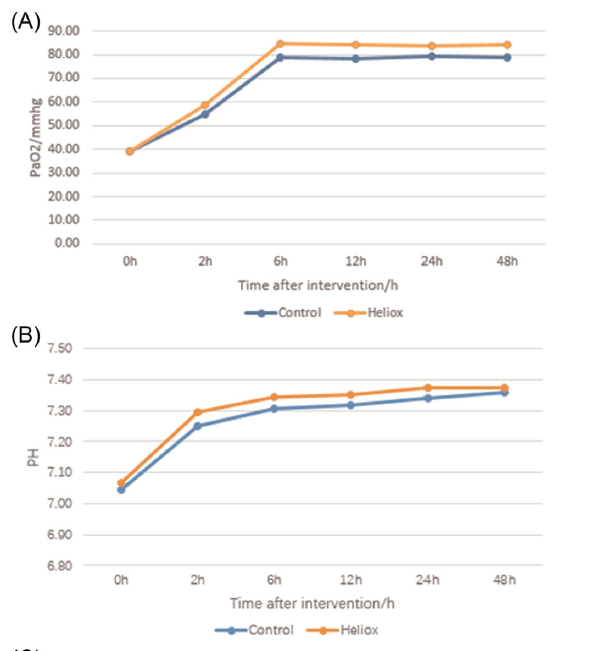
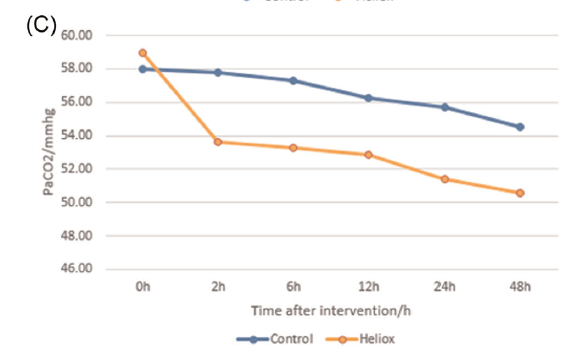
The authors state that the following markers of pO2, pH and pCO2 shown in the graphs were all significantly improved in the heliox group but looking at the first two I find that hard to believe as the curves look almost superimposed. pCO2 however could be different in particular given the linear flow described above so ventilation might be improved.
Finally, across the board, markers of inflammation were noted to improve with administration of heliox as well as markers of myocardial injury. The gas may have done what it was supposed to do.
I wish the conclusions were that easy
I want to like this paper so badly. Sadly, I have some pretty significant reservations. It is helpful to see that the two groups began at a similar PaO2/FiO2 ratio. What is missing though is the ventilatory requirements to get to that point. There is no information provided as to the mean airway pressures or PIP/PEEP for each group over time to get a sense of whether the two groups in terms of severity of illness were the same. Yes we know that the inflammatory markers at the start were similar but could the difference in changes of inflammation relate to a progressive rise in the control group that were just sicker rather than a protective effect of heliox to reduce inflammation? Also when one looks at the change in pCO2 how do you interpret that without knowing the minute ventilation to achieve those data points? It is really unfortunate that the authors did not use oxygenation index (MAP X FiO2/PaO2) as this would have taken the ventilation component at least into account. Would be helpful as well to know the weaning strategy in each group as without blinding might the authors have reacted more aggresively with weaning of the ventilator to get to extubatable settings knowing that the babies were receiving the intervention. As there was no weaning strategy planned out from the start we can only guess. Lastly, one could have possibly gotten around the inability to hide the heliox tanks by having a Neonatologist not on service take each blood gas data and sight unseen suggest changes to ventilation without being able to see which arm a baby was in.
I will end on a positive note though. It has been almost twenty years since I did the piglet study using heliox. I had always hoped that this research would see the light of day in a human model although my piglet data didn’t show much benefit however the intervention was shorter than this study. I think this study is worthy of being repeated using a different mode of ventilation that does not rely on manual changes to PIP but rather by using a VG mode the baby would be gradually weaned as compliance improves. Any further study needs to address differences that were missing from this paper as well. I don’t think this is the last we will see of heliox and I look forward to seeing another paper although if it takes another twenty years I may be out of this line of work.

