British Columbia COVID-19 Documents
The most up to date documents can be found here: British Columbia COVID Resources

The most up to date documents can be found here: British Columbia COVID Resources
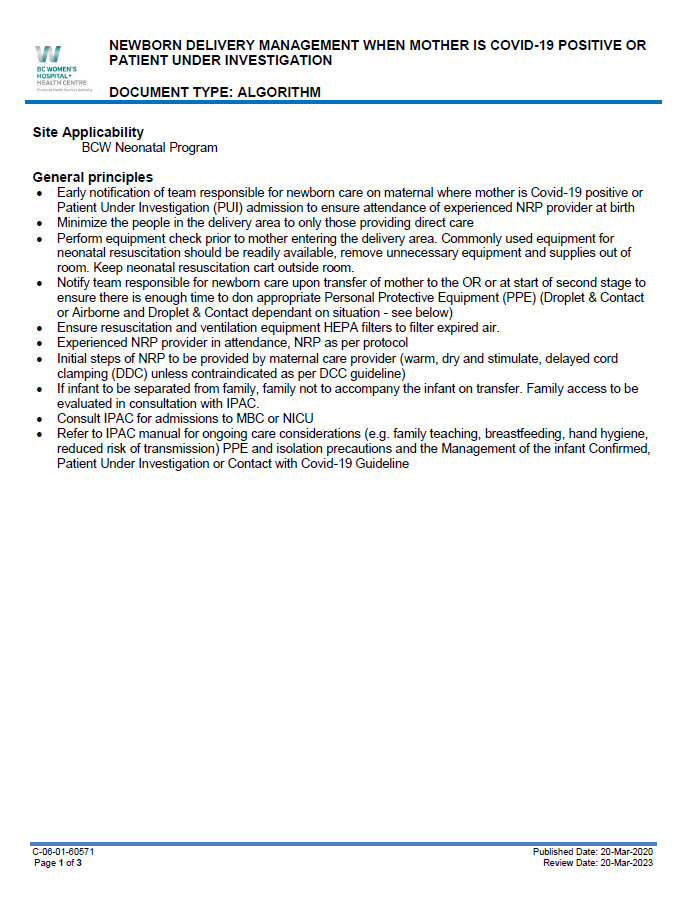
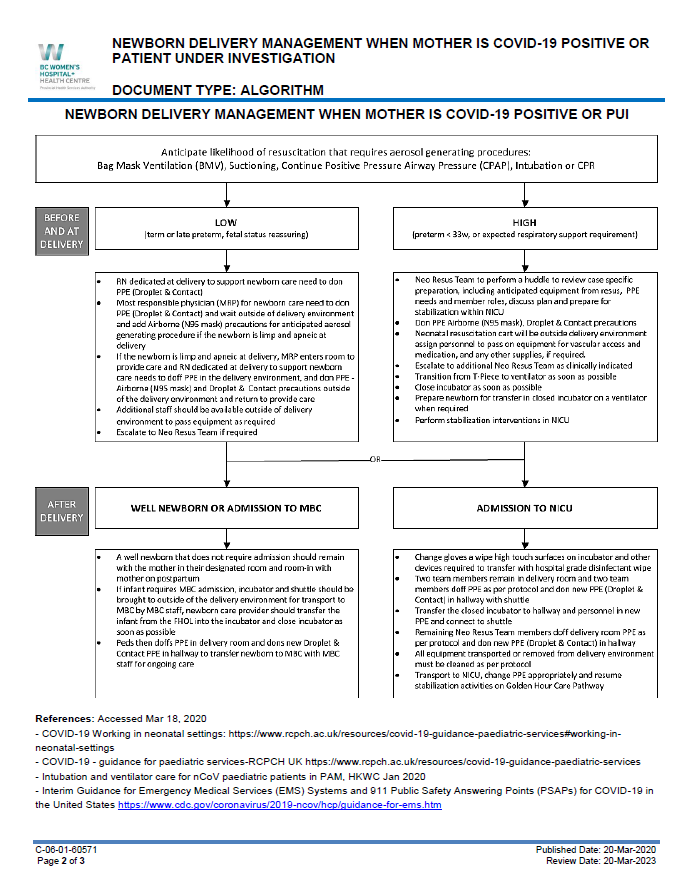
We are living in challenging times but, as a community caring for neonates and their families, we will get through this together. Canadians and others around the world are digesting a great deal of information in order to come up with a best approach to caring for mothers and infants with either suspected or confirmed COVID-19 infections. It is an imperfect science for sure as we have scarce information to go on but you may find it helpful to look at what centres are doing in terms of their approaches to delivery and care in the NICU. Please note that these are being posted in an attempt to share our collective efforts but that referral to your local health authority protocols is recommended.
Protocols and other relevant information including sim/ education and processes can be shared from sites across Canada and accessed through the COVID-19 menu at the top of the site.
