by All Things Neonatal | Apr 17, 2015 | genetics, precision medicine
I know it sounds absurd that the President of the United States of America should listen to two Hollywood actors but there may be something to this title. In 1997, a movie starring the two actors named Gattaca was released. The premise of the movie was that sometime in the future we would be able to sequence the genes of all humans. Having this knowledge would allow society to direct people towards certain paths in life. Imagine you carried a genetic marker associated with above average mathematical and visual spatial skills. Your parents would be told after analyzing just one drop of blood that you would best be suited to becoming an architect or engineer; two professions where this enhanced skill set would confer an advantage. I have to admit the movie captivated me as a young medical student and I dreamed of such applications in the future as in the “real world” gene sequencing was an ever growing reality.
The human genome has been mapped. As the science of genomics moves along the identification of more and more mutations in genes that either increase the risk of one developing a condition or be born with one are increasing. As an example, a specific mutation that leads to cystic fibrosis can be identified prenatally and prophylactic treatment started soon after birth to modify the course of the condition. This is an example of a screening test and by definition the purpose of screening for conditions is that by knowing the condition exists one can do something about it. This is the justification for newborn screening programs across Canada and the US and has been successful in preventing adverse outcomes for such conditions as phenylketonuria, galactosemia, hypothyroidism and many other diseases as well. These tests are not genetic based but rather look for metabolites in the blood that are elevated due to an error in the metabolism of some enzyme, hormone or other molecule in the body. The establishment of widespread screening programs is a success in modern medicine and one to be celebrated.
What about the field of Genomics then which involves the mapping of human genomes? If using a metabolite that is elevated to identify a condition is possible why not go further and identify causative genetic mutations? The answer lies in something that has been called “Precision Medicine”. This is where President Obama comes in. While Governor of Illinois he first put his weight behind the concept by drafting a bill that was not passed but endorsed by his office nonetheless. 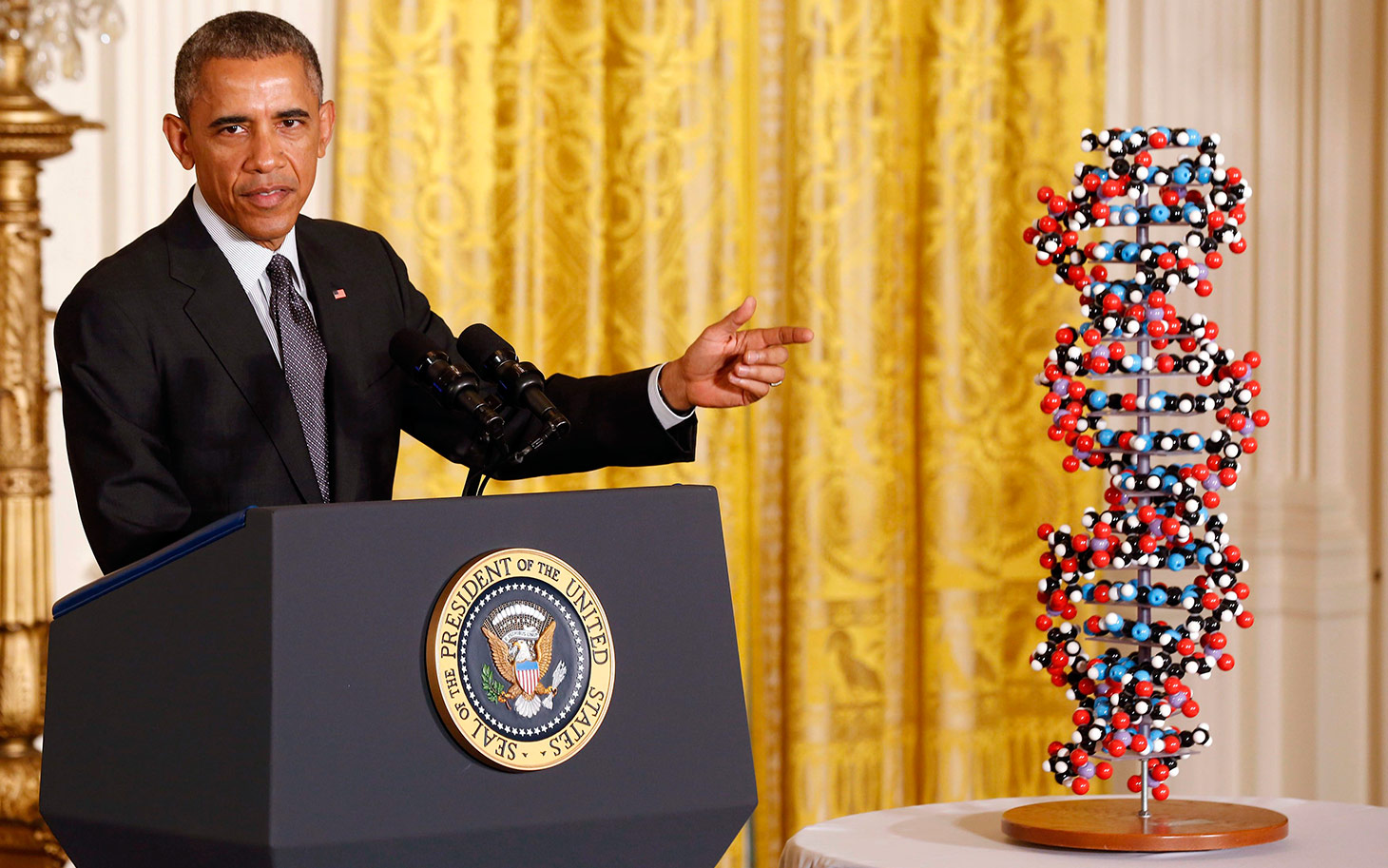 Now we come to 2015 and as President he has again raised the need for funding of such work by asking congress for $215 million dollars to fund the “Precision Medicine Project” which was announced in January 2015.
Now we come to 2015 and as President he has again raised the need for funding of such work by asking congress for $215 million dollars to fund the “Precision Medicine Project” which was announced in January 2015.
The goal of the project is to sequence the DNA of both healthy and ill individuals and identify genetic determinants of health. In fact pilot projects are already underway in some centres in the US and in this case are studying infants including 400 at the University of North Carolina Chapel Hill. Does this sound like a certain movie to you?
