by All Things Neonatal | Mar 14, 2015 | caffeine
If that is not a title designed purely to gather attention I don’t know what is. I can’t take credit for the title thought as I borrowed it from the following video and article link. . In late 2014 and January of 2015 the subject of using these two medications to improve survival without chronic lung disease-CLD (for a review see here) started making the rounds of many websites and news agencies.
Caffeine is given to premature infants to stimulate breathing via blockade of adenosine receptors in the brainstem. As adenosine inhibits breathing in this part of the brain it is an effective treatment to address apnea in the newborn. In 2006 Schmidt B et al published the Caffeine For Apnea of Prematurity (CAP) Trial (Full Article) and demonstrated that infants 500 – 1250g who received caffeine versus those who did not, spent less time on a ventilator and furthermore had less chronic lung disease in the long run. A win on both fronts and in essence established early caffeine use as a standard therapy in NICUs. Further research has demonstrated that early use of caffeine has other benefits when given shortly after delivery such as fewer intubations, greater success supporting infants using CPAP alone rather than invasive ventilation. Although many mother’s around the world avoid caffeine during pregnancy it has become one of the most common drugs used in the premature newborn and to allay any anxiety about outcome, a follow-up study from the CAP study above has shown no harm in long-term neurodevelopment from the exposure to caffeine.
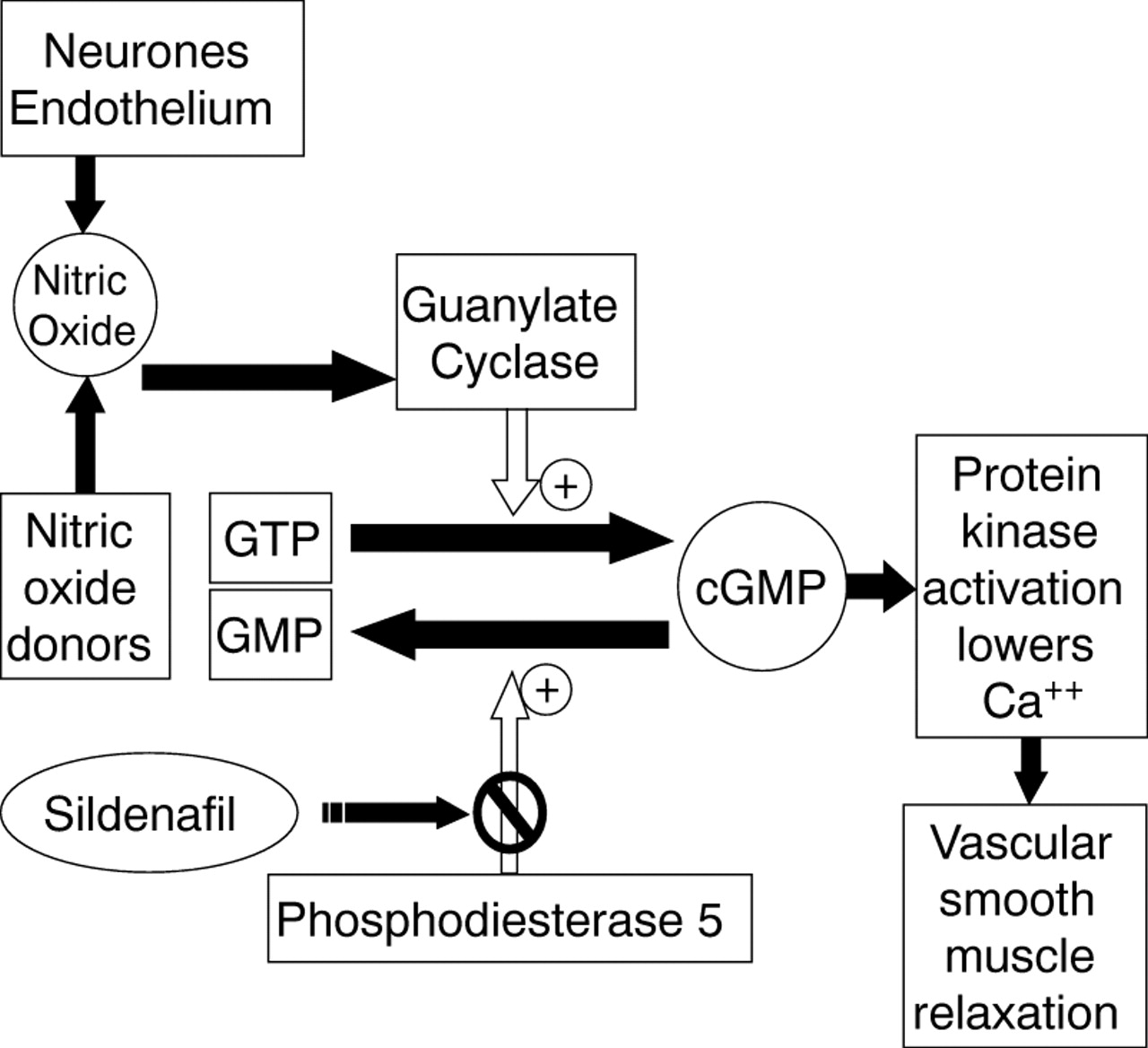
What then about Sildenafil otherwise known by it’s trade name Viagra? Sildenafil is a phosphodiesterase V inhibitor which works by increasing levels of cGMP which in turn cause the smooth muscle in arterial vessels to relax.
