This has been a question that has befuddled Neonatologists for years. Get ten of us in a room and you will get a variety of responses ranging from (talking about caffeine base) 2.5 mg/kg/day to 10 mg/kg/day. We will espouse all of our reasons and question the issue of safety at higher doses but in the end do we really know? As I was speaking to a colleague in Calgary yesterday we talked about how convinced we are of our current management strategies but how we both recognize that half of what we think we know today we will be questioning in 10 years. So how convinced should we really be about caffeine?
Even the Cochrane Review Suggests There Is Something Amiss
Back in 2010 the Cochrane Collaboration examining 6 trials on caffeine for treating apnea of prematurity concluded “Methylxanthine is effective in reducing the number of apnoeic attacks and the use of mechanical ventilation in the two to seven days after starting treatment.” Notice the bolded section. Two to seven days. Interesting that we don’t see the effect last in perpetuity. Why might that be? Do babies become resistant with time or is there a change in the way these infants metabolize the drug such that levels in the bloodstream drop after that time point. It is almost certainly the latter and in the last 7 years have we really seen any response to this finding? I would say no for the most part although I don’t work in your unit so hard to say for sure. At least where I practice we pick a dose somewhere between 2.5-5 mg/kg/day and give a load of 10 mg/kg when we start the drug. From time to time we give a miniload of 5 mg/kg and may or may not increase the dose of maintenance based on the number of apneic events the babies are having. What if we could be proactive instead of reactive though. Do the babies need to have multiple events before we act or could we prevent the events from happening at all?
Proactive Treatment With Caffeine
We have known that caffeine clearance increases with postnatal age. The half-life of the drug shortens from about a week at the earliest gestational ages to 2-2.5 days by term equivalent age. For those infants who are older such as 32 weeks and above we expect them to be off caffeine (if they need it) within 2-3 weeks so I am not really talking about them but what about the babies born earlier than that or certainly MUCH earlier at 23 and 24 weeks who will be on caffeine possibly till term. Should one size (dose) fit all? No it really shouldn’t and some crafty researchers led by Koch G have published a paper that demonstrates why entitled Caffeine Citrate Dosing Adjustments to Assure Stable Caffeine Concentrations in Preterm Neonates.
In this paper the authors armed with knowledge of the half life of caffeine at different gestational ages were able to calculate the clearance of the drug at different postnatal ages to demonstrate in a model of a 28 week male infant weighing 1150g. The authors further took into account predicted weight changes and were able to calculate what the expected caffeine levels would be in the fictional infant at various time points. The target caffeine levels for this patient were a trough level of 15 -20 mg/L which are the currently acceptable ranges in the literature. The testing was first done using a standard load of 10 mg/kg (base) followed by 2.5 mg/kg/d (base) and demonstrated levels which yielded the following graph over time. 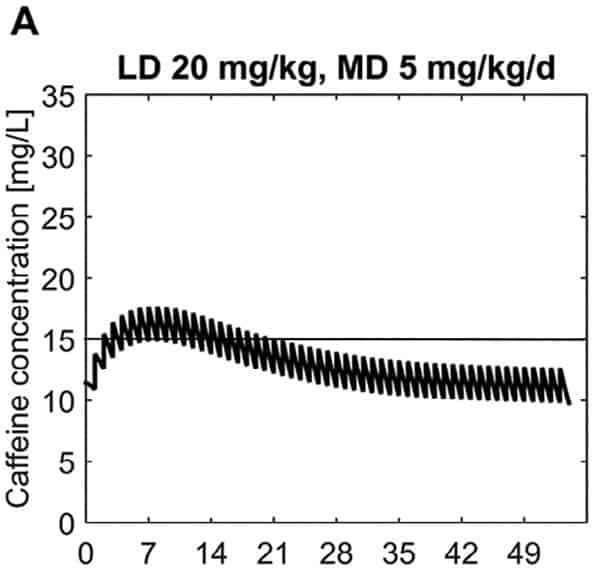 What this demonstrates is that if the dose is unchanged over the first 7 weeks, this hypothetical infant will only achieve effective concentrations for the first week. Interesting isn’t it that the Cochrane review found clinical effect over the first 2-7 days? What if you were to double the dose to really “hit” the infant with a good dose of caffeine from the start and maintain at that level based on their weight gain as shown next.