Before you think that I am against such advancement in medicine I am all for it but with some words of warning. We have known for some time that many types of cancer are caused by different genetic mutations that cause cells to start growing into tumours or abnormal cells in the case of leukemia. Knowing these genetic markers allows Oncologists to choose the right chemotherapy or other treatment to offer you the best chance of survival. Similarly as Angelina Jolie found, having the BRAC1 gene influenced her decision to have her ovaries removed after her double mastectomy before they could develop cancer. Having this information allows the individual to make an informed decision as to what is in the best interests for themselves and their loved ones.
Why is any of this concerning?
The issue though in all of this centres around several very concerning points. What happens to these blood spots that a nurse collects after doing the routine newborn screening in the hospital. Are they your property, the hospitals or the governments? This is the exact question that culminated in lawsuits in Minnesota and Texas recently. Unbeknownst to parents, their newborn’s blood was being sent to the US Armed Forces DNA Identification Laboratory for the creation of a forensics database. In many other states the blood was being kept for many years without parent’s knowledge. Moreover what would the government do with such data is not clear. The central question then is who has the rights to your babies DNA? For a more in-depth analysis of the history and the legal issues please read this http://www.usnews.com/opinion/articles/2014/04/28/newborn-screenings-violate-dna-privacy-rights
The second issue on the horizon has to do with the concept of a screening test. As mentioned before the purpose of screening programs are to identify treatable conditions early, such that preventative medicine to avoid complications can be started. As medicine moves along and identifies thousands upon thousands of causative genetic mutations there is a tremendous risk of straying from the intent of screening and moving towards simply identifying conditions that may not be treatable or may not affect an individual until adulthood. Take for example that a newborn screen identifies that your child is at high risk of developing early onset coronary artery disease 30 – 40 years from now. What if they are predicted to develop glaucoma in their 30s? You could go on and on with these examples but what impact could that have on their life. As a parent would you encourage them to become an elite athlete knowing they could have a myocardial infarction from coronary ischemia in their 30s? Would you support them in becoming an Ophthalmologist when you knew they were likely to develop glaucoma and visual disturbance early in their career making it difficult for them to practice? Would it have been better to not know and let them pursue their dreams even if only for a limited time? Taken to the extreme if you knew they carried a mutation leading to an untreatable condition that leads to death in their 30s ninety percent of the time what type of quality of life would they have?