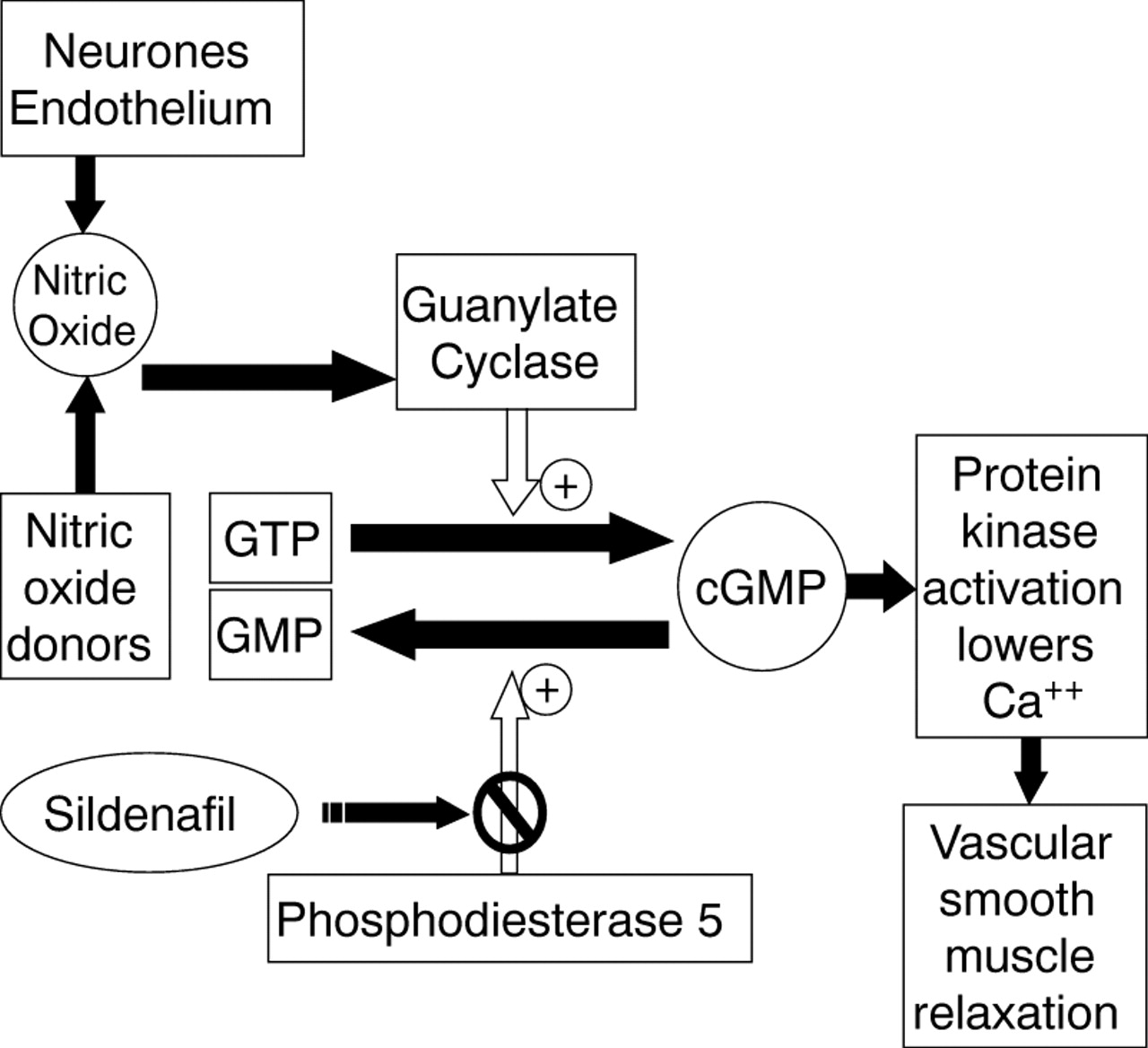
It may surprise some of you to learn that Sildenafil was originally designed to treat high blood pressure in the lungs or pulmonary hypertension. It was a well-known side effect that took it’s marketing in a completely different direction. Previous research however, studying the impact on patients with pulmonary hypertension in the newborn demonstrated that sildenafil alone or in combination with inhaled nitric oxide could reduce pulmonary vasoconstriction. Approximately 10-25% of premature infants with CLD have accompanying pulmonary hypertension depending on how one defines it’s presence. Sildenafil then could arguably be used to treat patients who have established CLD or perhaps even evolving CLD to prevent the oxygenation problem from pulmonary hypertension that accompanies CLD.
