by All Things Neonatal | Feb 28, 2015 | Breastmilk
I wrote this post almost a year ago and could not believe such practice was going on. Here we are this week and the following was published in Men’s Health magazine indicating breast milk consumption by body builders has not gone away quietly.
For my own thought on this including updates to the original post please read below.
It may seem like I am making a joke but sadly it is the real deal as you can see from the USA Today video released in the past couple weeks. The benefits of drinking breast milk to add muscle mass has spread quickly among that community. That is not to say that the majority are using it but there definitely is a following. Taking a look at the website “Only The Breast“ reveals the sad truth. There are currently 6368 classifieds for women selling breast milk with 804 of these women specifically targeting men who wish to buy (Update: As of February 23, 2016 the number of offerings has risen to 10135 with 1294 offering to men so the problem is getting worse not better!). Contrast this with only 113 women willing to donate their milk. This is only one site as women are also resorting to Craigslist and Kijiji to just name a couple of alternatives. There is money in selling breast milk and sadly those who most need it may not be getting it.
The amount of evidence supporting the benefits of an exclusive breast milk diet for preterm infants in particular has exploded in the past few years. There is no question in my mind that breast milk should be distributed to babies whose mothers are unable to provide enough milk for them while in the hospital. The proven reductions In necrotizing enterocolitis; a major cause of morbidity and death in the NICU are reason enough to exclude formula from a low birth weight preterm infant. See Formula versus donor breast milk for feeding preterm or low birth weight infants.
If each case of necrotizing enterocolitis costs the US Health care system approximately $150000 imagine how much money could be saved when estimates from other studies such as the one by Sullivan et al target the reduction in NEC at about 70%. In our own centre with approximately seven cases per year we would expect to see 5 less babies affected by this per year.
Aside from the above concerns about using breast milk in a population that has no likely benefit there is substantial risk to purchasing milk online. As mentioned in the USA today video the FDA has spoken out against such practice due to high likelihood of contamination by bacteria secondary to non standardized methods of storage. The article cited in the video can be found here.
Where is the harm?
The rate of contamination at 74% is frightening and in turn puzzling that people so focused on treating their bodies like a temple would consider ingesting it. A search on Pubmed using a combination of different search criteria combined with a broader search using google failed to come up with one article showing any evidence supporting the consumption of breast milk by those wishing to build muscle mass. Given the lack of evidence and the potential for harm this is a practice that needs to be eliminated as soon as possible. The selling of excess supply from mothers to males who have no potential to benefit is tragic. Each ounce that is sold in such a way is a waste of liquid gold and in essence is “stolen” away from the pool of milk that could be sent to a Human Milk Banking Association of North America approved Milk Bank. All Milk Banks that follow their standards provide breast milk which has is safe to consume as opposed to those sourced from online sites. Furthermore newer organizations such as the Mother’s Milk Coop pay for such milk as an alternative for mothers seeking income through the selling of their excess supply. There are of course possible issues that arise from paying mothers for their milk but if they are looking to profit then perhaps the coop is the preferred option. Selling milk and giving formula to their infants is not something I condone but if they are going to do it anyway the online route is the worse of the two options.
It is my hope that this post serves to educate even one mother that while their efforts to earn some income are understood there are better and safer ways to do so than an unregulated site such as “Only The Breast” or others. If you come across anyone who even hints at selling their milk through the means mentioned above, direct them to the closest breast milk bank or to the Coop mentioned above (recognizing that this too is not ideal)!
Finally, with the significant impact exclusive breast milk diets can have on outcomes for premature neonates hospitals worldwide would be wise to follow the lead of the University Hospital of Limerick who was just honoured for their initiative to ensure near 100% use of breast milk in their hospital through the use of donor milk.
Encourage your local hospitals to acquire donor breast milk if they don’t have a program to do so already. If they already have a program work with your health region to expand it.