The last point has to do with who owns the information. If it is indeed the government then could a world as portrayed in Gattaca not be that far off. Could parents be told soon after birth that their child will not be eligible for certain occupations or directed into specific paths? Could future employers request this information as part of a disclosure for being considered for a job? In the 90s we saw such fear become a reality when many individuals refused to have HIV testing as they were concerned the test alone would make them ineligible for life insurance.
Lastly could we see a world in which many births would never happen as prenatal testing might identify conditions that the fetus would one day develop as adults and parents decide that the child’s life was not worth living?
I don’t think Gattaca has arrived…yet. The point of all of this is that we need to tread the field of genomics very carefully. Medicine has a long history of developing technology that had the greatest promise and then once in use raised the classic question “Just because we can do this should we?” I sincerely hope that President Obama and the rest of the developed world consider these issues as we move forward which I am sure we will. We are on the cusp of a dramatic shift in the way medicine in practiced. Precision Medicine is upon and if you think that I am talking about something that is off in the distant future please look at these hospital websites where you can have your “Precision Medicine” already. I wonder what Uma Thurman and Ethan Hawke think about all of this?
http://dukepersonalizedmedicine.org/
http://mayoresearch.mayo.edu/center-for-individualized-medicine/individualized-medicine-clinic.asp
by All Things Neonatal | Apr 14, 2015 | Developmental care, kangaroo care, Neonatology
It’s the 5th International Kangaroo Care Day!
We took the challenge this year again and I am happy to announce achieved even greater success than last time around! Since the last time we have purchased special clothing to facilitate the practice and with this new initiative perhaps it helped us reach new highs! Here are the results paraphrased from one of our very own!
At St. Boniface Hospital
“663 hours and 29 minutes. This means 2 hours and 4 minutes per patient per day.
The really great part of this is the involvement we had from L&D and LDRP. Both units kept log sheets and informed patients and visitors about the importance of Skin to Skin.
L&D logged 65 hours and 27 minutes for 58 patients which equals more than an hour per patient, their patients don’t stay as long.
LDRP logged a total of 268 hours and 47 minutes for 34 patients which is more than 8 hours of skin to skin per patient and baby. LDRP had some parents who did more than 15 hours during their hospital stay, one family logged 34 hours!
At HSC
321 hours of KC in the 3 Neonatal Areas combined!
.5 hours per patient per day eligible for KC! (excludes those too sick)
How Does This Compare to Last Year (For St.B)?
Sunnybrook NICU in Toronto put out a challenge to promote Kangaroo Care for a two-week period to in the NICU. We took the challenge at St. Boniface Hospital and here are the results…
Our dates were from April 13-27.
We totaled 647 hours and 10 minutes, equals 27 days worth of skin to skin.
Total of 36 babies in the unit, another 14 infants that were held KC while in a C-section or being monitored by our Observation staff (these babies had TTN and were being transitioned KC in L&D and LDRP.
We had 9 long term micro premies that were in the unit at the time of the challenge, they averaged 33-69 hours during the two week period.
Not bad at all I say based on the number of babies we had! This represents an average of 18 hours of KC per baby over that time!
You have likely heard of Kangaroo Care and you may have even seen some children receiving it in your hospital. Why is this so important?
Kangaroo Care (KC) or Skin to Skin Care (STS) is an ideal method of involving parents in the care of their premature infant. It fosters bonding between parents and their hospitalized infant, encourages the family to be with their child and thereby exposes them to other elements of neonatal care that they can take part in. While we know that many units are practising Kangaroo Care there is a big difference between having KC in your unit and doing everything you can to maximize the opportunity that your families have to participate.
