If you have had a baby born prematurely and are reading this blog post you may have been told that the medical team is looking for a PDA. The PDA stands for Patent Ductus Arteriosus and the last two words Ductus Arteriosus really helped your fetus as it was growing in the womb. In order to understand how it can cause a problem after birth it is first important to understand what it did and why it exists in the first place.
Act I – The Womb
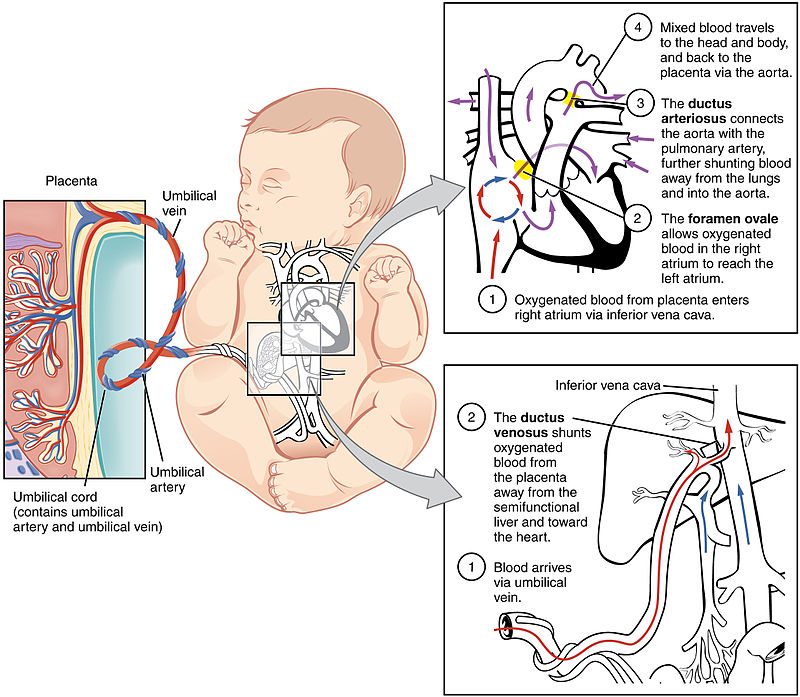
When your baby was developing its lungs the tissue was busy branching into airways that ended in little air sacs called alveoli. Each of those alveoli was next to a capillary which is our smallest blood vessels in the body. One day these units (alveolus and capillary) will happily exchange oxygen that is breathed in for carbon dioxide that needs to be breathed out. In the womb though the lungs were filled with fluid and air was nowhere to be seen. As such, most of the blood (about 90%) that came back from all the veins in the body to the right side of the heart had no business going to the lung. There was just not really any point in sending blood to the lung when it couldn’t pick up any oxygen there. The fetus by having a ductus arteriosus had a “pop off valve”. Since the pressure in the lung was high instead of sending blood to the lung, the 90% went from the right ventricle in the lower part of the heart to the pulmonary artery and from there across the ductus arteriosus to the aorta. The blood following this path therefore basically bypassed the lung and went from the “right” side of the heart to the “left” side that normally sends blood with oxygen to the rest of the body. The oxygen in this case came from the placenta. This fetal ciruculation is shown in the figure below.