There will no doubt be geographic differences which may be due to unit layout (single/double rooms, open bay concept, negative pressures rooms), local IPC and health authority protocols. Hopefully, though, our community can share useful resources, algorithms, videos, etc that can serve as a framework for others to use or modify to suit their needs.
Thanks to all of you for your dedication, your hard work and for your caring. Please stay safe and stay healthy – we will get through this – together.
Ontario “Provincial Council for Maternal and Child Health – Covid 19 Practice Support Tools

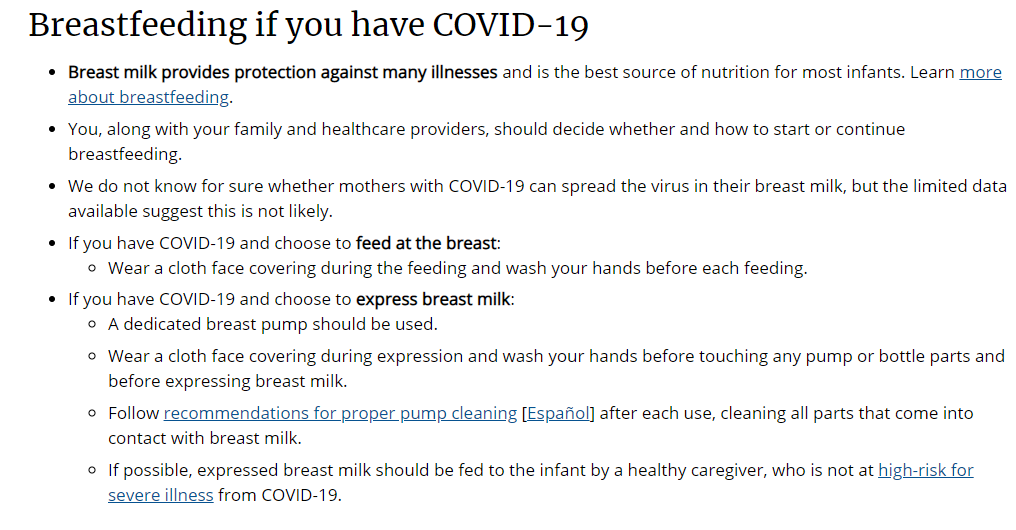
This is another hot topic out there as centers around the world struggle to determine how best to manage the mother who has contracted COVID-19 in pregnancy. There are resources out there already such as the CDC which states the following.
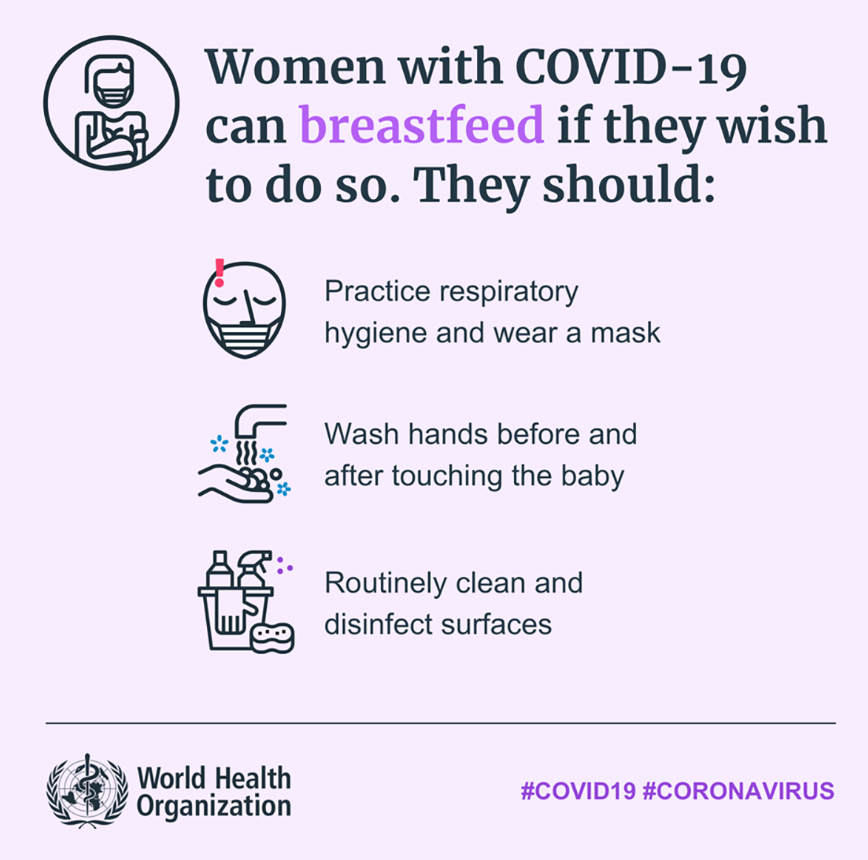
The World Health Organization on the other hand has this to say as of yesterday.