“Save your preemie with Caffeine and Viagra!” seems to indicate that the evidence is out there and that it is VERY positive but sadly it just isn’t. The evidence for use of sildenafil in established CLD is weak and limited to small observational or retrospective studies in which patients were put on long-term sildenafil and over time improved. The challenge with these types of studies is that it is difficult to say with any certainty that the patient wouldn’t have improved over many months anyway. Certainly, in those reports where the medication was stopped and ultrasound evidence of pulmonary hypertension returned, it is suggestive but these one-off cases are not enough to convince me that it should be considered as a standard of care.
Rat models of evolving CLD have demonstrated improved angiogenesis and alveolar growth with additional findings in the heart of less right ventricular enlargement and pulmonary hypertension. If confirmed in humans this would certainly be a wonderful treatment to prevent CLD from developing, as these findings are largely what contribute to this diagnosis. So what is the evidence for a preventative effect of sildenafil?
One Tiny RCT
In this study of 20 patients, half were randomized to sildenafil 3 mg/kg/d and half to placebo for a 4 week course starting at day 7 of age in patients who were still ventilated. In the end only 7 patients in the sildenafil arm finished the study. No differences in any outcomes were found so no benefit could be demonstrated. The study was underpowered to find a difference and aside from that the dose chosen was low compared to other studies using as much as 8 mg/kg/d. Could a larger dose shown a difference in outcome? Maybe but again a larger sample size would have helped and I suspect will come with time. The bottom line is that it was a small study that does not add anything to the pool of evidence suggesting a benefit of sildenafil in either treatment of patients with CLD or to prevent it.
This is the danger of course in the lay press hearing about information like this. It is sensational and will attract a lot of readers but in the end should parents be asking their health care providers in NICU to use sildenafil as a standard treatment for CLD or to prevent it? For the time being I would say not but with the provision that I actually believe there may be a role but for the right patient.
In our unit we have an Integrated Targeted Neonatal Echocardiography program that allows us to take measurements of pulmonary vascular resistance that are quite different from traditional measures reported using a standard echocardiogram. Using this technique, patients with pulmonary hypertension can be identified and treated whether it be with inhaled nitric oxide or sildenafil or both. It is also tempting to speculate that there may be early predictors of patients who may develop CLD with pulmonary hypertension and it is those premature infants that would like be the best to target such therapies in. By selecting out those patients only who would develop this condition a therapy to prevent it would be better studied in a pure sample. Treating the 75-90% of patients who will not develop this condition with a drug will dilute out your results for sure compared to studying only those patients with a high likelihood of disease. I will have to dream of this type of study for the time being though as I am unaware of such work being done at the moment.
Finally I think it is worth mentioning that Sildenafil should not be used without some caution. In 2012 the US FDA issued a warning (read warning here) on the use of high doses of Sildenafil for the treatment of pulmonary hypertension due to a higher mortality rate in a Pediatric clinical trial (Free article here) involving children at least a year of age. The high dose group received a dose from roughly 3-6 mg/kg/day which is in keeping with the dosing used in the trials in infants. Since that time the FDA has softened it’s stance (clarification) but it need to be acknowledged that the use of Sildenafil under a year of age is considered off label and with the aforementioned concerns it would seem prudent if using the medication to use a lower dose.