Act II – Life on the outside
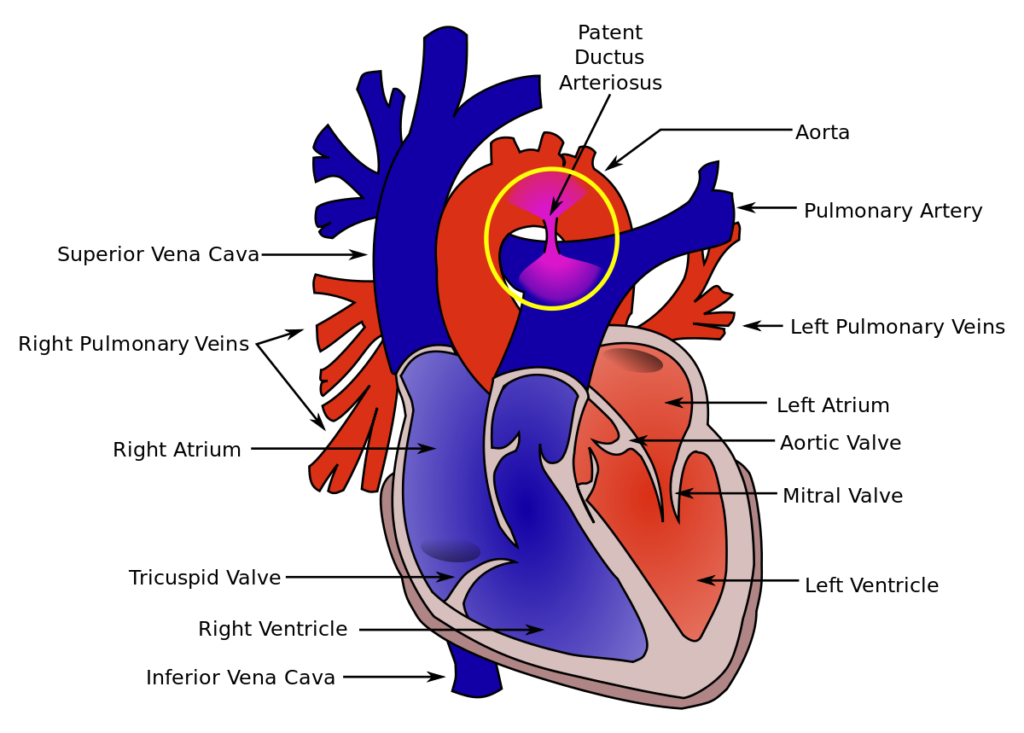
After birth the lungs fill with air containing oxygen and the resistance to blood flowing into the lung decreases which is a good thing as it allows oxygen to move from the alveolus to the capillary and back to the left side of the heart. As oxygen in the blood stream rises this usually leads to closure of the ductus arteriosus. In preterm babies though the ductus may not shut and this is what we call a Patent Ductus Arteriosus or PDA. This becomes a problem when the blood pressure in the aorta is high and the pressure in the lungs falls with breathing of air. Eventually, instead of the right to left flow of blood that occurred before, you now get blood flowing from the aorta to the pulmonary artery going to the lung and as more and more blood flows to the lungs they start to look white on chest x-rays and it gets harder and harder for your baby to breathe. The mixing is shown below.
Act III -So what do we do about it?
If we suspect that there is a PDA your doctor will order a test called an echocardiogram. This is an ultrasound of the heart and may be done by a specialist in the heart called a Cardiologist or may be done by a Neonatologist trained in doing such tests. Either way if the doctors believe the PDA is causing problems they will suggest a treatment plan to deal with it. The problems that would tend to motivate us to treat would most commonly be that your baby is needed support to help their breathing although problems related to poor blood supply to the kidneys might also lead us to treat.
The mainstays of treatment are two very common drugs and one that you may not have heard of. Indomethacin is a drug that was first used to help close PDAs and is a non steroidal anti-inflammatory (NSAID) drug that is in the same class as ibuprofen (advil) which is another drug that is used. In some centres another very common drug acetaminophen (tylenol) is employed. Most centres at this point are using one of the first two. Regardless after the medicines are given the doctors will order another echocardiogram to see if the PDA has closed and if not may repeat a course of the same medicine or choose a different one.
Act IV – What do you do if it just won’t close?
The next steps depend on how your baby is tolerating the PDA. If your infant is breathing on their own and their kidney function is working well many doctors will just observe and not offer more treatment. Babies though who are on a ventilator or are having significant issues related to their kidneys may rarely need to have a surgeon put a clip on the PDA to close it. These days this is quite rare and there are some centres that choose to not treat the PDA with medicine or surgical closure at all and just wait it out until they are gone. Almost 90% of them will close on their own if you leave them alone but again it depends on how sick your infant is in order to determine if this is reasonable.

