I don’t envy our nurses who care for babies withdrawing from various opiates and other substances. These assignments are definitely a challenge and require a great deal of patience and depending on the shrillness of an infant’s cry a good set of earplugs. Nonetheless we do our best with these infants to keep them calm and avoid as much stimulation as we can as we attempt to minimize the excitability of their nervous system.
Over 40 years ago the Finnegan Neonatal Abstinence scoring system was developed to assist medical teams by providing as objective a system as possible to compare one infant to another and determine when and if a patient should be treated pharmacologically. Unfortunately there is a problem inherent with this scoring system. It is the same problem that exists when you don’t have a blinded research trial. Imagine you are caring for an infant and you were given no history about drug exposure. How might you score a patient like that compared to one in which you are told has been exposed to illicit substances? Your senses are heightened and moreover if you were told this baby is “withdrawing terribly” or “is awful at night” you are biased. How are you likely to score such a patient when they are “on the edge” of being counted as a 1 or a 0 in a category? I bet in many cases, especially if you haven’t taken care of many such patients you err on the side of caution and score them on the high side. It is human nature. When the possible outcome of failing to recognize a withdrawing patient is a seizure, no one wants to be on when it happens having their scoring questioned. Have a look at the scoring tool though.
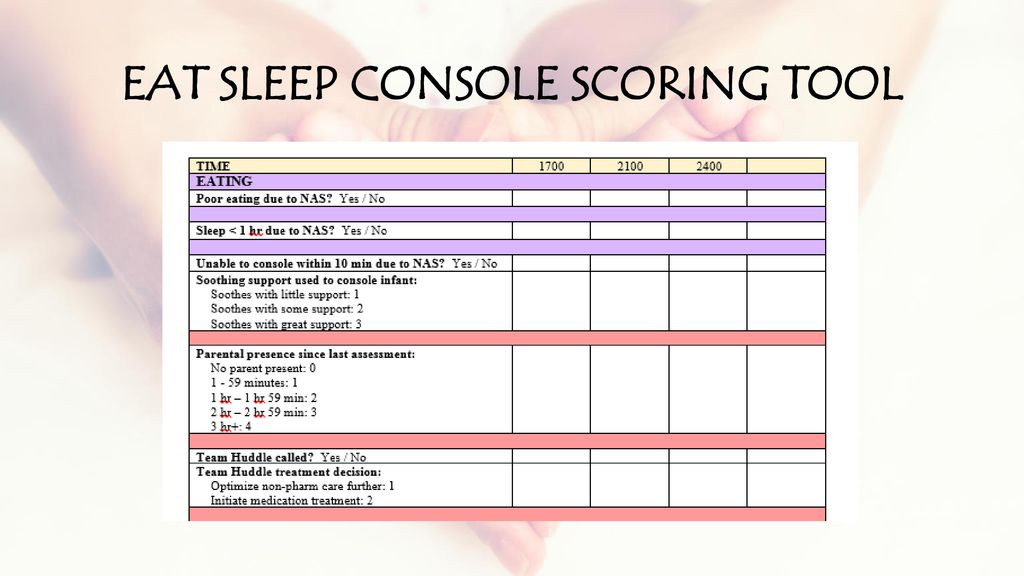
Neonatal Abstinence Syndrome – Eat Sleep Console Score Mode. EAT SLEEP CONSOLE SCORING TOOL.
There is a lot of stuff in there to check off! What if it could be simpler?
The ESC Tool
In early May, news began to break of an abstract being presented at the Pediatric Academic Society meeting. The news story from the AAP can be found here. The ESC tool is a three question tool used to assess whether an infant requires treatment for withdrawal.
E – Eat (is an infant is able to eat 1 or more ounce per feeding)
S – Sleeping (sleep for an hour or longer undisturbed)
C – Console (Be consoled in 10 minutes or less.)
If all three criteria are met, the patient does not need treatment. If one or more criteria are not met the housestaff are notified and first non-pharmacologic and then pharmacologic means are employed if necessary to control symptoms.
The authors did something quite interesting. They looked at 50 patients with 201 hospital days with prenatal exposures to opiates and applied the ESC criteria to guide treatment. Concurrently they captured the Finnegan scores but did not use them to guide treatment.