Taking all of this information in I would suggest it seems wise to continue giving our premature infants a morning cup of coffee each day but for the time being I would leave more frequent use of Viagra to the adults.
by All Things Neonatal | Mar 12, 2015 | General Comments

I would like to thank each and every one of you for your words of encouragement over the last three weeks since the inception of this blog. Today marked a significant event by surpassing 100 followers who receive an email with each blog post. As of tonight, there have also been almost 2000 viewings of these posts from at least 20 countries worldwide. I find these metrics informative as I really have no idea how many views happen on Facebook or Twitter but with the blog data I get a sense of how many of you are out there!
I have thoroughly enjoyed writing these pieces and really appreciate the feedback on each topic. The last few weeks have included correspondence with someone from another country who was unaware that Propranolol could be used for hemangiomas and a practical suggestion for starting children on propranolol in a day clinic type of environment. I look forward to the opening of such a clinic in our hospital in the next year or so. There is no doubt that the topic that garnered the most attention was the use of breast milk by body builders. Although this was a more playful topic it did raise awareness of the use of donor breast milk and who knows whether or not a unit somewhere may look into this through the communication that the post generated. The Sympathetic Note to the Anti-Vaxxers caused an explosion on Twitter that left me exhausted after 3 days of exchanges with people opposed to vaccination. I have to say that although it was tiring, the amount of websites, articles and information from that side of the argument that I was provided is worthy of a post in and of itself! I learned a lot from individuals on the other side of the promoting health coin and I feel as if I am a better doctor for it as I now have better insight into the basis for many of their arguments.
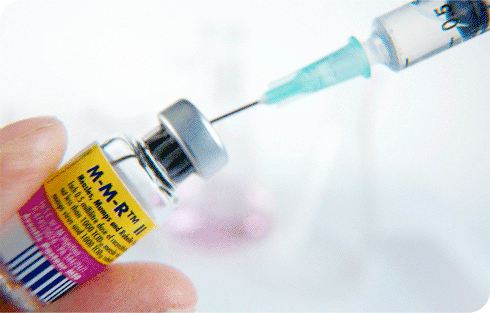
I have to say the pinnacle of this experience however was an exchange with someone who attributed their child’s autism to the MMR vaccine. After a bit of a lengthy exchange I was sent a picture of her beautiful daughter with a thank you for having given them some relief after reading the post on MMR. Their daughter was lovely as was the knowledge that I had helped someone who I would have otherwise never met if it weren’t for this medium.
Your support has kept my enthusiasm for writing up and on a local front I also want to thank the doctors, nurses, dieticians, RRTs and others who have encouraged this medium for education. I have really enjoyed being stopped in the NICU, IMCN or hallways to chat further about this post or that. It means a lot!
Moving forward I look forward to many more opportunities to share with you. I would like to add that I have created a twitter feed at @NICU_musings to talk about these and other topics not on the blog for those of you who are more bent on Twitter. There is also now a Facebook page at https://www.facebook.com/allthingsneonatal where discussion can also take place if you are more of a Facebook fan.
I will leave you with this news story I read tonight which reminded me of the power of community generosity that many of you know we have been blessed with here. Charitable giving is a very special and important thing and this story seemed right to finish off on a high note.
http://www.yourerie.com/news/news-article/d/story/pay-it-forward-check-helps-neonatal-intensive-care/16215/VCOYMz8je0631nC0dShYQQ
by All Things Neonatal | Mar 10, 2015 | Uncategorized

Leonard Nimoy passed away February 27th and shortly afterwards a paper was published that his character Spock would have been proud of. For those of you who know me you will surely appreciate that I try to minimize blood work as much as possible in our infants. That is not to say that other colleagues don’t but in my case it may border on an obsession. I am always on the lookout for technology which helps to achieve this goal that is both accurate and safe to use in our population of neonates.
We are all familiar with Masimo as the providers of the Radical-7 Co-Oximetermonitors that we use in our units. They are highly accurate and provide our histogram analysis which we employ to minimize oxygen use in the units. Some time ago an additional capability was developed which allows the non invasive continuous measurement of hemoglobin (SpHb), along with carboxyhemoglobin and methemoglobin.http://www.masimo.com/hemoglobin/ This technology had been validated in adults and infants > 3000g limiting its widespread applicability in many Neonatal Units. In adults however it had been shown to reduce likelihood of transfusion as a significant benefit.
