
by All Things Neonatal | Dec 28, 2017 | preemie, Prematurity, technology, ventilation
Intubation is not an easy skill to maintain with the declining opportunities that exist as we move more and more to supporting neonates with CPAP. In the tertiary centres this is true and even more so in rural centres or non academic sites where the number of deliveries are lower and the number of infants born before 37 weeks gestational age even smaller. If you are a practitioner working in such a centre you may relate to the following scenario. A woman comes in unexpectedly at 33 weeks gestational age and is in active labour. She is assessed and found to be 8 cm and is too far along to transport. The provider calls for support but there will be an estimated two hours for a team to arrive to retrieve the infant who is about to be born. The baby is born 30 minutes later and develops significant respiratory distress. There is a t-piece resuscitator available but despite application the baby needs 40% oxygen and continues to work hard to breathe. A call is made to the transport team who asks if you can intubate and give surfactant. Your reply is that you haven’t intubated in quite some time and aren’t sure if you can do it. It is in this scenario that the following strategy might be helpful.
Surfactant Administration Through and Laryngeal Mask Airway (LMA)
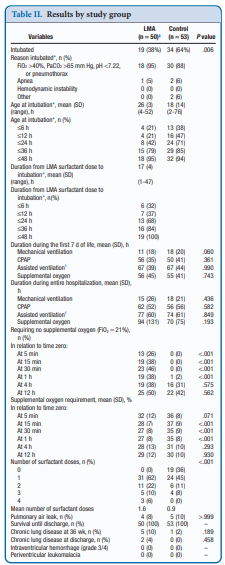
Use of an LMA has been taught for years in NRP now as a good choice to support ventilation when one can’t intubate. The device is easy enough to insert and given that it has a central lumen through which gases are exchanged it provides a means by which surfactant could be instilled through a catheter placed down the lumen of the device. Roberts KD et al published an interesting unmasked but randomized study on this topic Laryngeal Mask Airway for Surfactant Administration in Neonates: A Randomized, Controlled Trial. Due to size limitations (ELBWs are too small to use this in using LMA devices) the eligible infants included those from 28 0/7 to 35 6/7 weeks and ≥1250 g. The infants needed to all be on CPAP +6 first and then fell into one of two treatment groups based on the following inclusion criteria: age ≤36 hours,
(FiO2) 0.30-0.40 for ≥30 minutes (target SpO2 88% and 92%), and chest radiograph and clinical presentation consistent with RDS.
Exclusion criteria included prior mechanical ventilation or surfactant administration, major congenital anomalies, abnormality of the airway, respiratory distress because of an etiology other than RDS, or an Apgar score <5 at 5 minutes of age.
Procedure & Primary Outcome
After the LMA was placed a y-connector was attached to the proximal end. On one side a CO2 detector was placed and then a bag valve mask in order to provide manual breaths and confirm placement over the airway. The other port was used to advance a catheter and administer curosurf in 2 mL aliquots. Prior to and then at the conclusion of the procedure the stomach contents were aspirated and the amount of surfactant determined to provide an estimate of how much surfactant was delivered to the lungs. The primary outcome was treatment failure necessitating intubation and mechanical ventilation in the first 7 days of life. Treatment failure was defined upfront and required 2 of the following: (1) FiO2 >0.40 for >30
minutes (to maintain SpO2 between 88% and 92%), (2) PCO2 >65 mmHg on arterial or capillary blood gas or >70 on venous blood gas, or (3) pH <7.22 or 1 of the following: (1) recurrent or severe apnea, (2) hemodynamic instability requiring pressors, (3) repeat surfactant dose, or (4) deemed necessary by medical provider.
Did it work?