Money very well spent I say.
by All Things Neonatal | Feb 27, 2015 | Pregnancy

The answer to this question seems to be quite elusive! In 2009 the American Society of Obstetricians and Gynecologists published a recommendation to avoid elective delivery of infants < 39 weeks gestational age.
http://bit.ly/1JT84fm
Induction after 41 but before 42 weeks was advised, however due to the increased rates of complications after 42 weeks including mortality, asphyxia and complications of having a large infant to name a few. This was also supported by the Cochrane Review on the same topic that can be found here: http://1.usa.gov/1E2aq8a
The decision to avoid elective delivery prior to 39 weeks was secondary to many published reports demonstrating that such deliveries had a higher chance of having babies born with complications, the most likely of which was respiratory distress leading to increased rates of NICU admissions. That being said the incidence of asphyxia in the same group was lower than if one waited until a later gestational age.
Since that time, the recommendations have been to avoid these elective deliveries but a recent article has been receiving a lot of press that suggests we have it all wrong. Outcomes may be better if one delivers prior to 37 weeks.
http://www.mirror.co.uk/news/world-news/inducing-labour-37-weeks-can-5181536
In this study from Denmark (published Feb 18th in the British Journal of Obstetrics and Gynecology) an enormous sample of patients (832935) over a ten year period were studied to determine outcomes for each pregnancy when one compared elective delivery prior to 37 weeks with c-sections or planned vaginal birth. Despite an adoption in Denmark of the recommendations as outlined above from ACOG, the incidence of delivery prior to 37 weeks increased significantly. What makes this article so sensational is that during this time the number of NICU admissions decreased in this cohort delivered prior to 37 weeks vs the expectant vaginal births. Concurrently the risk of cerebral palsy decreased, large babies decreased and also less nerve injuries after birth but strangely with an increase in the incidence of shoulder dystocia. The original article abstract is found here: http://1.usa.gov/1MXaE2U
Before I go on I feel the need to state the obvious. As a man I have no idea what it is like to be pregnant although I do know that as women approach and then pass the 37 week mark of their pregnancy, many are enamoured with the idea of giving birth ASAP. I have no doubt there is an appeal to this research study explaining why so much press has been devoted to this paper. It suggests an action that many women I believe would be more than happy to accept but is it the right way to go?
The short answer is I don’t know for sure. The authors do a fairly good job of looking at variables that might have influenced outcomes such as maternal age, smoking rates, number of prior pregnancies etc but one has to question what variables may have influenced outcomes that were not measured? Looking at a massive number of patients gives a robustness to the results but it also means that you have collected a sample over a large period of time. Over a ten year period, practices can change, new technologies become implemented and new NICUs may be built all of which may account for an improvement in outcome over time. This is not to say that the authors are not on to something here but it does give one reason to pause and question how one study can have such a different result than many others that have come before it.
I think that the authors in this case took the right path and acknowledge at the end of the article that more work must be done in essence to confirm the findings. As a Neonatologist I am very interested to see if further work in the area will confirm these findings in a modern cohort.
If they do though will we have the capacity to deal with the increased number of admissions if it turns out they are wrong. Only time will tell.

by All Things Neonatal | Feb 26, 2015 | Vaccination
Sucrose given to newborns prior to anticipated painful procedures has been used for many years now. The pooled evidence as presented by the Cochrane Database of Systematic Reviews concludes that “Sucrose is safe and effective for reducing procedural pain from single painful events (heel lance, venepuncture).” As care providers for newborns in an Intensive care setting we have become accustomed to providing this sugar to infants prior to such procedures and there is no question that we note the benefit in both subjective assessment of pain and when using more objective scoring systems.
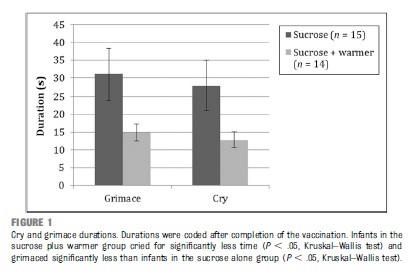
It is for this reason that I read with great interest the article by Gray L et al Pediatrics entitled Sucrose and Warmth for Analgesia in Healthy Newborns: An RCT. The study included 29 infants roughly half of which were randomized to sucrose 1 mL/kg of a 25% solution (Sweet-Ease) and the other to the same solution plus placement on an overhead warmer prior to Hepatitis B immunization. The results demonstrated a reduction in crying with both interventions compared to the sucrose alone as shown in the following figure.