The publication referred to above is entitled Validation of noninvasive hemoglobin measurement by pulse co-oximeter in newborn infants by Nicholas et al. J of Perinatology; March 5, 2015:1-4. (http://1.usa.gov/18zmEqV) What drew me to this observational study comparing continuous measurement of HgB to serum HgB samples was that the population studied were infants all less than 3000g. Sixty one patients were enrolled and at three different time points between 2-10 days, serum HgB was compared to SpHb. The patients had a birth weight mean of 1177 +/- 610g with 48% of the subjects having a weight < 1000g.
The results were quite interesting to me. The mean difference between HgB and SpHb was -0.9 +/- 16.7 g/L for the whole group and for infants < 32 weeks -2.3 +/- 16 g/L. The correlation coefficient for the whole sample was 0.66 and for the <32 week group 0.69. What does this mean? The correlation coefficients suggest that the relationship between the two variables is not quite linear, as a true linear relationship exists as you get closer to a correlation coefficient of 1. The standard deviations are quite large for these samples so for example a patient with a true serum HgB of 100 could have a measured HgB of either 67 or 137 at the extremes but on average would have a SpHb of 97. This may not seem to be that great a correlation but it may be the trend that is more important than the actual number. This is similar to the concept of using trends in transcutaneous or end tidal CO2 sampling in ventilated patients. What will likely need to be teased out in a larger cohort though is how much agreement there is in an individual patient over time. If a patient is reading 10 g/L below on the first serum HgB measurement what will it read later in the patient’s course as HgB levels change. Also as the authors state it is unclear what effect polycythemia and anemia or low perfusion state might have on accuracy since these infants were studied only over a maximum 8 day period.
So where does this leave us? The technology has now been studied in a population of infants that comprises the largest cohort of infants that have HgB monitored frequently. If the technology is capable of trending HgB for us then I think there may be some use. Would we need to draw a CBC every two weeks as an example if the SpHb was reading > 100 and a first and second CBC showed that for that patient the result was within 10 or 15 g/L of the true value? Could we use such a continuous reading to warn us of a severe IVH or pulmonary hemorrhage as it is happening? Certainly such information if accurate would be useful. A trial of this technology may be warranted!
While this post has focused on one advancement, the fictional Tricorder is not far off from reality but it is currently separated into many different devices. We now have contact lenses and subcutaneous devices that can measure glucose continually (http://bit.ly/1awuqQI), endotracheal tubes that can provide continuous pCO2 measurement and the ability to measure bilirubin non-invasively just to name a few. As the technology becomes more sophisticated with time I have no doubt that we will see a drop worldwide in the number of skin breaks we see in our patients and that for me is a step in the right direction.

by All Things Neonatal | Mar 9, 2015 | Dermatology
The story is typical. A family notices a small red spot in the weeks following delivery which enlarges over the next month. They present to their family doctor or Pediatrician who identifies the most common skin lesion in childhood; a hemangioma affecting about 3-10% of all children depending on the population observed. As a resident I was given the following advice regarding hemangiomas; “As long as the hemangioma is not of cosmetic concern, sight threatening, multiple in number or causing anemia or thrombocytopenia watchful waiting is recommended.” Furthermore I recall the following general advice that while they tend to enlarge over the first year of life, 40% are gone by 4 years, 60% by 6 years and 90% by 9 years. After my training I started a practice passing along the same advice to the infants I now cared for.
Then something happened similar to the serendipitous discovery of penicillin. In 2008, Leaute-Labreze et al published a case report in which they described a child being treated for a facial hemangioma with corticosteroids. Unfortunately the hemangioma did not respond to treatment but rather led to a cardiomyopathy requiring treatment with propranolol. Curiously the hemangioma demonstrated significant regression on propranolol. The results of this case report prompted further treatments with propranolol in an unblinded fashion. Since this time propranolol and more recently topical Timolol (sample size 41) have been studied both in observational and small randomized controlled trials. Propranolol while effective has potential side effects such as hypotension, bradycardia and bronchospasm which has limited it’s widespread application except for those patients with either large, sight threatening or multiple hemangiomas. Topical timolol in the RCT above was demonstrated to be safe and when given locally, free of such side effects making it a seemingly ideal treatment for smaller hemangiomas that may have some cosmetic concerns later in life as they regress. That being said, the time of onset for regression was noted to be after 12-16 weeks of therapy and the target they aimed for was a reduction of >5% which is certainly modest. While only a small improvement it was seen 60% of the time in the treatment group and 11% in the placebo arm. From personal experience I have used topical Timolol with patients in the NICU with varying success but in some cases the results were quite impressive. Looking at the RCT by Chan, timolol was only applied to those hemangiomas that were small and deemed unsuitable for treatment with propranolol.