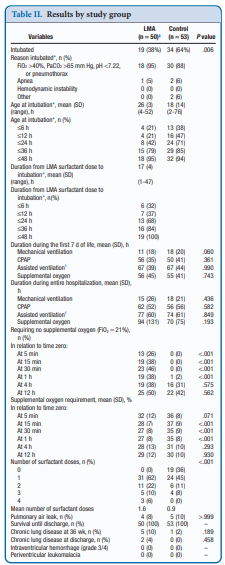
It actually did. Of the 103 patients enrolled (50 LMA and 53 control) 38% required intubation in the LMA group vs 64% in the control arm. The authors did not reach their desired enrollment based on their power calculation but that is ok given that they found a difference. What is really interesting is that they found a difference in the clinical end point despite many infants clearly not receiving a full dose of surfactant as measured by gastric aspirate. Roughly 25% of the infants were found to have not received any surfactant, 20% had >50% of the dose in the stomach and the other 50+% had < 10% of the dose in the stomach meaning that the majority was in fact deposited in the lungs. I suppose it shouldn’t come as a surprise that among the secondary outcomes the duration length of mechanical ventilation did not differ between two groups which I presume occurred due to the babies needing intubation being similar. If you needed it you needed it so to speak. Further evidence though of the effectiveness of the therapy was that the average FiO2 30 minutes after being treated was significantly lower in the group with the LMA treatment 27 vs 35%. What would have been interesting to see is if you excluded the patients who received little or no surfactant, how did the ones treated with intratracheal deposition of the dose fare? One nice thing to see though was the lack of harm as evidenced by no increased rate of pneumothorax, prolonged ventilation or higher oxygen.
Should we do this routinely?
There was a 26% reduction in intubations in te LMA group which if we take this as the absolute risk reduction means that for every 4 patients treated with an LMA surfactant approach, one patient will avoid intubation. That is pretty darn good! If we also take into account that in the real world, if we thought that little of the surfactant entered the lung we would reapply the mask and try the treatment again. Even if we didn’t do it right away we might do it hours later.
In a tertiary care centre, this approach may not be needed as a primary method. If you fail to intubate though for surfactant this might well be a safe approach to try while waiting for a more definitive airway. Importantly this won’t help you below 28 weeks or 1250g as the LMA is too small but with smaller LMAs might this be possible. Stay tuned as I suspect this is not the last we will hear of this strategy!

by All Things Neonatal | Nov 16, 2017 | Neonatal, Neonatology, preemie, Prematurity
Given that today is world prematurity day it seems fitting to talk about prematurity at the absolute extreme of it.
It has been some time since as a regional program we came to accept that we would offer resuscitation to preterm infants born as early as 23 weeks gestational age. This is perhaps a little later in the game that other centers but it took time to digest the idea that the rate of intact survival was high enough to warrant a trial of resuscitation. This of course is not a unilateral decision but rather a decision arrived at after consultation with the family and interprofessional team. To be sure it is not an easy one. Other centers have argued that resuscitation should be offered to those infants as young as 22 weeks gestational age and data now exists due to enough centres doing so to provide families with some guidance as to expected survival rates and importantly the likelihood of disability. This topic has been covered previously in /2015/09/25/winnipeg-hospital-about-to-start-resuscitating-infants-at-23-weeks/. Why cover this topic again? Well an article on CNN might have something to do with it.
Resuscitating Below 22 weeks
This week as I was perusing the news I came across a rather shocking article on CNN. Born before 22 weeks, ‘most premature’ baby is now thriving.  The article tells the tale of a baby delivered at 21 weeks and 4 days that now as a three year old is reaching appropriate milestones without any significant impairments. It is a story that is filled with inspiration and so I am not mistaken I am delighted for this child and their family that this outcome has occurred. When the lay press latches onto stories like this there is no doubt a great deal of sensationalism to them and in turn that gathers a lot of attention. This in turn is a great thing for media.
The article tells the tale of a baby delivered at 21 weeks and 4 days that now as a three year old is reaching appropriate milestones without any significant impairments. It is a story that is filled with inspiration and so I am not mistaken I am delighted for this child and their family that this outcome has occurred. When the lay press latches onto stories like this there is no doubt a great deal of sensationalism to them and in turn that gathers a lot of attention. This in turn is a great thing for media.
A Few Caveats Though
With the exception of pregnancies conceived through IVF the best dating we have is only good to about +/- 5 days when an early first trimester ultrasound is performed or the date of the last menstrual period is fairly certain. A baby though who is born at 21 weeks + 4 days may in fact be 22 +3 days or even more depending on when the dating was done (second trimester worse). Let’s not take away though from the outcome being this good even at 22 weeks. That is a pretty perfect outcome for this family but the point is that this baby may in fact be older than 21 weeks.