The question though is where do these recommendations come from? How strong is the evidence and what do you do when two very large trusted organizations don’t seem to be on the same page?
Do you remember SARS? This was another coronavirus.
Wong SF et al published Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome in 2004 in which they described the outcomes of 12 women infected with the coronavirus causing SARS. In this study they sampled Evidence of perinatal transmission of virus was assessed by SARS-associated coronavirus reverse-transcriptase polymerase chain reaction (SARS-CoV RT-PCR) and viral culture on cord blood, placenta tissue, and amniotic fluid at or after delivery. None of the tested infants were found to have infection nor were any of the tissues or fluids positive. They did not test breast milk specifically but as none of the infants developed SARS one could infer that if the other samples were negative so were the breastmilk samples. The conclusion after the SARS epidemic is that vertical transmission does not occur.
It may surprise you but there is very little out there on breastmilk and COVID-19. Having said that, there is very little data on pregnancy and COVID-19 so the question then is how strong is the evidence for lack of transmission in breastmilk?
There is really one study by Chen H et al Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The authors looked at 9 women presenting in the third trimester and examined outcomes from pregnancy. All of the infants were delivered via c-section and in 6 of the 9 samples of breastmilk were obtained and sampled for COVID-19. The good news was that none of the samples tested positive for the virus.
I suppose the result shouldn’t be that surprising as the virus causing SARS is similar and also has not been demonstrated to lead to neonatal infection. The question then is whether one should freely breastfeed their newborn if they are known to be positive for COVID-19.
Getting back to the earlier recommendation from the WHO, it reads as pretty firm. Looking at the sum total of evidence I think it is safe to say we don’t have a lot of data to go by. What we have though in this situation is to look at risk/benefit. To the best of our knowledge, COVID-19 is not transmitted into the fetus and after birth does not get into breastmilk. Both of these things appear to be quite good but as the virus spreads and more pregnant women contract the virus we may see as we get a larger sample that it is possible but I suspect this is a virus that simply doesn’t transmit to breastmilk. What if we banned breastfeeding in suspect or confirmed patients? The potential loss of immunoglobulins against COVID-19 is a real risk for the infant as they continue to live in the same home as the mother. How do we know that such antibodies exist? As for as I know for COVID-19 this hasn’t been proven yet but in the SARS epidemic a case report demonstrated that antibodies against this virus were indeed in breastmilk; SARS and pregnancy: a case report. Given that the viruses are part of the same class I would imagine the same would hold true with the new coronavirus. They may not be born with the virus but if they are receiving passive immunity from the mother that needs to be considered given that we have nothing effective (at the moment) to treat anyone. An alternative is to use donor breast milk but if we go down that road, our supplies will be exhausted before long. Weighing everything and using the best data we have at the moment my bias would be continue breastfeeding albeit with the recommendations for droplet precautions and hand hygiene as the WHO suggests. In that way, the recommendations from the CDC seem more measured. Having said all of that everything these days is subject to change.
Stay safe out there everyone.

This week on social media this seemed to be a hot topic. What should we do to protect ourselves as we start to see more mothers infected or at least suspected of having COVID-19
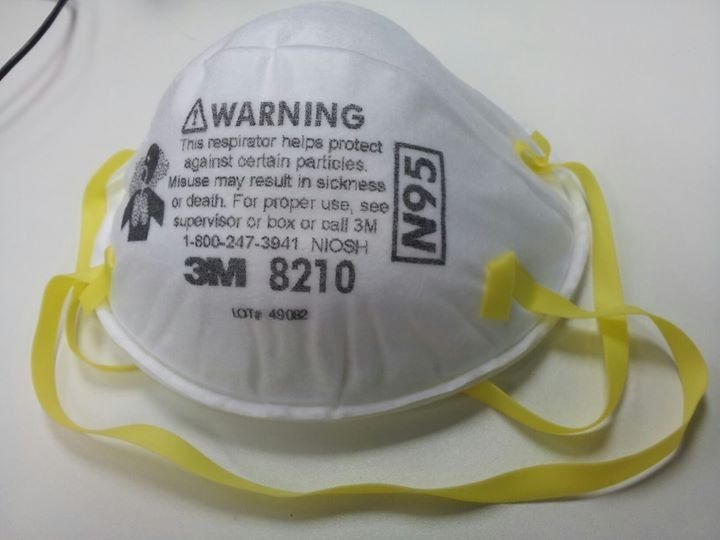
presenting in labour. Should we be assuming all of these infants are infected and if so should we all don personal protective equipment (PPE) including the N95 mask? Let’s see what we know so far.
The big concern with this began after a report of a 36 hour old newborn in China contracting the virus. This was published in Clinical Infectious Diseases in the paper A case report of neonatal COVID-19 infection in China. As the authors point out in this paper it is difficult to determine if the baby was born with the infection or was seeded with virus at birth and then tested positive at that point. This story made the news and sparked a lot of questions about whether newborns could be infected.