What this demonstrates is that if the dose is unchanged over the first 7 weeks, this hypothetical infant will only achieve effective concentrations for the first week. Interesting isn’t it that the Cochrane review found clinical effect over the first 2-7 days? What if you were to double the dose to really “hit” the infant with a good dose of caffeine from the start and maintain at that level based on their weight gain as shown next. 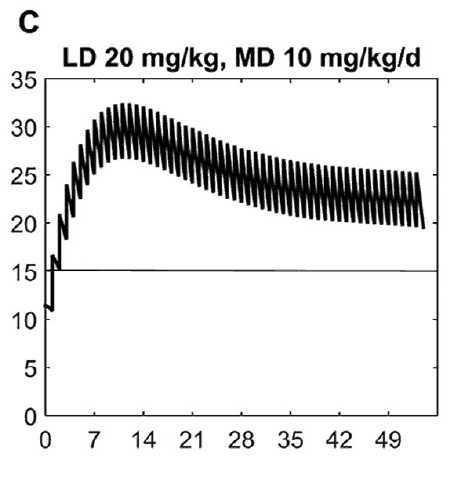 Well, you will get what you are hoping for and keep the trough level above 15 mg/L but you will hit 30 mg/L that some have said is too high and can lead to adverse effects (ever seen SVT with these high doses? I have). Like Goldilocks and the Three Bears could there be a dosing strategy that might be just right? The authors put in another model based on the knowledge of caffeine clearance over time and suggested a strategy in which after the first week the adjusted maintenance doses would be 3 mg/kg/day and 3.5 mg/kg/day in the third to fourth weeks and lastly 4 mg/kg/d in the 5th to 8th week. Using that dosing schedule the model produced this curve.
Well, you will get what you are hoping for and keep the trough level above 15 mg/L but you will hit 30 mg/L that some have said is too high and can lead to adverse effects (ever seen SVT with these high doses? I have). Like Goldilocks and the Three Bears could there be a dosing strategy that might be just right? The authors put in another model based on the knowledge of caffeine clearance over time and suggested a strategy in which after the first week the adjusted maintenance doses would be 3 mg/kg/day and 3.5 mg/kg/day in the third to fourth weeks and lastly 4 mg/kg/d in the 5th to 8th week. Using that dosing schedule the model produced this curve.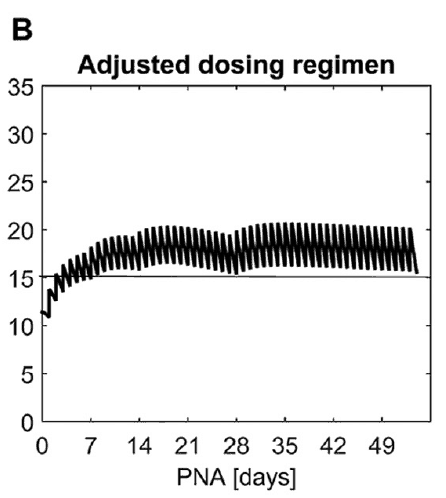 As you can see, the infant would have a therapeutic target without reaching levels above 30 mg/L and potential for side effects. As many of you read this however you may ask the obvious question. Each of us have seen infants who require higher doses than this to rid themselves of significant apnea and escape reintubation. Given that this is a mathematical model it assumes that this fictional infant will respond beautifully to a trough level of 15 to 20 mg/L but some will not. Even in the curve shown it is clear that there is some room to go higher in the dosing as the curve is just touching 20 mg/L.