There is much more to KC than simply holding a baby against your chest. For a demonstration of KC please watch the accompanying video and show it to any one in your units that may need a visual demonstration. This excellent video is from Nationwide Children’s Hospital and walks you through all of the important steps to get it right and maximize benefit.
https://www.youtube.com/watch?v=_MateX87u9k
Before you reach the conclusion that KC only serves to enhance the parental experience it does so much more than that. The practice began in Bogota Columbia in 1979 in order to deal with a shortage of incubators and associated rampant hospital infections. The results of their intervention were dramatic and lead to the spread of this strategy worldwide. The person credited with helping to spread the word and establish KC as a standard of care in many NICUs is Nils Bergman and his story and commentary can be found here http://bit.ly/1cqIXlm
The effects of KC are dramatic and effective to reduce many important morbidities and conclusively has led to a reduction in death arguably the most important outcome. An analysis of effect has been the subject of several Cochrane Collaboration reviews with the most recent one being found here.
To summarize though, the use of KC or STS care has resulted in the following overall benefits to premature infants at discharge or 40 – 41 weeks’ postmenstrual age:
Reduction in
mortality (typical RR 0.68, 95% CI 0.48 to 0.96)
nosocomial infection/sepsis (typical RR 0.57, 95% CI 0.40 to 0.80)
hypothermia (typical RR 0.23, 95% CI 0.10 to 0.55)
Increase in
KMC was found to increase some measures of infant growth, breastfeeding, and mother-infant attachment
To put this in perspective, medicine is littered with great medications that never achieved such impact as simply putting your child against your chest. This is another shining example of doing more with less. This is not to say that modern medicine and technology does not have its place in the NICU but KC is simply too powerful a strategy not to use and promote routinely in the NICU.
Please join me in championing this wonderful technique and make a difference to all of our babies!
A sample of our parent letter to promote KC is found in the link below.
Parent letter II
by All Things Neonatal | Apr 13, 2015 | minimizing bloodwork, Neonatal, Pain in the Neonate
As those of you who have been following this blog are aware, I am always on the lookout for strategies that can help minimize blood work without sacrificing care in the NICU. At particular risk our the very premature infants in our units who for example at 1 kg have about 80-90 mL of blood. It does not take very many 0.5 – 1 mL “small” draws to create anemia. In a recent study (free article in link) of infants less than 1500g entitled A mathematical modeling approach to quantify the role of phlebotomy losses and need for transfusions in neonatal anemia, the authors studied 26 infants over a one month period. The results were staggering in that these infants experienced 138 +/- 21 blood draws with an average of nearly four transfusions per patient. While the authors do not specify what type of testing was done they did find a shocking statistic that 59% of the blood collected by weight of sample was discarded. This certainly stresses the point that we should aim to minimize the volume of sample collected in each case to that which is only necessary for the equipment to run. Furthermore, strategies to minimize sample draws should be utilized where possible and if accuracy permits point of care technology may further reduce volumes required and provide immediate results at the bedside. Lastly where possible, utilizing non-invasive technology to avoid blood draws needs to be explored when possible and was the subject of another post on Masimo non-invasive HgB measurement (http://wp.me/p5NWfD-1t).
Certainly in sick neonates whether they be term or preterm the drawing of blood gases to monitor ventilation contributes to the anemia of prematurity which often culminates in a transfusion. Sicker infants with greater lability due to respiratory compromise are deserving of optimal ventilation and this is achieved by monitoring pCO2 levels in arterial or venous samples. There have been different strategies employed to replace the sampling of CO2 by blood gas analysis which have not been very successful but there is one that I believe has promise that I will discuss at the end.