Secondly, there are millions of babies born each year in North America. Some of these infants are born at 22 weeks. How do they fare overall? From the paper by Rysavy et al from 2015 the results are as follows.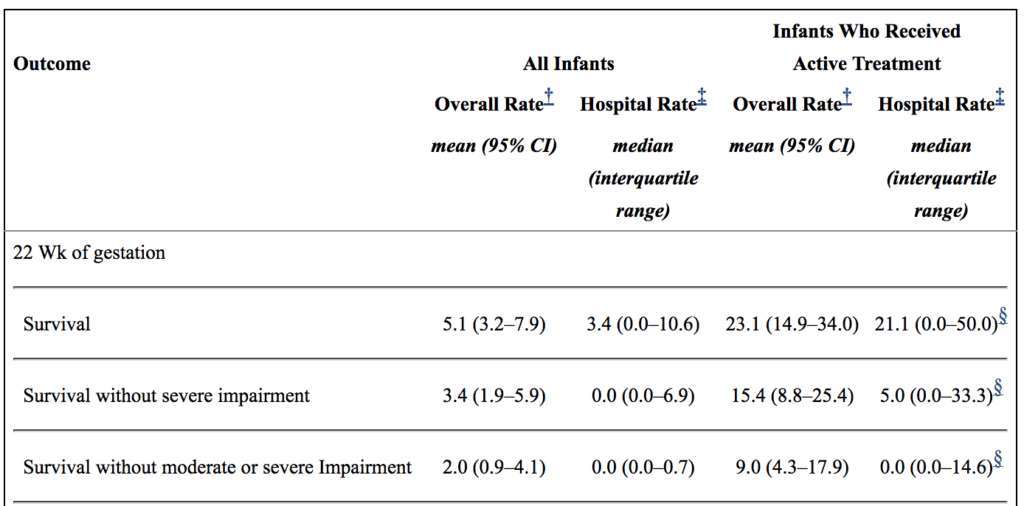
If you look at the overall rate of survival it is on an average of 5.1%. If you take a look though at those infants in whom resuscitation is provided that number increases to a mean of 23%. Intact survival is 9% overall. The odds aren’t great but they are there and I suspect the infant in the article is one of those babies. Flipping the argument though to the glass is half empty, 91% of infants born at 22 weeks by best estimate who are offered resuscitation will have a moderate or severe disability or die. I am not saying what one should do in this situation but depending on how a family processes the data they will either see the 110 chance of intact survival as a good thing or a 9/10 chance of death or disability as a very bad thing. What a family chooses though is anyone’s best guess.
Should we resuscitate below 22 weeks if the family wishes?
I guess in the end this really depends on a couple things. First off, how certain are the dates? If there is any degree of uncertainty then perhaps the answer is yes. If the dates are firm then I at least believe there is a barrier at which futility is reached. Perhaps this isn’t at 21 weeks as some patients may indeed be older but think about what you would offer if a family presented at 20 weeks and wanted everything done. What if it were 19 weeks? I suspect the point of futility for all lies somewhere between 19-21 weeks.
As I prepare to attend the annual meeting in Ottawa tomorrow for the Fetus and Newborn Committee I think it is prudent to point out just how difficult all of this is. The current statement on Counselling and management for anticipated extremely preterm birth I think hits on many of these issues. The statement is the product on not only the think tank that exists on this committee but was the product of a national consultation. I know I may be biased since I sit on the committee but I do believe it really hits the mark.
Should we be thinking about resuscitating at 21 weeks? For me the answer is one clouded by a whole host of variables and not one that can be easily answered here. What I do think though is that the answer in the future may be a yes provided such infants can be put onto an artificial placenta.  Even getting a few more weeks of growth before aerating those lungs is necessary may make all the difference. The NICUs of tomorrow certainly may look quite different than they do now.
