If you have been following this blog for awhile you may recall a post from a couple years back on Physiological based cord clamping. The premise of that paper was that rather than arbitrarily choosing a time to clamp the cord, one should look for the following three features that indicate adequate pulmonary blood flow has been established:
1. Establishment of adequate breathing(average tidal volume > 4 ml/kg) on CPAP – using a mask capable of measuring expired volumes
2. HR above 100 BPM
3. SpO2 above the 25th percentile using an FiO2 <0.4
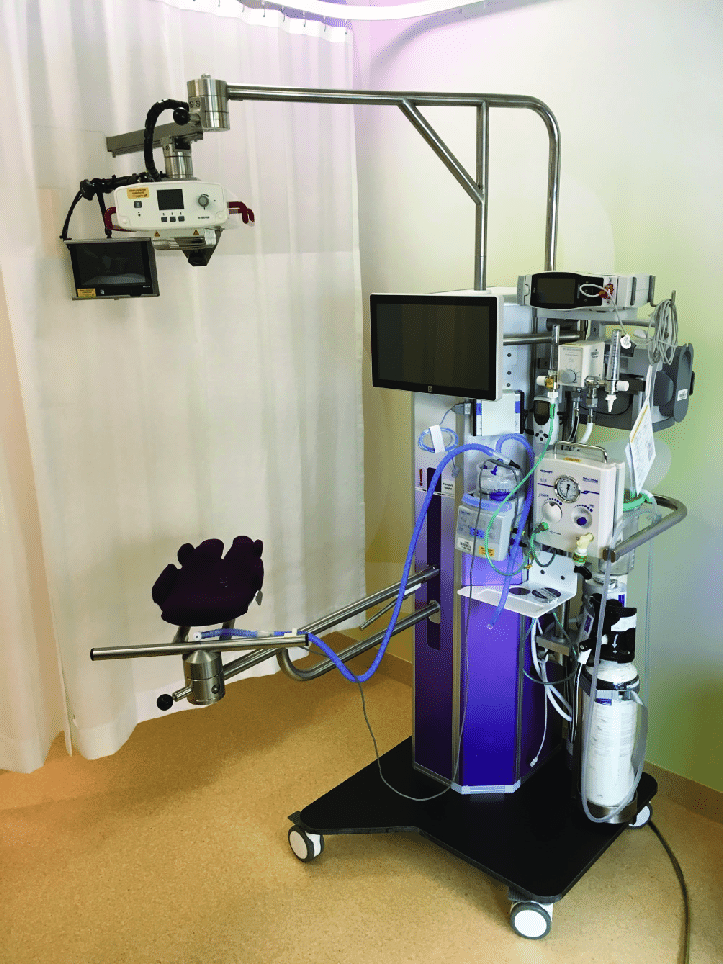
In the original trial it was a proof of concept design that sought to determine if resuscitation on their “Concord” table was feasible and how long would it take for the above criteria to be met so the cord could be clamped.
The mean time for cord clamping in that trial was 4 minutes and 23 seconds. This is much longer than the typical delayed clamping of 30 -60 seconds and even longer than the few studies that have looked at delays of 1- 3 minutes.
The Next Phase
The same group now sought to compare DCC of 30 – 60 seconds with the PBCC approach for infants <32 weeks gestational age in the paper Physiological-based cord clamping in very preterm infants – Randomised controlled trial on effectiveness of stabilisation. This trial was set up as a non-inferiority trial to see if the pre-defined difference in time to stability of 75 seconds would be crossed. A power calculation was performed that indicated the authors would need to recruit 64 infants with 32 in each arm. Due to poor recruitment the authors chose to stop the trial early with only 17 infants in the DCC group and 22 infants in the PBCC arm. An analysis with those patients identified that the non-inferiority limit had been met already.
Difference in resuscitation
Infants randomised to the DCC group had their cords clamped at 30-60 seconds and had their resuscitation started on a resuscitation table. Infants in the PBCC arm were placed on the Concord after delivery and had their resuscitation performed there. Care afterwards would have been similar.
They found that the mean time to stabilisation was 5:54 +/- 2:27 in the PBCC group and 7:07 +/-2:54 in the DCC groups. The mean difference was 1:19 min (95% CI -3:04 to 0:27 min). The results clearly demonstrated a finding of shorter time to stabilisation in the PBCC arm as shown in the figure.
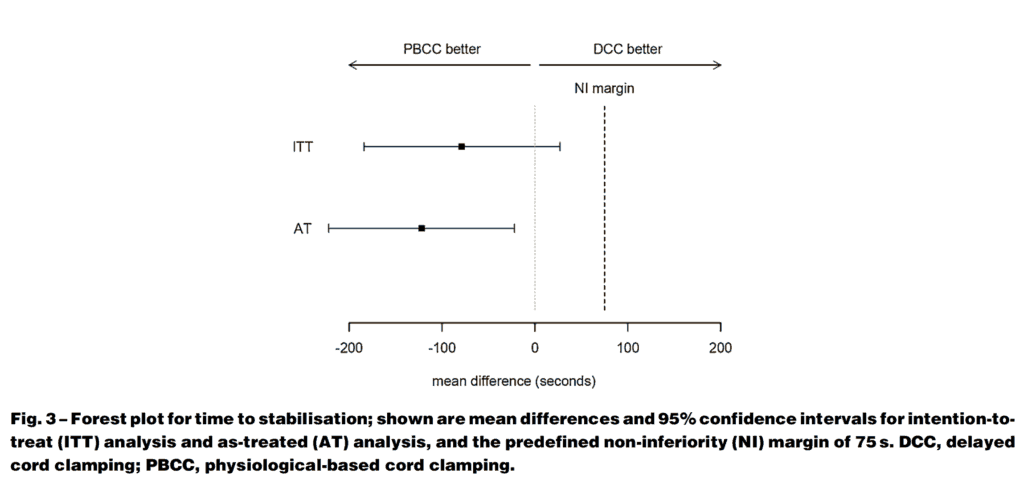
As the confidence interval crossed 0 though in the intention to treat analysis we can say that PBCC is no worse than DCC but can’t say it is superior as a strategy overall. Perhaps larger numbers may have shown something different but at least we know it isn’t worse.
Other Findings
One thing that I would imagine Obstetricians would be concerned with here is the potential for significant blood loss since uterotonics were not provided until the cord was clamped which in PBCC was quite a bit longer, Opposite to what one would have expected the mean blood loss in the DCC group was 450 mL compared to 300 mL in the PBCC arm. Not different statistically though given the small numbers.
There were almost twice the number of females in the PBCC group which could account for some of the findings here. Another difference worth noting was that respiratory support was initiated earlier on the concord than on the standard resuscitation table which the authors acknowledge may be due to familiarity with doing so from experience with the specialized set up. Earlier ventilation (1:11 min vs 2 min in the DCC) could indeed lead to earlier reaching of the end points of the stabilisation criteria.
Regardless of the last couple points, what is needed now is a much larger study to look at clinical outcomes. The numbers were so small here to really examine such clinical points but this is where I believe we are now headed. If the pattern continues I guess we will see another study coming from this group in a couple years so stay tuned!