Transcutaneous pCO2 measurement was introduced in the 1980s. While this technology does allow measurement of pCO2 the variation between true arterial pCO2 and tcPCO2 can be wide making the technology difficult to implement on a consistent basis. In particular the accuracy in infants <28 weeks has been quite poor leading to increased numbers of arterial and venous samples to “check” ow closely the results correlate. As was described in 2005 by Aliwalas LL et al the technology in this group who actually have the highest number of blood draws does not meet the required standard to replace arterial pCO2 measurements (http://www.ncbi.nlm.nih.gov/pubmed/15496874)
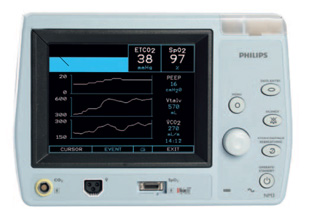
Another method is of directly sampling exhaled CO2 in ventilated patients. Traditionally such measurements were taken with proximal gas sampling and in neonates in particular the results were discouraging. Problems encountered with proximal end tidal sampling were related to the lack of cuffed endotracheal tubes in part as the measured gas would be diluted with air in the presence of any leak around the tube leading to underestimation of true CO2 levels. Furthermore, in the presence of significant pulmonary disease the clearance of CO2 may be impaired such that the arterial pCO2 – ETCO2 difference may be quite large. For a review see the free article by Malloy and Deakins Are carbon dioxide detectors useful in neonates? The agreement between arterial and proximal sampling measured in this way has been quite variable and as such the technology has not really caught on to any great degree for monitoring ventilated infants. That being said it can be quite useful at determining if the endotracheal tube is in the trachea or esophagus. The presence of the waveform even if not yielding an accurate level confirms proper placement although where the tube sits in the trachea still needs confirmation.
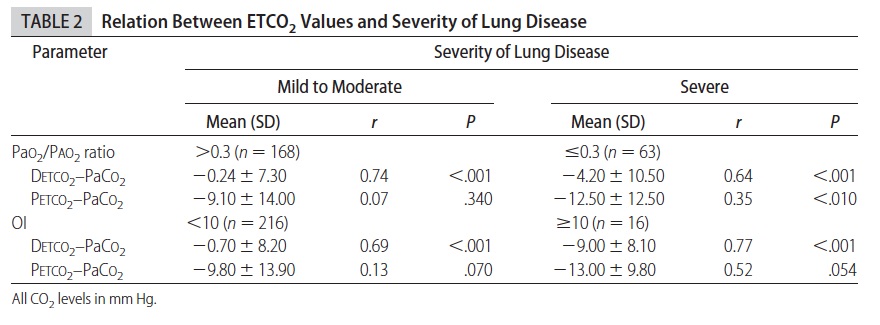
The final method for sampling CO2 is the one which I believe holds the most promise for actually reducing blood draws and by extension risk of anemia and pain in the neonate. Kugelman and colleagues in Haifa, Israel published the following paper (free article in the link) A novel method of distal end-tidal CO2 capnography in intubated infants- comparison with arterial CO2 and with proximal mainstream end-tidal CO2. This creative study utilized a double lumen endotracheal tube which had been designed for surfactant installation and distal pressure measurement to instead sample pCO2 near the carina. This strategy was postulated to eliminate the issue with dilution of gas from proximal sampling and provide a closer measurement of true pCO2 when compared to arterial CO2 and proximal sampling. They studied 27 infants with varying degrees of pulmonary condition severity although most had RDS. When comparing the three methods of pCO2 measurement the following was found.
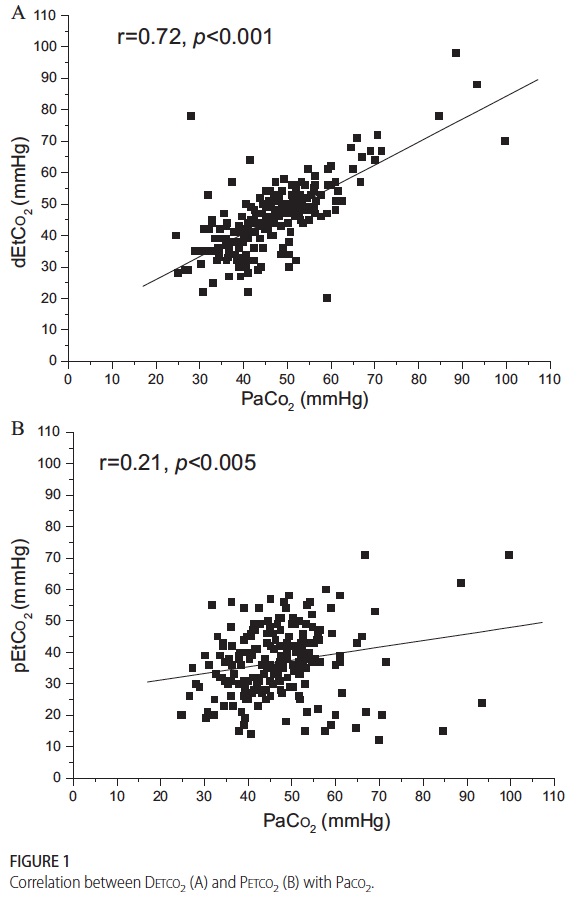 This demonstrates that while proximal measurement was quite poorly correlated with true arterial pCO2 the distal measurement was much more accurate. In fact the mean differences between arterial pCO2 and distal measurement was -1.5 mm Hg while that of proximal measurement -10.2 mm Hg albeit with wide confidence intervals. As found in other studies of proximal end tidal CO2 measurement, worse pulmonary disease correlated with worse accuracy as shown in table 2.