Even getting a few more weeks of growth before aerating those lungs is necessary may make all the difference. The NICUs of tomorrow certainly may look quite different than they do now.
by All Things Neonatal | Oct 19, 2017 | BPD, Neonatal, Neonatology, preemie, Prematurity
If you work in Neonatology then chances are you have ordered or assisted with obtaining many chest x-rays in your time. If you look at home many chest x-rays some of our patients get, especially the ones who are with us the longest it can be in the hundreds. I am happy to say the tide though is changing as we move more and more to using other imaging modalities such as ultrasound to replace some instances in which we would have ordered a chest x-ray. This has been covered before on this site a few times; see Point of Care Ultrasound in the NICU, Reducing Radiation Exposure in Neonates: Replacing Radiographs With Bedside Ultrasound. and Point of Care Ultrasound: Changing Practice For The Better in NICU.This post though is about something altogether different.
If you do a test then know what you will do with the result before you order it.
If there is one thing I tend to harp on with students it is to think about every test you do before you order it. If the result is positive how will this help you and if negative what does it tell you as well. In essence the question is how will this change your current management. If you really can’t think of a good answer to that question then perhaps you should spare the infant the poke or radiation exposure depending on what is being investigated. When it comes to the baby born before 30 weeks these infants are the ones with the highest risk of developing chronic lung disease. So many x-rays are done through their course in hospital but usually in response to an event such as an increase in oxygen requirements or a new tube with a position that needs to be identified. This is all reactionary but what if you could do one x-ray and take action based on the result in a prospective fashion?
What an x-ray at 7 days may tell you
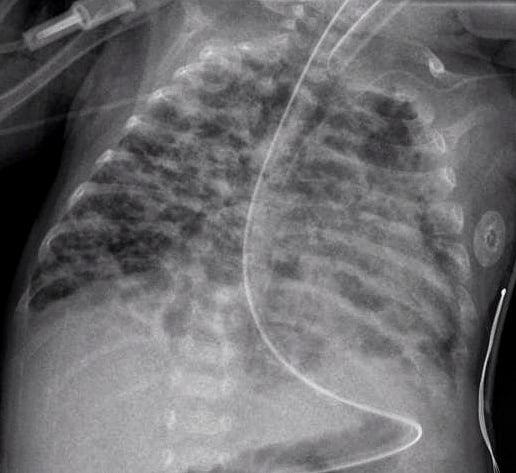
How many times have you caught yourself looking at an x-ray and saying out loud “looks like evolving chronic lung disease”. It turns out that Kim et al in their publication Interstitial pneumonia pattern on day 7 chest radiograph predicts bronchopulmonary dysplasia in preterm infants.believe that we can maybe do something proactively with such information.
In this study they looked retrospectively at 336 preterm infants weighing less than 1500g and less than 32 weeks at birth. Armed with the knowledge that many infants who have an early abnormal x-ray early in life who go on to develop BPD, this group decided to test the hypothesis that an x-ray demonstrating a pneumonia like pattern at day 7 of life predicts development of BPD.  The patterns they were looking at are demonstrated in this figure from the paper. Essentially what the authors noted was that having the worst pattern of the lot predicted the development of later BPD. The odds ratio was 4.0 with a confidence interval of 1.1 – 14.4 for this marker of BPD. Moreover, birthweight below 1000g, gestational age < 28 weeks and need for invasive ventilation at 7 days were also linked to the development of the interstitial pneumonia pattern.
The patterns they were looking at are demonstrated in this figure from the paper. Essentially what the authors noted was that having the worst pattern of the lot predicted the development of later BPD. The odds ratio was 4.0 with a confidence interval of 1.1 – 14.4 for this marker of BPD. Moreover, birthweight below 1000g, gestational age < 28 weeks and need for invasive ventilation at 7 days were also linked to the development of the interstitial pneumonia pattern.
What do we do with such information?
I suppose the paper tells us something that we have really already known for awhile. Bad lungs early on predict bad lungs at a later date and in particular at 36 weeks giving a diagnosis of BPD. What this study adds if anything is that one can tell quite early whether they are destined to develop this condition or not. The issue then is what to do with such information. The authors suggest that by knowing the x-ray findings this early we can do something about it to perhaps modify the course. What exactly is that though? I guess it is possible that we can use steroids postnatally in this cohort and target such infants as this. I am not sure how far ahead this would get us though as if I had to guess I would say that these are the same infants that more often than not are current recipients of dexamethasone.
Would another dose of surfactant help? The evidence for late surfactant isn’t so hot itself so that isn’t likely to offer much in the way of benefit either.