The findings I hope you will agree are quite interesting!
“FNASS scores indicated starting morphine in 30 infants (60%). Morphine was actually started on only 6 patients (12%) (p< 0.0001) based on the ESC approach. The FNASS led protocol directed initiating or increasing meds on 24.6% of days compared to 2.7% of days using the ESC approach (p< 0.0001). The FNASS approach directed that morphine was either not started or decreased on 65.8% of days compared with 94.4% of days using the ESC approach (p< 0.0001). There were no readmissions or reported adverse events.
Pretty amazing but…
The ESC approach greatly reduced the need for treatment and as the authors state there were no readmissions or reported adverse events. What we don’t know and will be needed I suspect before anyone will adopt this strategy (which I have to say again is so much simpler that current approaches) is how these children do in the long run. If the system is undertreating withdrawal, could we see downstream impacts of a “kinder and gentler” approach? One outcome that will be reported soon in the next month is length of stay. I am eagerly awaiting further results as I for one think that a simpler approach to these patients may be just what the doctor ordered. I think the nurses might thank us as well but we will see just how appropriate it is!
The Abstract reporting these findings can be found below
Novel Approach to Evaluating and Treating Infants with Neonatal Abstinence Syndrome


I think it would be a good idea to at least add muscle rigidity and tremors.
Nurses often are not taught how to use the NAS withdrawal scale and babies are already routinely under treated. If these were adults and could declare their suffering no one would begrudge them their medication. Until all staff are taught how to accurately assess a substance exposed child, it matters not which scale is used. And there is a strong concern that anything that comes dangling the ‘earlier discharge’ carrot in these days of fiscal restraint will be accepted for all the wrong reasons.
True enough Leigh. I think the big answer that is needed here though is whether less treatment leads to worse outcomes. We will need as per usual larger studies to answer this
I think that sleeping only 1hour between feeds may be fine re: intervention assessment re: the ESC, but it is an unrealistic exoectation for Nursing Staff. Feeding babies every 2 hours is a challenge with current nursing patient ratios, so 1 hour may be unrealistic. Have I missed something? Is this approach based on patients cared for by Nurses, or by rooming in parents on a Post Partum unit? I also agree with the person who commented that most NAS patients are underscored at times. I will also add that keeping these patients calm by leaving them in Mumaroos or such calming devices for untold lengths of time may result in low scores. And then they are sent home without the fancy calming devices. I like the simplicity of this new scoring approach, but maybe the ESC time between feeds should be 2 hours for a more realistic expectation of Nursing Care. Thank you.
I am interested in this new tool and I would like to do a comparative research study. I am a nursing student at Cape Breton University in Sydney, Nova Scotia, Canada. Is there any way to get in touch with somebody to discuss this further? If successful, I may obtain funding to complete more research. Please contact me at [email protected]
Looking for more information on your studies.
Regards, Deborah Peters
Deborah I just found this and am terribly sorry for missing it. The best bet would be to write the author of the quoted paper and see if they could share information with you.
Does any admin address the questions or concerns of this page? Still waiting for a reply…
Deborah I try to respond to all questions but must have missed yours. what was it?
Talk to me after more studies. Great idea if the infants are one on one….but they never are. One hour is completely insufficient, 10 minutes to console is also often unrealistic. Have these folks ever worked in a busy NICU?
I have used and taught Finnegan scoring for 30 years. I did not believe ESC could work. Now I have seen and experienced many ESC successes. HOWEVER, three principles MUST be in place. 1) The mom active and consistent in her drug rehab program, 2) the mom and her support people available to totally care and comfort the infant 24/7 and 3) the hospital team committed not only to daily rounding but also free to call stat team huddles when ESC criteria are not met. Rescue dosing of morphine has also worked. Only a few babies have needed our past practice of every three hour dosing.
Thank you for the feed back
My NICU has been using Eat, Sleep and console protocol for several months with excellent results. Decreased length of stay, increased parent and family coping skills. Family satisfaction is also very high. We screen families before initiating the protocol. Parents must provide the majority of their babies care and have a reliable family member to assist them in caring for the baby. Mothers must be on a medication assisted therapy.