This demonstrates that while proximal measurement was quite poorly correlated with true arterial pCO2 the distal measurement was much more accurate. In fact the mean differences between arterial pCO2 and distal measurement was -1.5 mm Hg while that of proximal measurement -10.2 mm Hg albeit with wide confidence intervals. As found in other studies of proximal end tidal CO2 measurement, worse pulmonary disease correlated with worse accuracy as shown in table 2.
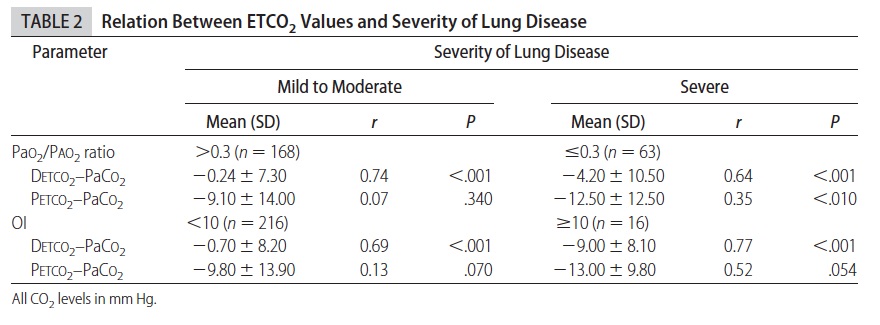
As the pCO2 rises above 60 the accuracy is less but remains much better than proximal measurements. Interestingly the same group has published an additional trial using high frequency ventilation and confirmed the measurements remain accurate. (http://www.ncbi.nlm.nih.gov/pubmed/22328495)
So what does the future hold? in VLBW infants one concern may be the internal diameter of the smallest double lumen tubes and the effect of upsizing to a larger tube and risk of subglottic stenosis. After a personal communication with Dr. Kugelman I understand that this has not been an issue in their unit as they tend to use these double lumen tubes in most if not all of the their infants. The accuracy is sufficient enough from my point of view that units should be able to implement this strategy at least in larger infants at first (those who would need a 3.0 ETT and larger) to see the effect on blood sampling. I suspect that one blood gas a day to determine accuracy in a given patient would be sufficient most of the time if the numbers were found to correlate well.
I would welcome feedback from people who work in units where this strategy has been utilized. How effective is it? Did it reduce your blood gas draws or increase them due to unreliability? Have you seen a rise in subglottic stenosis? Please send your feedback to either this site or at my Facebook page at www.facebook.com/AllThingsNeonatal.

by All Things Neonatal | Apr 5, 2015 | LGBT
I know, this sounds like a ridiculous title to a post but it actually happened in Detroit recently. Krista and Jamie Contreras loving parents of 6 day old Bay were denied care by a Pediatrician solely due to the parents being Lesbians. Please watch this short video before reading on.
http://www.cnn.com/videos/us/2015/04/04/bts-smerconish-gay-couple-says-doctor-refused-to-treat-baby.cnn
I can’t help but think that the recent laws that have been passed in Indiana and Arkansas open the door for similar situations in those states. Moreover, imagine the impact if the laws spread to other conservative states in the US. If you look at some history though, the Religious Freedom Restoration Act (RFRA) was first passed in 1993. The act was brought into being after an American Indian man was fired from his job for failing a company drug test. The drug in this case was peyote which culturally was acceptable for him to use but not in keeping with company policy. The law that was brought into existence was therefore designed to protect people from the Government and industry interfering with religious practices which in this case they were as peyote was used as part of his religious practice.