In the end the truth is I am not sure if knowing concretely that a patient will develop BPD really offers much in the way of options to modify the outcome at this point. Having said that the future may well bring the use of stem cells for the treatment of BPD and that is where I think such information might truly be helpful. Perhaps a screening x-ray at 7 days might help us choose in the future which babies should receive stem cell therapy (should it be proven to work) and which should not. I am proud to say I had a chance to work with a pioneer in this field of research who may one day cure BPD. Dr. Thebaud has written many papers of the subject and if you are looking for recent review here is one Stem cell biology and regenerative medicine for neonatal lung diseases.Do I think that this one paper is going to help us eradicate BPD? I do not but one day this strategy in combination with work such as Dr. Thebaud is doing may lead us to talk about BPD at some point using phrases like “remember when we used to see bad BPD”. One can only hope.

by All Things Neonatal | Sep 7, 2017 | preemie, Prematurity, ventilation
A grenade was thrown this week with the publication of the Australian experience comparing three epochs of 1991-92, 1997 and 2005 in terms of long term respiratory outcomes. The paper was published in the prestigious New England Journal of Medicine; Ventilation in Extremely Preterm Infants and Respiratory Function at 8 Years. This journal alone gives “street cred” to any publication and it didn’t take long for other news agencies to notice such as Med Page Today. The claim of the paper is that the modern cohort has fared worse in the long run. This has got to be alarming for anyone reading this! As the authors point out, over the years that are being compared rates of antenatal steroid use increased, surfactant was introduced and its use became more widespread and a trend to using non-invasive ventilation began. All of these things have been associated with better short term outcomes. Another trend was declining use of post-natal steroids after 2001 when alarms were raised about the potential harm of administering such treatments.
Where then does this leave us?
I suppose the first thing to do is to look at the study and see if they were on the mark. To evaluate lung function the study looked at markers of obstructive lung disease at 8 years of age in survivors from these time periods. All babies recruited were born between 22-27 completed weeks so were clearly at risk of long term injury. Measurements included FEV1, FVC, FVC:FEV1 and FEF 25-75%. Of the babies measured the only two significant findings were in the FEV1 and ratio of FEV1:FVC. The former showed a drop off comparing 1997 to 2005 while the latter was worse in 2005 than both epochs.
| Variable |
1991-92 |
1997 |
2005 |
| %predicted value |
N=183 |
N=112 |
N=123 |
| FEV1 |
87.9+/-13.4 |
92.0+/-15.7 |
85.4+/-14.4 |
| FEV1:FVC |
98.3+/-10 |
96.8+/-10.1 |
93.4+/-9.2 |
This should indeed cause alarm. Babies born in a later period when we thought that we were doing the right things fared worse. The authors wonder if perhaps a strategy of using more CPAP may be a possible issue. Could the avoidance of intubation and dependence on CPAP for longer periods actually contribute to injury in some way? An alternative explanation might be that the use of continuous oximetry is to blame. Might the use of nasal cannulae with temporary rises in O2 expose the infant to oxygen toxicity?
There may be a problem here though
Despite everyone’s best efforts survival and/or BPD as an outcome has not changed much over the years. That might be due to a shift from more children dying to more children living with BPD. Certainly in our own centre we have seen changes in BPD at 36 weeks over time and I suspect other centres have as well. With concerted efforts many centres report better survival of the smallest infants and with that they may survive with BPD. The other significant factor here is after the extreme fear of the early 2000s, use of postnatal steroids fell off substantially. This study was no different in that comparing the epochs, postnatal glucocorticoid use fell from 40 and 46% to 23%. One can’t ignore the possibility that the sickest of the infants in the 2005 cohort would have spent much more time on the ventilator that their earlier counterparts and this could have an impact on the long term lung function.
Another question that I don’t think was answered in the paper is the distribution of babies at each gestational age. Although all babies were born between 22-27 weeks gestational age, do we know if there was a skewing of babies who survived to more of the earlier gestations as more survived? We know that in the survivors the GA was not different so that is reassuring but did the sickest possible die more frequently leaving healthier kids in the early cohorts?