This leaves us with the question; what does one use if anything for larger hemangiomas which traditionally don’t fit into the category of needing treatment vs patient observation. Secondly, is it wise to systematically treat all larger hemangiomas with propranolol as outpatients, given the potential severity of the side effects, some of which may be life threatening.
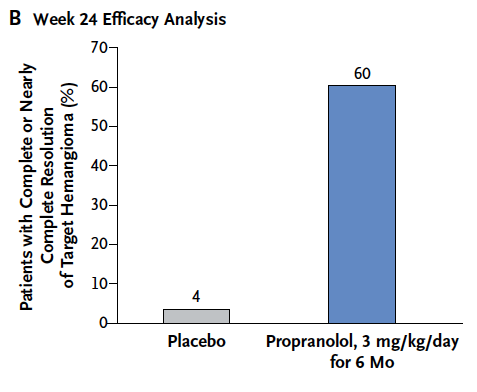
This past week in the New England Journal of Medicine we have come full circle as Leaute-Labreze et all have published a large prospective RCT http://bit.ly/1ACqn2C to determine the optimal dose and duration of propranolol for treatment of hemangiomas requiring systemic treatment. The number of patients enrolled in this study was 456 which makes it the largest study to date in this field. This study sought to determine whether 1 mg/kg/day vs 3 mg/kg/day divided twice a day for 3 or 6 months would provide the best resolution without unacceptable side effects. Eligible patients were between 1-5 months of age with a proliferating hemangioma and were treated for either 3 or 6 months depending on which arm of the study they were on. The results of this trial were striking and found that the best balance of benefit and risk was with 3 mg/kg/day for 6 months and is shown below graphically compared to placebo.
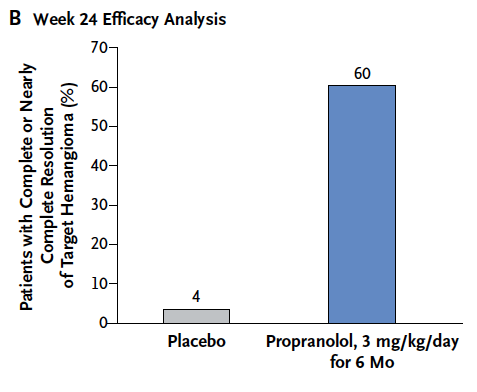
This difference translates into a number need to treat to cause regression = 1.7 or rounded up 2. For every two patients that you treat with propranolol you will cause one hemangioma to regress. Try finding a therapeutic benefit like that in another trial!
But what about safety? Side effects were rare compared to placebo but not negligible. The most common side effect was diarrhea and with respect to life threatening adverse effects the only one really noted was bradycardia but in a patient with enterocolitis. My take on this treatment is that it appears to have great impact with little downside!
How do we apply these results though to “real life” situations. We now have as I see it a “one-two punch”. Hemangiomas that are deemed to require no systemic treatment can be treated with a safe topical drop that has been used for years for glaucoma patients. Patients with larger more significant hemangiomas may be treated with a highly efficacious treatment that may have very few side effects.
The downside of systemic therapy at least in Winnipeg is that treatment with propranolol generally requires a hospital admission at the start of treatment to monitor for side effects that would be considered life threatening. With an incidence of 5% of children it would be impractical to admit 600 children a year for such treatment based on an estimated 12000 births in the region a year.
I do believe the time is upon us for change though. As I see it, gone are the days where we tell parents that we will see what develops when their child has a small hemangioma. If you have a willing parent who is concerned about the hemangioma and it is < 1.5 cm in size I believe topical Timolol should be offered to the family for a period of 6 months treatment. Anything larger than that would merit treatment with propranolol. Nine years is potentially a very long time to wait for a lesion to regress and potentially leave a scar or telangiectasia behind. If we can do something about it now with such a high rate of success and minimal risk to the patient, why wait?
