The Canadian Pediatric Society has a statement on the use of premedication before non-emergent intubation which was written in 2011 and reaffirmed in 2018. After reviewing available medications for use the recommended strategy was atropine, fentanyl and succinylcholine. This combination does involve three different medications, the first being to prevent bradycardia, the second to sedate and the third to paralyze. With the use of three medications however there is always room for error so it is very alluring to try and use one medication to provide optimal conditions for intubation. As a matter of fact I once tried thiopental as a single agent as a fellow (unpublished) which never saw the light of day due to difficulties with recruitment. Nonetheless I was after a simpler solution to providing good conditions for intubation so it is not surprising that others are also looking at single agents as well.
Propofol Would Seem Like a Good Contender
Propofol has been used in the adult and Pediatric world for some time. It causes a decreased level of conciousness and amnesia surrounding the events for which it was given. It is short acting often wearing off within minutes which would seem perfect for procedural sedation. On the downside one of its side effects is hypotension so in a fragile neonate this might be something to be watch for.
Dose finding study
de Kort et al published Propofol for endotracheal intubation in neonates: a dose-finding trial this month. It is an interesting study design for those unfamiliar with dose finding studies. The goal was to begin with a low but starting dose for propofol at 1 mg/kg/dose and escalate by 0.5 mg/kg/dose until adequate sedation was reached WITHOUT signficant adverse side effects. Moreover the authors built on previous work in this area to attempt to break the patients into 8 groups as shown in this figure.
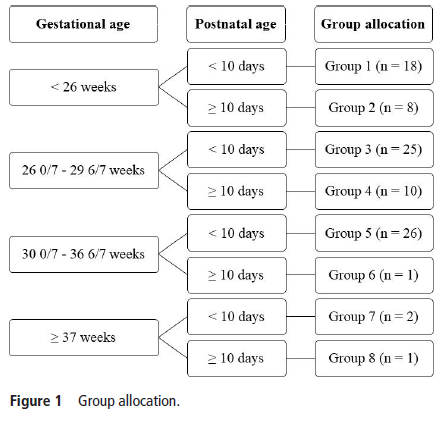
All patients were less than 28 days so allocation was based on gestational age and whether a patient was greater or less than 10 days of age at dosing. Level of intubation readiness was evaluated using a standardized tool called the Intubation Readiness Score.
Side effects were hypotension, myoclonus,
chest wall rigidity, persistent respiratory and/or circulatory failure and bronchospasm. Blood pressure was assessed via an indwelling catheter if available or by cuff if not available. Importantly any mean blood pressure after provision of propofol less than the gestational age met the criteria for declaring hypotension.
The Findings
The study was terminated early due to low inclusion in some groups after 91 total patients had been enrolled. In the end there were only enough patients in Groups 3 (26 – 29 weeks and <10 days) and 5 (30 – 36 weeks and < 10 days) enrolled to analyze fully. The results of the dose finding analysis are shown below.
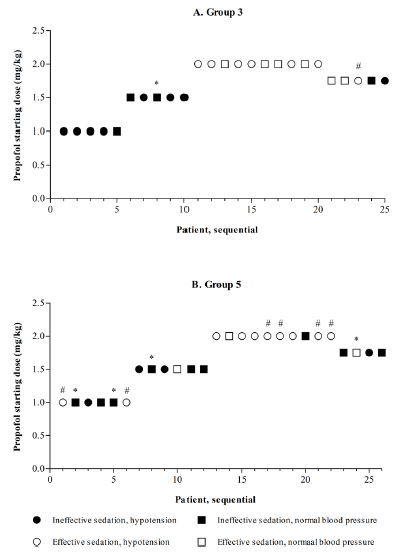
Walking through group 3, there were 5 patients enrolled at the 1 mg/kg level and based on poor levels of sedation in all the dosing for next 5 were increased to 1.5 mg/kg. As intubating conditions improved, the authors found that at a dose of 2 mg/kg while conditions were optimal, hypotension became a significant problem with 59% being hypotensive. The management of hypotension included 54% needing volume resuscitation and inotropes in 10%. Curiously the hypotension often did not appear until 2 hours or more after drug delivery. When the authors did a step down to 1.75 mg/kg as a intubation dose they found it was inadequate for providing good conditions for intubation albeit with less hypotension.
Not the right drug
The goal of this study was to find the optimal dose that provided good intubation conditions without significant side effects. The strength of this study was that it included babies across a wide range of gestational ages from 26+0 to 36+6 weeks gestational age. While the authors were unable to recruit enough patients to fill each group the stoppage of the study made sense as it was clear that the goal of the study would not be met. Propofol would be a great single agent if it weren’t for the issues found in this study. This is not to say that the drug is a poor choice for Pediatrics but in the Neonatal world I just don’t think it has a place. I would welcome further testing on other single agent drugs but that of course is an analysis for another post!