This bigger issue interestingly is not mentioned in the paper. Looking at the original cohorts there were 438 in the first two year cohort of which 203 died yielding a survival of 54% while in 1997 survival increased to 70% and in 2005 it was 65%. I can’t help but wonder if the drop in survival may have reflected a few more babies at less than 24 weeks being born and in addition the holding of post natal steroids leading to a few more deaths. Either way, there are enough questions about the cohorts not really being the same that I think we have to take the conclusions of this paper with a grain of salt.
It is a sensational suggestion and one that I think may garner some press indeed. I for one believe strongly though as I see our rates of BPD falling with the strategies we are using that when my patients return at 8 years for a visit they will be better off due to the strategies we are using in the current era. Having said that we do have so much more to learn and I look forward to better outcomes with time!

by All Things Neonatal | Aug 10, 2017 | newborn, preemie, Prematurity, resuscitation, ventilation
I know how to bag a baby. At least I think I do. Providing PPV with a bag-valve mask is something that you are taught in NRP and is likely one of the first skills you learned in the NICU. We are told to squeeze the bag at a rate of 40-60 breaths a minute. According to the Laerdal website, the volume of the preterm silicone bag that we typically use is 240 mL. Imagine then that you are wanting to ventilate a baby who is 1 kg. How much should you compress the bag if you wish to delivery 5 mL/kg. Five ml out of a 240 mL bag is not a lot of squeeze is it? Think about that the next time you find yourself squeezing one. You might then say but what about a t-piece resuscitator? A good choice option as well but how much volume are you delivering if you set the initial pressures at 20/5 for example? That would depend on the compliance of the lung of course. The greater the compliance the more volume would go in. Would it be 5 mL, 10 ml or even 2.5 mL based on the initial setting? Hard to say as it really depends on your seal and the compliance of the lung at the pressure you have chosen. If only we had a device that could deliver a preset volume just like on a ventilator with a volume guarantee setting!
Why is this holy grail so important?
It has been over 30 years since the importance of volutrauma was demonstrated in a rabbit model. Hernandez LA et al published Chest wall restriction limits high airway pressure-induced lung injury in young rabbits. The study used three models to demonstrate the impact of volume as opposed to pressure on injuring the lung of preterm rabbits. Group 1 were rabbit ventilated at pressures of 15/30/45 cm H2O for one hour, group 2 rabbits with a cast around their thorax to limit volume expansion and group 3 sets of excised lungs with no restriction to distension based on the applied pressures. As you might expect, limitation of over distension by the plaster cast led the greatest reduction in injury (measured as microvascular permeability) with the excised lungs being the worst. In doing this study the authors demonstrated the importance of over distension and made the case for controlling volume more than pressure when delivering breaths to avoid excessive tidal volume and resultant lung injury.
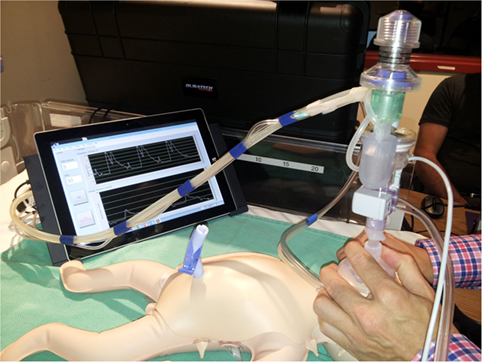
The “Next Step” Volume Ventilator BVM
Perhaps I am becoming a fan of the Edmonton group. In 2015 they published A Novel Prototype Neonatal Resuscitator That Controls Tidal Volume and Ventilation Rate: A Comparative Study of Mask Ventilation in a Newborn Manikin. The device is tablet based and as described, rather than setting a PIP to deliver a Vt, a rate is set along with a volume to be delivered with a peep in this case set at +5. 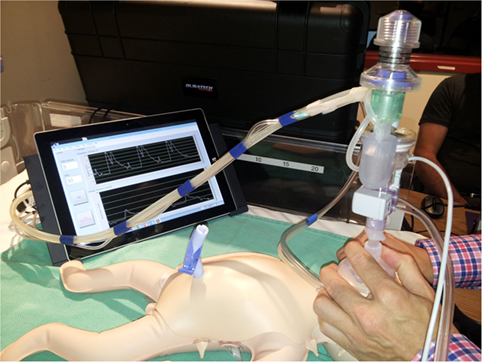 This study compared 5 different methods of delivering PPV to a 1 kg preterm manikin. The first was a standard self inflating bag, the next three different t-piece resuscitators and then the Next Step. For the first four the goal was to deliver a pressure of 20/5 at a rate of 40-60 breaths per minute. A test lung was connected to the manikin such that each device was used for a one minute period at three different levels of compliance (0.5 ml/cmH2O, 1.0 ml/cmH2O and then 2.0 ml/cm H2O representing increasing compliance. The goal of the study was to compare the methods in terms of delivering a volume of 5 mL to this 1 kg model lung. The order in which the devices were used was randomized for the 25 participants in the study who were all certified in NRP and included some Neonatologists.