That sounds like a very positive step in the right direction so why have Indiana and Arkansas come under so much heat over this current legislation? The reason is that the law makes it possible for not only the individual but a company or business to sidestep the law if their religious beliefs are found to be in conflict with a person or request. Don’t believe this could happen? It already did. The US Supreme Court recently ruled that the Hobby Lobby company could refuse to provide birth control to employees as a health benefit. Using birth control violates the company’s Christian religious beliefs.
The physician in this case lacked a solid RFRA in Michigan so she could do nothing more than apologize for her stance. What concerns me greatly though is the hypothetical situation in which a member of the Lesbian Gay Bisexual Transgender (LGBT) community decides to have a child with a member of the same sex in a state with an RFRA. What if for instance Michigan had such a law? Would this Pediatrician have apologized or simply stood behind the government? I am not sure what would have happened and in a state like Michigan which in my view is a little more progressive than some of the states in the “Bible Belt” I suspect this family would have found another Pediatrician to take care of them. If this story had taken place in Arkansas, how difficult would it have been to find another Pediatrician on short notice while the infant was still hospitalized? Might be a little harder.
On the first day of Medical School all students are asked to take the Hippocratic Oath. The Oath is not the same as was first spoken by Hippocrates but rather in one form or another is based on the version that came from the Declaration of Geneva and reads as follows:
At the time of being admitted as a member of the medical profession:
- I solemnly pledge to consecrate my life to the service of humanity;
- I will give to my teachers the respect and gratitude that is their due;
- I will practice my profession with conscience and dignity;
- The health of my patient will be my first consideration;
- I will respect the secrets that are confided in me, even after the patient has died;
- I will maintain by all the means in my power, the honour and the noble traditions of the medical profession;
- My colleagues will be my sisters and brothers;
- I will not permit considerations of age, disease or disability, creed, ethnic origin, gender, nationality, political affiliation, race, sexual orientation, social standing or any other factor to intervene between my duty and my patient;
- I will maintain the utmost respect for human life;
- I will not use my medical knowledge to violate human rights and civil liberties, even under threat;
- I make these promises solemnly, freely and upon my honour.
Point number 4 states “The health of my patient will be my first consideration”. Furthermore point #8 specifically spells out that sexual orientation should not matter.
In essence the newborn baby is in need of treatment and you are obligated to provide such treatment without consideration of whether the parents are members of the LGBT community.
Quite frankly I am embarrassed for this physician. Do not misunderstand my intention here though. Whether I support the LGBT community or not is irrelevant to this discussion. What is relevant is that a member of the medical community who swore an oath to put the patient first has violated that oath. It is my hope that these words will reach the eyes or ears of physicians who may have had similar thoughts and remind them of the oath that they once swore to uphold. The United States is at a tipping point (quoting Malcolm Gladwell again) where physicians or medical corporations may opt to refuse treatment for infants who happen to be born to LGBT parents. The infant was born into this world and needs someone to care for them from a medical standpoint. Whether their parents choose to be intimate with members of the same sex should never enter the equation and I hope that this is the last report I hear of this behaviour by a member of the medical community. Sadly as I often say hope is not a good plan and I fear that this indeed will not be the last instance we hear of.
The President of the United States no doubt wishes to leave a legacy as he prepares to leave office. Obamacare, a nuclear deal with Iran and a two state solution for Israel and the Palestinians will be great accomplishments if they last. Sadly if he doesn’t weigh in and do something soon the ability of companies, organizations and governments to discriminate against member of the LGBT community will leave a black mark on the Presidency that will be remembered long after the Republicans undo much of what he feels will be his “accomplishments”.
Please Mr. President. Do something.

