This post is a written as a tribute to John Minski RRT who taught me much about ventilation over the years and has been a champion for innovation in our unit. As he prepares to move on to the next phase of his life I thought it would be a nice send off to talk about something that he has been passionate about for some time. That passion is inhaled nitric oxide for more than just pulmonary hypertension.
Prior Evidence
This is actually nothing really new. For a review on the background behind the theory you can read The potential of nitric oxide releasing therapies as antimicrobial agents. While we think of iNO as being a drug for pulmonary hypertension it has other capabilities. It can diffuse across cell membranes and damage pathogens by causing nitrosative and oxidative damage. The amount of iNO needed though to accomplish this bactericidal action is much higher than the typical levels of 20 – 40 ppm that we use. Last year in August Bogdanovski et al published Antibacterial activity of high-dose nitric oxide against pulmonary Mycobacterium abscessus disease. They describe a protocol of providing 30 minute doses of 160 ppm for 21 days in a 24 year old patient with cystic fibrosis who was infected with mycobacterium abscessus. While they were not able to eradicate the organism, they were able to demonstrate functional improvement in the patient. Also notable was the absence of adverse effects in terms of methemoglobin levels. Other prior research in-vitro has shown iNO at high levels to be truly bacteriocidal as per the review above.
Can iNO kill COVID19?
There is work being done at the moment on a trial of nasal sprays of iNO to eradicate COVID19 infection. It shouldn’t be surprising then to see other work being done in the field and one such report came out in November 2020 entitled Rescue Treatment With High-Dose Gaseous Nitric Oxide in Spontaneously Breathing Patients With Severe Coronavirus Disease 2019
In this paper they describe the use of iNO at 160 ppm in 5 spontaneously breathing patients with confirmed COVID19 infection. This was provided as a rescue therapy in the absence of any high quality therapies for this disease. The protocol was to give them the same dose of 160 ppm for 30 minutes at a time until resolution of their symptoms with those that received multiple treatments getting anywhere from 5-9 courses. In each case after each 30 minute period the treating physicians measured levels of methemoglobin and nitrogen dioxide and found in each patient acceptable levels after these brief exposures.
Results
Of the 5 patients treated 2 died from COVID19 and three survived. The two patients who died interestingly were the ones who each only received one treatment each. The other three received 5, 8 and 9 treatments respectively. The authors recorded mean arterial pressure, heart rate, respiratory rate, SpO2/FiO2 and finally measurements of inflammatory markers in the two patients who died (E) and the 3 who survived in (F) in the figure below.
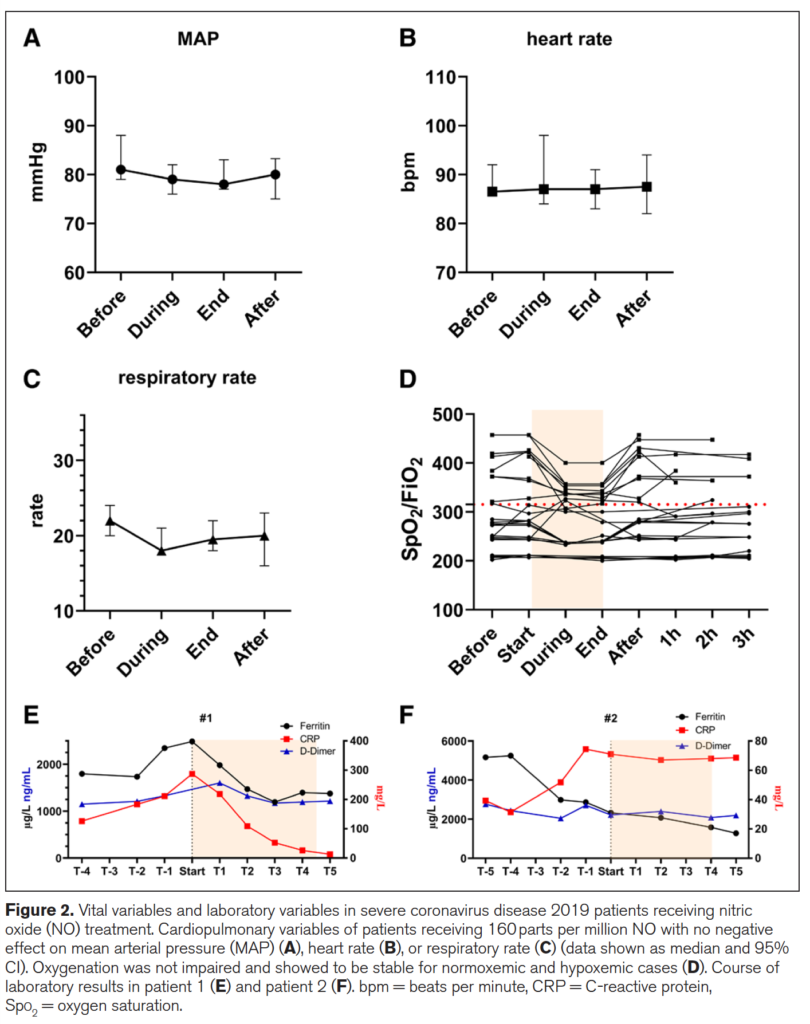
What is interesting from the figure above is the reduction in respiratory rate during treatment (certainly could be placebo from believing they will get better) but the oxygenation during the treatment improved as well. Could this be from a reduction in associated pulmonary hypertension? Certainly could be. Looking at the patients who died in (E) vs the ones in (F) who survived (patient 3 not shown) demonstrate that use of iNO stopped the rise in CRP and in the case of those who died reduced it significantly. There could be an argument made then that the changes in respiratory pattern observed during treatment are associated with a concomitant attenuation of inflammation. This treatment just might work but of course needs far more studies to be certain of that. On that note a review of iNO for this type of indication reveals there are currently 16 studies enrolling in this area of research so I imagine there will be more info to come with this story.
What about the neonate with pneumonia?
I sent this paper around to my colleagues and it generated some great discussion. I am no Ethicist but the question raised was could this be considered a “last ditch” treatment for the neonate succumbing to a pneumonia? I have no doubt if you are reading this that you will have seen in neonatal units around the world that there are infants who develop pneumonia unresponsive to traditional treatments such as iNO at regular doses, antibiotics, higher PEEP, surfactant etc. If we have this knowledge with respect to the potential use of iNO at high dose and a positive impact on pulmonary infective disease is this something that should be offered to parents?
We have no date to my knowledge in babies on the use of this type of dosing but it comes down to a question of what is the alternative? If a patient is dying on the ventilator are we at the point of knowledge here that it is worth offering the family this treatment? One could do so with full disclosure about the lack of neonatal data both for effectiveness and safety. Or do you fall on the side of it could be harmful and expedite death so should not be used. If you use it though and wait till the patient is in extremus on 100% oxygen might it be too late? Do parents have the right to know when they ask the question “is there anything else you can do?” For me I think the answer is that there should be a discussion with this evolving research out there. I am comfortable with it as long as the parents understand the potential for it to make things worse and shorten their time with their child. Alternatively if they choose not to that is their prerogative but should they have the choice when the competing outcome is death?
I can’t tell you whether you should or shouldn’t offer this in your institution but my suspicion is that you will be discussing this among colleagues before long. Who knows you might just one day say you saw it here first!
Thanks John M for the inspiration and keep sending those articles!