My advice to you if you either have a child with a hemangioma or know someone else with one is to have them ask their doctor whether Timolol or Propranolol would be right for them. Given these findings I know my practice will change.
by All Things Neonatal | Mar 5, 2015 | Vaccination
I have two healthy children who make friends easily and excel at most tasks put before them. Children with autism may be healthy but life may be anything but easy. WIth the receipt of any bad news comes different phases of emotion but one common reaction is search for answers. Today I experienced an exchange of comments on Twitter from someone who disagreed with some comments I made with respect to giving the MMR vaccine. The gist of it was that they had been the responsible parent, listened to the doctors of the world and given the MMR vaccine only to find out some time later that their child was diagnosed with autism. I feel for this person and every other parent touched by this diagnosis. It is devastating and life changing although with time and a lot of work such children can make great strides but sadly not all.
I understand then the fear of receiving such a diagnosis is a compelling reason to avoid getting vaccinated if there is even a chance that your child could develop autism. You are wanting to protect your child and I commend you for that. Unfortunately while trying to protect them you are in fact leaving them unprotected and for that matter the rest of the children in your community. The aruguments against vaccinating with MMR centre around three major arguments. The first is that parents often recall receiving the vaccine shortly before the diagnosis of autism was given, the second that the literature supports that autism is caused by vaccines and the last that when the MMR vaccine was brought into existence autism rates started to rise. Below I will address each point with factual information that I hope in some way will make an impact on those who hold onto the beliefs which is all they are that their child developed autism due to the vaccine.
Timing of the vaccine
Definition of autism (from Wikipedia):Autism is a neurodevelopmental disorder characterized by impaired social interaction, verbal and non-verbal communication, and restricted and repetitive behavior. Parents usually notice signs in the first two years of their child’s life.[2] The signs typically develop gradually, but some children with autism will reach their developmental milestones at a normal pace and then regress.
Under a year of age language is fairly limited. Social interaction, language and repetitive behaviours are typically noted after the first year of life. Given the timing of the diagnosis and the provision of MMR at a year of age it is no wonder that parents will attribute the vaccine to the diagnosis. Let’s think about this though for a minute. What is happening here is confirmation bias. As a parent you have heard that MMR can cause autism although thankfully it is quite rare but when you get the diagnosis you immediately jump to the conclusion that this is the true cause. What you have is an association and nothing more but your mind has convinced you otherwise. It equally could have been the new cookie you gave your child that month, the fumes from the car in a traffic jam or any other possible influence or it could be that it was always going to happen but as humans we need to make sense of things. Its in our genes but it causes us to make a dangerous link that to be frank just doesn’t exist.
Autism is caused by the MMR vaccine
This argument centres around a extremely well cited paper that has been refuted. Andrew Wakefield published a link between autism and the MMR vaccine that set the world on fire. The paper though was shown to be fraudulent and has been the subject of many publications since. retraction: http://bit.ly/1wb3Xjn
Let’s think about this for a second. What if this paper had never been published in the first place? A link between vaccines and autism would not have been put in the minds of people such as Jenny McCarthy and other people outspoken against vaccines (she has since softened her stance). In fact most people would not have even thought of such a link. In essence the argument would not have even been present in pop culture and the wave of anti-vax literature would not exist. Those young people who weren’t alive in the 1970s which is the time of our last point would not even be aware of the argument. So the question is, if the lie had never been told would we even need to write pieces like this today? Hard to believe people stand on an argument that was never meant to be in the first place. To put it another way, if I published a paper that I confirmed a sample from the moon contained cheese and it spread throughout the media outlets of the world, if it was refuted would anyone actually cite it? The fact is these people who are either scared of vaccines or have a child with autism need something to hang onto and this is it.
Autism rates increased after MMR came along
Again this is an association that people have attributed to be causative. For a wonderful explanation of this phenomenon in the 1970s please read the article at this link: http://1.usa.gov/1MajxDf
Autism diagnoses did in fact rise but that had more to do with a change in the way doctors classified autism than any external factor.
What all three points have in common is that we as parents need to find order where there is disorder. We also have the same drive as physicians to do no harm. It is compelling and strong in all of us. Each and every person who writes anti-vax literature I believe is not out to harm us but they truly believe that the reading they have done or the simple beliefs they have are the right ones.
What I ask is that people read a blog such as this and open themselves up to a paradigm shift. If you can read what I have written and convert your thinking to one where you realize that all you have believed was based on poor information and switch to one in which your drive is protect your child by immunizing them your children and our children will all be better for it.