by All Things Neonatal | Apr 4, 2015 | Uncategorized
The following video is seemingly out of a science fiction story but it is reality and has made a world of difference for a mother and her newborn!
http://www.cnn.com/videos/us/2015/01/23/dnt-legallly-blind-mom-sees-newborn.cbc/video/playlists/oh-baby/
The story is the same. You and your partner find out that you will be expecting a newborn in the near future. You dream of what they might look like and dream about meeting them for the first time. In the case of the mother in this video that was not the case as she suffers from Macular Degeneration. A disease that typically affects people beyond the childbearing years but in her case afflicted her at an age way too soon.
Medical breakthroughs happen frequently and are wonderful to behold but this story caught my eye due to the impact of being able to restore something that we as parents hold so dear to us. To be able to view our beautiful baby with our own eyes. Thanks to an Ottawa company featured in the video this is now a reality for this mother.
As I sit and write this post with my beautiful children close by I can’t help but think how grateful I am to be able to take in their beauty. This is something I never questioned I would be able to do but for some no doubt this was a dream. The difference is that thanks to http://www.esighteyewear.com/ a Canadian company this is now a reality.
I am not an Ophthalmologist but I have no doubt that such eyewear will transform the quality of life beyond this case as Macular Degeneration is something that many unfortunately live with. If you know someone with MD you may wish to pass this along to them as it may change their life.
 Now we come to 2015 and as President he has again raised the need for funding of such work by asking congress for $215 million dollars to fund the “Precision Medicine Project” which was announced in January 2015.
Now we come to 2015 and as President he has again raised the need for funding of such work by asking congress for $215 million dollars to fund the “Precision Medicine Project” which was announced in January 2015.
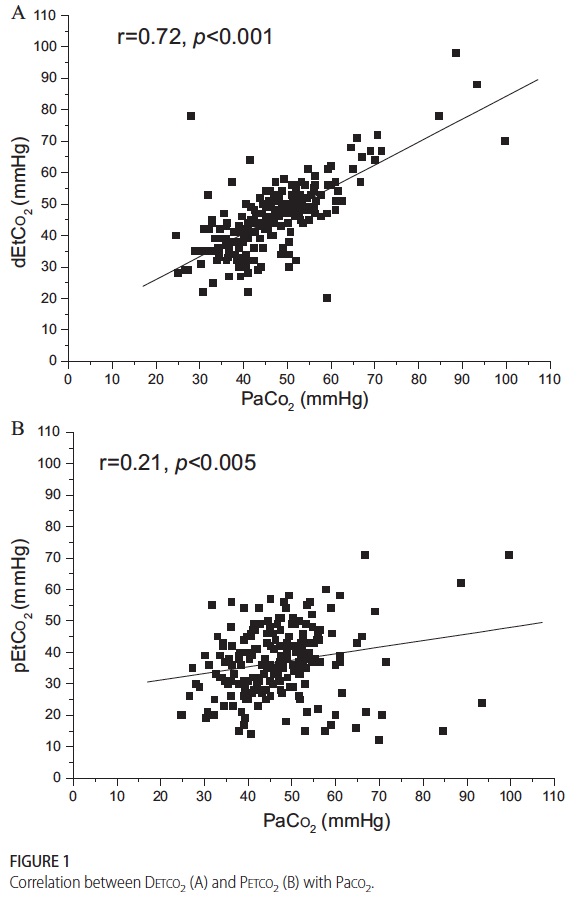 This demonstrates that while proximal measurement was quite poorly correlated with true arterial pCO2 the distal measurement was much more accurate. In fact the mean differences between arterial pCO2 and distal measurement was -1.5 mm Hg while that of proximal measurement -10.2 mm Hg albeit with wide confidence intervals. As found in other studies of proximal end tidal CO2 measurement, worse pulmonary disease correlated with worse accuracy as shown in table 2.
This demonstrates that while proximal measurement was quite poorly correlated with true arterial pCO2 the distal measurement was much more accurate. In fact the mean differences between arterial pCO2 and distal measurement was -1.5 mm Hg while that of proximal measurement -10.2 mm Hg albeit with wide confidence intervals. As found in other studies of proximal end tidal CO2 measurement, worse pulmonary disease correlated with worse accuracy as shown in table 2.