As you can see, the infant would have a therapeutic target without reaching levels above 30 mg/L and potential for side effects. As many of you read this however you may ask the obvious question. Each of us have seen infants who require higher doses than this to rid themselves of significant apnea and escape reintubation. Given that this is a mathematical model it assumes that this fictional infant will respond beautifully to a trough level of 15 to 20 mg/L but some will not. Even in the curve shown it is clear that there is some room to go higher in the dosing as the curve is just touching 20 mg/L.
A Suggestion For The Future
What grabbed my attention here is the possibility that we could take a proactive rather than reactive approach to these infants. Once a small baby is controlled on their dose of caffeine whether it is 2.5, 3, 5 or even 6 mg/kg/d of caffeine should we wait for more events to occur and then react by increasing caffeine? What if we are too late to respond and the patient is intubated. What effect does this have on the developing lung, what about the brain that is subjected to bradycardic events with resultant drops in cardiac output and cerebral perfusion. Perhaps the solution is to work with our pharmacists and plan to increase dosing at several time points in the infants journey through the NICU even if they aren’t showing symptoms yet. No doubt this is a change in approach at least for the unit I work in but one that should start with a conversation!


I agree, proactive use may benefit these infants. We know from experience almost for sure apnia followed by some form of bradycardia will occur On preterm infants, on the same hand testing for caffeine levels need to be quickly available for the clinician so as to keep ahead of dosage needed.
Unfortunately at this time there does not appear to be a rapid turnaround for caffeine levels. It looks like about a week at best for getting results whether by blood or saliva
Dr Bancalari wrote some years ago in an editorial that caffeine use has shown a good therapeutic in prematurity apnea. Recent studies has shown also promising results with higher dose of caffeine. But, this promising results with caffeine therapy are resulting in liberalization of its use. He reminds in his editorial “of many therapeutic misadventures in the past because of adopting therapies before clear evidence of long term safety was achievied”.Bancalari. (Current management of apnea in premature infants: is caffeine the magic bullet? Early Hum Dev. 2014 Sep;90 Suppl 2:S1-2. doi: 10.1016/S0378-3782(14)50001-1.)
What is your opinion about this?
I am a pediatric ophthalmologist who does ROP screening in Argentina. In the units in which caffeine is used from the first day of life, the incidence of ROP has decreased in extreme preterm infants.
After the first week of life some premees need extra loading
I suggest that by the second week acute problems were solved mostly and enteral feeding and organ functions renal and Liver recovered
Metabolizm of the drug changed by time
Hi. Are doses all expressed as citrate or are some expressed as citrate and some as base? I think all we can derive from this data is that we must be cognizant that the pathways to metabolize caffeine mature over time hence a higher maintenance dose will be required to maintain the same drug level. Inter-individual variation in this population is is quite large so I don’t believe treating all the babies in the same manner is warranted.
Thank you for your literature review on caffeine citrate in preterm neonates. Also, important to note is that caffeine has being found to improve neurodevelopmental outcomes in this population. Its use for apnea of premature is just the initial indication.
In our level III NICUs, we use Caffeine with a loading dose of 20 mg/Kg follow by 5-6 mg/k per day. We measured levels, peak and trough, during the first year of use. We did not find toxic levels as define with level above 25 mg/L. When the number of episodes of apnea increase in an extremely premature infant and we ruled out other causes, we measure trough levels and found that in the majority of these cases, caffeine levels were sub-therapeutic (less than 12 mg/L). My opinion is that caffeine citrate at the doses mention above, don’t need routinely level checks.
thank you for sharing this real life experience
We start to use caffeine on the first day after delivery. We start 20mg/kg and continue with dose 5 mg/kg once a day. We have the ability to monitor the level of this medicine in the blood. We participated with other polish hospitals in study about early suply of caffeine. I don’t know if the results have already been publisched, but we see a lot of positive efects of this exam.