The latest story to hit the news though is more worrisome as it leaves little to the question of when the infant was infected. Newborn baby tests positive for coronavirus in London from the Guardian as well as other sources publicized that a newborn who was swabbed within minutes of birth tested positive. This is enough to strike fear in just about everyone but there are questions that need to be answered before panic can set in. There really are little if any details about this patient. Were they symptomatic or was a nasopharyngeal swab positive for the virus alone? While it is tempting to link the infected newborn with transmission from amniotic fluid, there are other sources of virus such as blood and stool that can be present at delivery from the mother than could have yielded the positive result.
Bear in mind the data is sparse but here is what we know about amniotic fluid thus far. In a recent paper in the Lancet entitled Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. some good information was found. It is important to note that all of the infants were born via c-section so the issue of potential contamination by stool or blood was greatly reduced. All of these women had their amniotic fluid sampled and all nine tested negative for the virus. Yes I realize nine samples does not totally guarantee that virus cannot be transmitted into amniotic fluid but it is certainly reassuring as they were pure samples. Also notable was that none of the babies in the study presented with any symptoms of respiratory distress.
Additionally another recent paper Infants Born to Mothers With a New Coronavirus (COVID-19) in Frontiers of Pediatrics demonstrated no neonatal infections in the three infants whose parents consented to testing for COVID-19. Presumably their amniotic fluid was free of virus as well.
In the twitter world this week there was much discussion about this issue. To use PPE including an N95 mask or not. I would love to tell you what you should do but that is up to your own institutions and their risk tolerance. While the media can certainly sensationalize things (and these two cases above haven’t helped stop that), the evidence would suggest at this time that these newborns are not born infected for the most part. One of the issues though is sample size for sure. How many pregnant