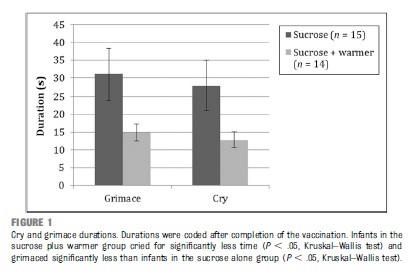
An additional finding was that of a dampening of heart rate acceleration if the infant received warmth as well. There is no question that the combination of warmth and sucrose is superior to providing sucrose alone but is the study relevant today?
The infants in this paper were recruited in 2008 at a time when we as a profession were not as accustomed to Kangaroo Care or Skin to Skin care as it is also known. In the study the overhead warmer was used as a substitute for Skin to Skin care but in 2016 would we do this? Perhaps if the mother was unavailable but certainly not if we could put the infant against the mother’s chest and provide sucrose. While the study has its merits I think it fails a critical test in order to apply it in our own practice. The question must always be asked no matter what the size of an effect “Can the results of the study be applied to my patient population?”
I fear in this case the answer is no for most of our infants. The paper serves as a good reminder that while results of a study may be valid, they might just not be useful in your own practice.
Antipyretics or Sucrose for Vaccine Related Pain?
Future questions though that come to mind are whether sucrose analgesia may be useful in older children at 2,4 and 6 months. Previous research has demonstrated that while fever may be effectively treated with prophylactic antipyretics the additional finding is that of reduced antibody production to some vaccine antigens. While a reduction has been noted, even with reduced levels protection remains as the threshold for immunity is not crossed. This has been evaluated in a systematic review in 2014 pertaining to the same topic. As some practitioners though now advise against such prophylaxis might sucrose be the replacement? This has been studied in 16-19 month olds receiving a series of vaccinations and found to be an effective pain reliever as demonstrated in the paper Oral sucrose administration to reduce pain response during immunization in 16-19-month infants: a randomized, placebo-controlled trial. While the results of the study demonstrate effectiveness to reduce pain the effect on the immune response remains unanswered.
What the future will hold I don’t know but if you are looking for another option for pain relief other than acetaminophen or ibuprofen you may wish to ask your practitioner about a little sugar next time.
by All Things Neonatal | Feb 25, 2015 | Vaccination

What?! A doctor speaking out against pro-vaccination? No I haven’t switched to the other side but a recent headline caught my eye due to its potential to create a social crisis.
Imagine you have just had a baby and friends of yours who you know have not vaccinated her children want to come by for a visit. (see link) Do you freak out and deny them entry as Kristin Bell would suggest or do you ask a few questions (more delicately than “do your children have measles” and allow the visit to happen?
It seemed like a good opportunity to calm people’s nerves by reminding them of why it is that your Pediatrician will not offer the MMR vaccine prior to the age of 1 year. If you have been vaccinated as a child then you generally will have lifelong immunity to measles. The Centre For Disease Control claims that the immunity is 95% after one dose and virtually 100% after the booster dose to measles, mumps and rubella. If the vaccine though is so effective why not give it before a year to protect your vulnerable infant? The answer lies in the natural immunity that is passed from mother to fetus in the form of IgG antibodies that cross the placenta. These antibodies offer protection to the fetus and then newborn and may circulate in the infants bloodstream until 1 year of age. In essence your infant is protected from measles by virtue of your parents being sensible and vaccinating you when you were a child. The benefits of breastfeeding by passing on further antibody protection are additive (see link)!
So before anyone accuses me of being careless let me restate that I would not expose my own child under a year of age to a child that was suspected of having measles but I often worry about the effect of one celebrity sharing information such as this and the social isolation that may ensue for those parents who choose for whatever reason not to immunize. Let us also not forget that there are legitimate reasons for not immunizing your children and should these children be ostracized?
Links:
http://www.huffingtonpost.com/2015/02/17/kristen-bell-vaccinations_n_6699368.html
http://www.ncbi.nlm.nih.gov/pubmed/19133867
by All Things Neonatal | Feb 25, 2015 | General Comments
I hope you bear with me as I venture into the realm of blogging. I have no doubt there will be both good and bad but I hope with time less of the latter. The goal of this is to stimulate shared learning by putting my thoughts out and hopefully getting feedback in return. Thanks in advance for your comments and I hope that the journey is worthwhile.
Michael