women with COVID-19 have there been to this point? Hard to say especially since not every person can be tested. For the time being though my bet is that these babies are not born viremic but may be contaminated at birth. How long the virus takes to grab hold of the newborn and possibly cause disease is a different story altogether. Once a baby is in an NICU and develops symptoms our approach must be more cautious.
We will have to see where this all goes but be careful out there.

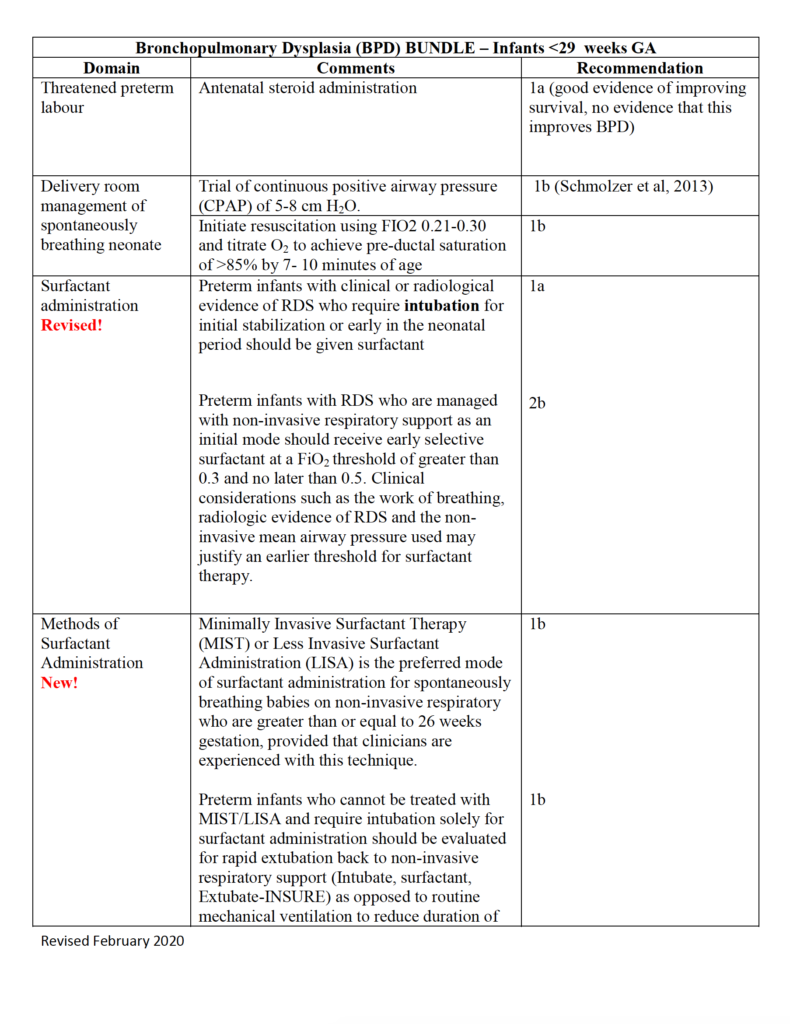
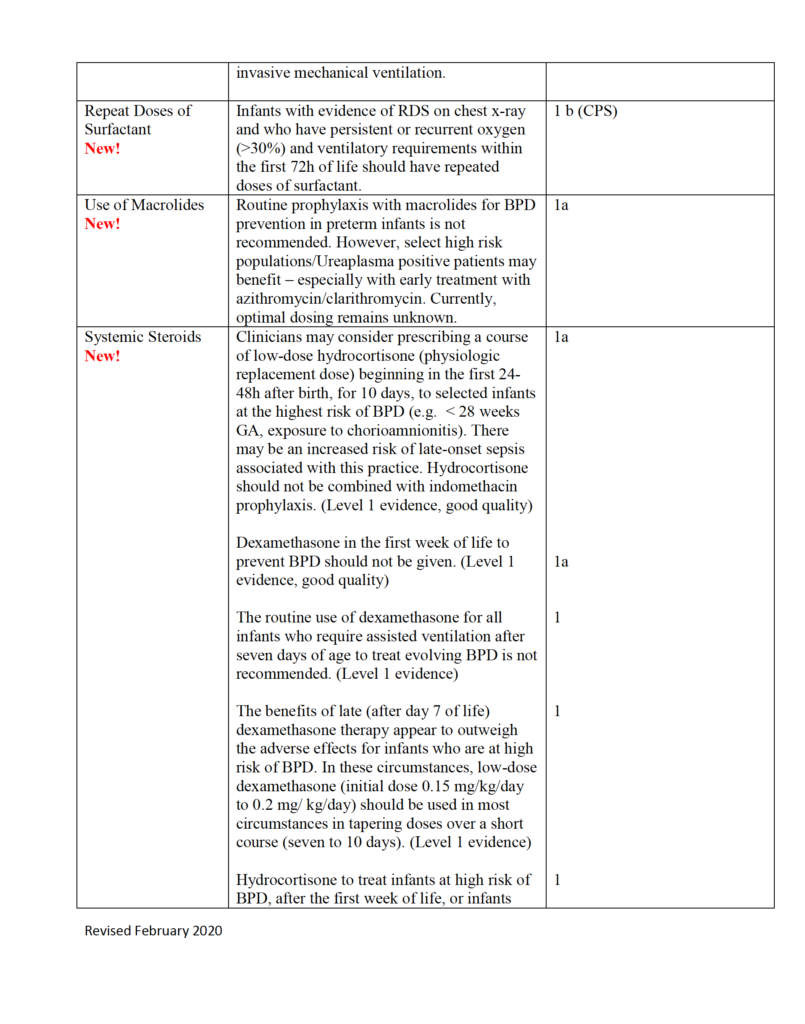
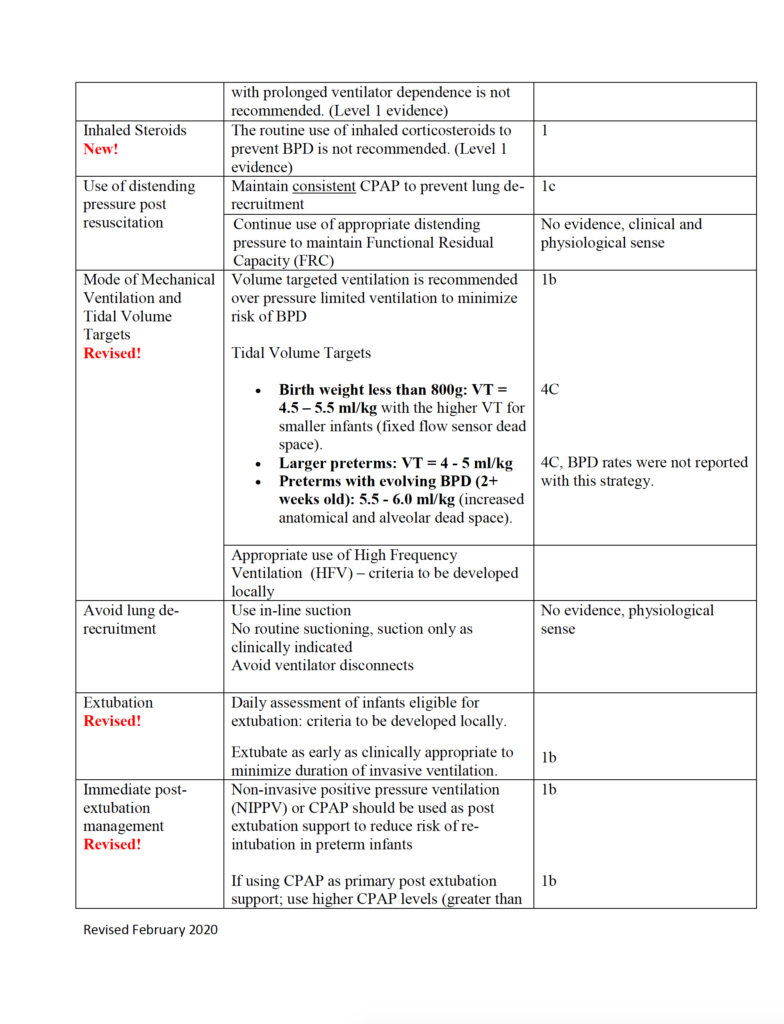
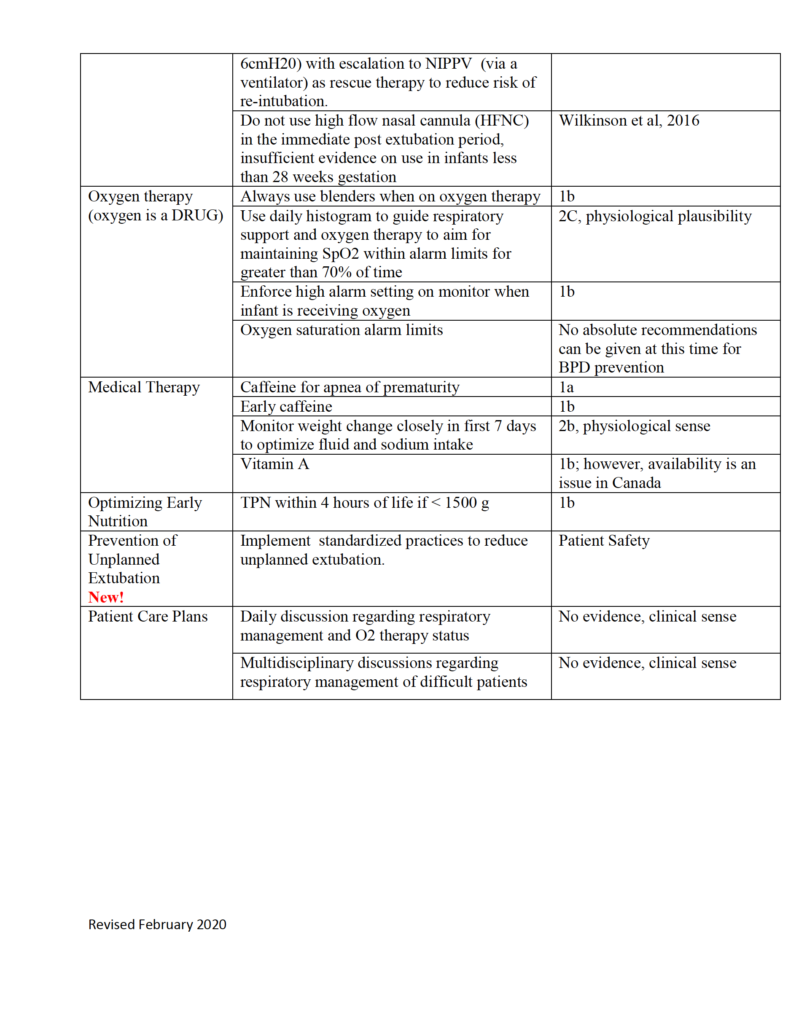
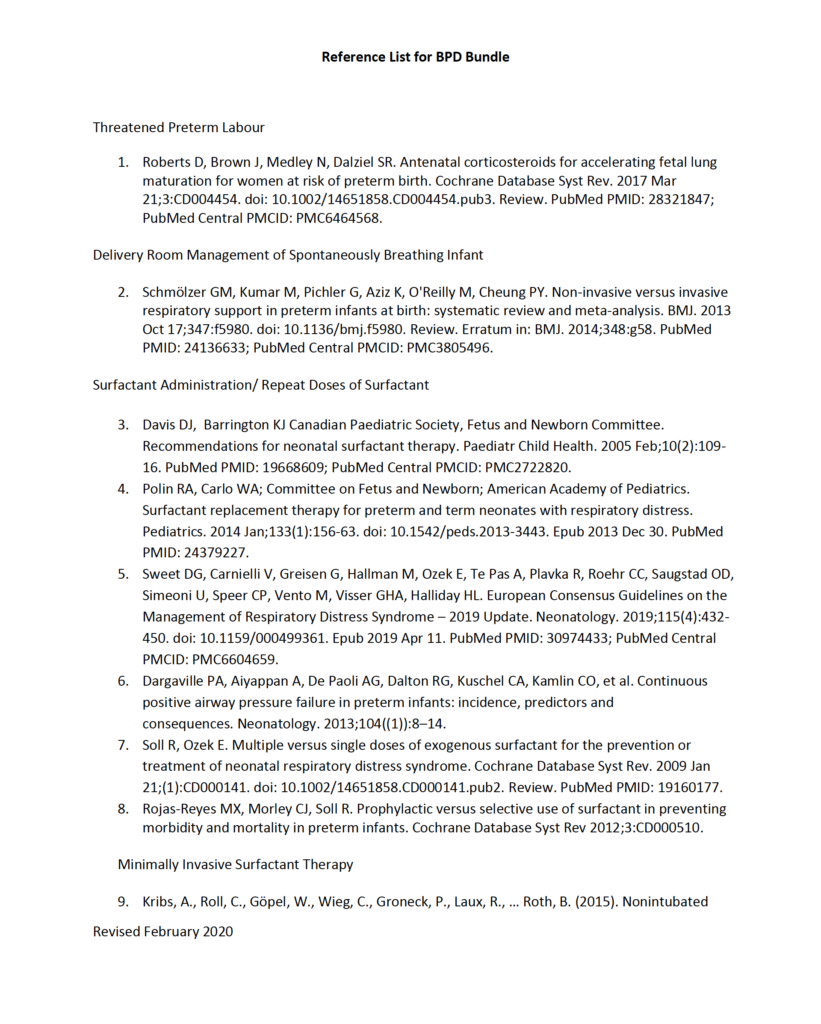
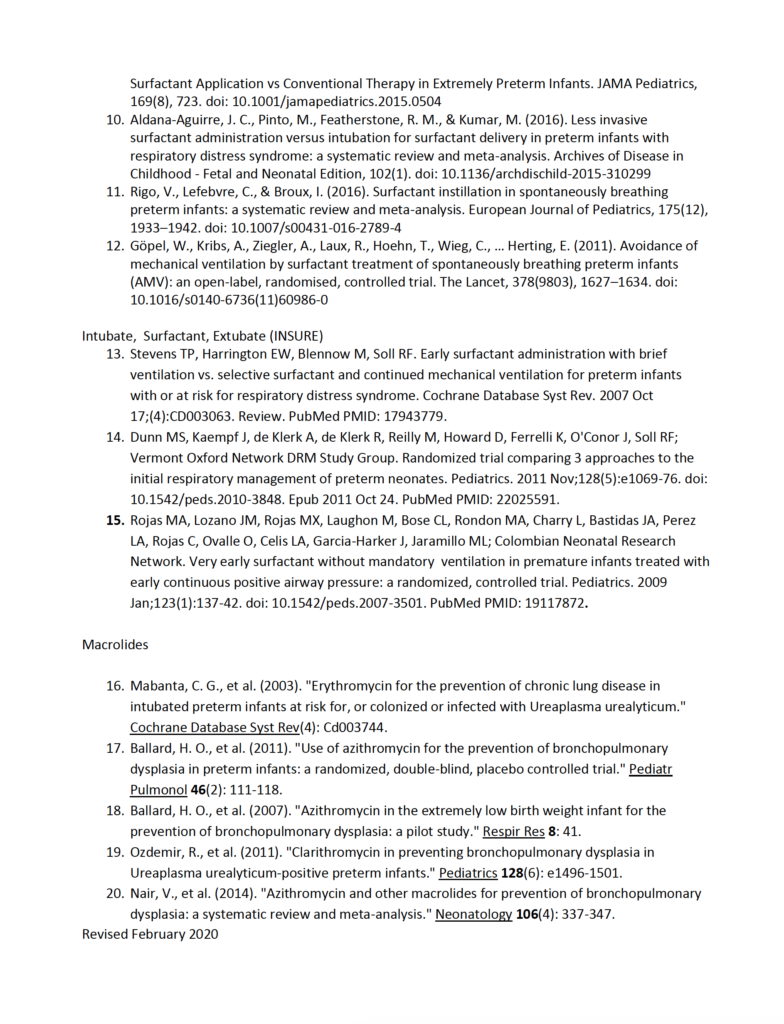
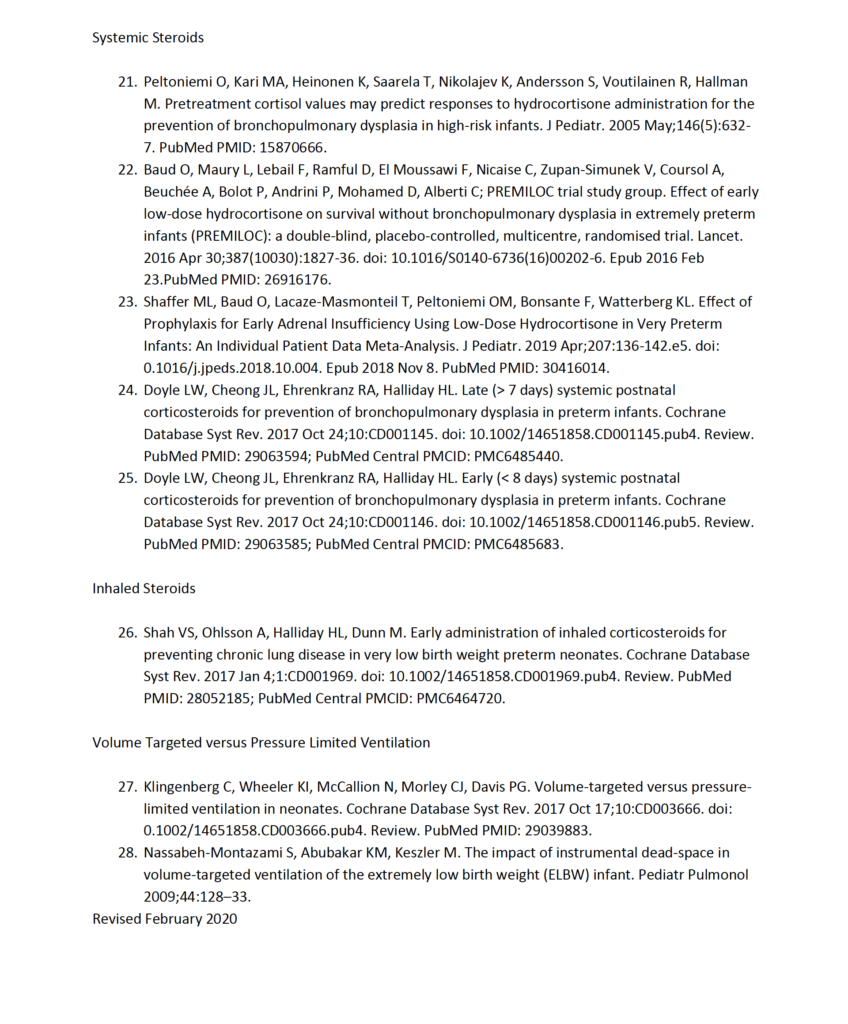
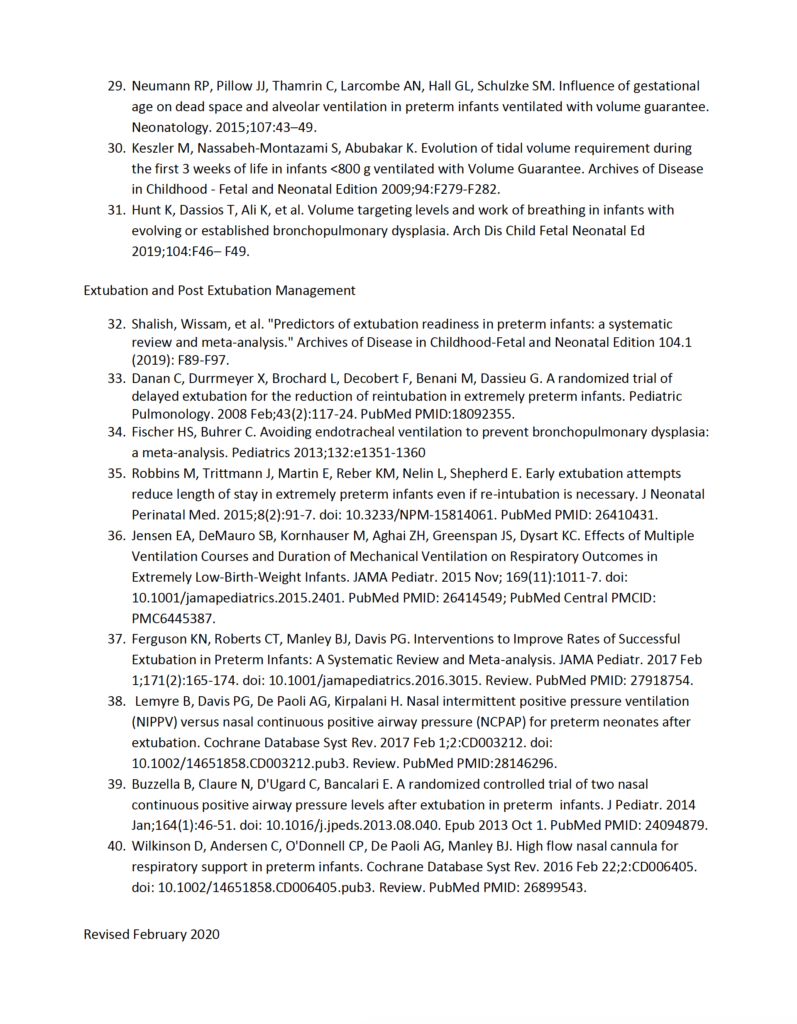
Evidence-based Practice for Improving Quality or EPIQ is a collaborative group here in Canada that is producing incredible work to examine the evidence to come up with the best approaches for treating conditions. One such target has been bronchpulmonary dysplasia or BPD. I was sent a document recently summarizing this work and thought it was definitely worth sharing with the masses.
Especially as we are all locked in somewhat with the expansion of COVID-19, a post on a lung disease seemed apropos. Our babies keep being born and with some preterm and at risk of developing BPD, what can you do to try and prevent this condition and moreover if an infant has developed it, what can we do to limit its severity and begin the healing phase?