This study compared 5 different methods of delivering PPV to a 1 kg preterm manikin. The first was a standard self inflating bag, the next three different t-piece resuscitators and then the Next Step. For the first four the goal was to deliver a pressure of 20/5 at a rate of 40-60 breaths per minute. A test lung was connected to the manikin such that each device was used for a one minute period at three different levels of compliance (0.5 ml/cmH2O, 1.0 ml/cmH2O and then 2.0 ml/cm H2O representing increasing compliance. The goal of the study was to compare the methods in terms of delivering a volume of 5 mL to this 1 kg model lung. The order in which the devices were used was randomized for the 25 participants in the study who were all certified in NRP and included some Neonatologists.
Some Concerning Findings
As I said at the beginning, we all like to think we know how to ventilate a newborn with BVM. The results though suggest that as compliance increases our ability to control how much volume we deliver to a lung based on a best guess for pressures needed is lacking. One caveat here is that the pressures set on the t-piece resucitators were unchanged during the 1 minute trials but then again how often during one minute would we change settings from a starting point of 20/5?
|
|
Vt (mL) |
|
|
0.5 mL/cmH20 |
1.0 mL/cmH20 |
2.0mL/cmH20 |
| Self inflating |
11.4 |
17.6 |
23.5 |
| Neo-Tee |
5.6 |
11.2 |
19.3 |
| Neopuff |
6.1 |
10 |
21.3 |
| Giraffe |
5.7 |
10.9 |
19.8 |
| Next Step |
3.7 |
4.9 |
4.5 |
Without putting in all the confidence intervals I can tell you that the Next Step was the tightest. What you notice immediately (or at least I did) was that no matter what the compliance, the self inflating bag delivers quite an excessive volume even in experienced hands regardless of compliance. At low compliance the t-piece resuscitators do an admirable job as 5-6 ml/kg of delivered Vt is reasonable but as compliance improves the volumes increase substantially. It is worth pointing out that at low compliance the Next Step was unable to deliver the prescribed Vt but knowing that if you had a baby who wasn’t responding to ventilation I would imagine you would then try a setting of 6 ml/kg to compensate much like you would increase the pressure on a typical device. How might these devices do in a 29 week infant for example with better compliance than say a 24 week infant? You can’t help but wonder how many babies are given minutes of excessive Vt after birth during PPV with the traditional pressure limited BVM setup and then down the road how many have BPD in part because of that exposure.
I wanted to share this piece as I think volume resuscitation will be the future. This is just a prototype or at least back then it was. Interestingly in terms of satisfaction of use, the Next Step was rated by the participants in the study as being the easiest and most comfortable to use of all the devices studied. Adding this finding to the accuracy of the delivered volume and I think we could have a winner.



 The article tells the tale of a baby delivered at 21 weeks and 4 days that now as a three year old is reaching appropriate milestones without any significant impairments. It is a story that is filled with inspiration and so I am not mistaken I am delighted for this child and their family that this outcome has occurred. When the lay press latches onto stories like this there is no doubt a great deal of sensationalism to them and in turn that gathers a lot of attention. This in turn is a great thing for media.
The article tells the tale of a baby delivered at 21 weeks and 4 days that now as a three year old is reaching appropriate milestones without any significant impairments. It is a story that is filled with inspiration and so I am not mistaken I am delighted for this child and their family that this outcome has occurred. When the lay press latches onto stories like this there is no doubt a great deal of sensationalism to them and in turn that gathers a lot of attention. This in turn is a great thing for media.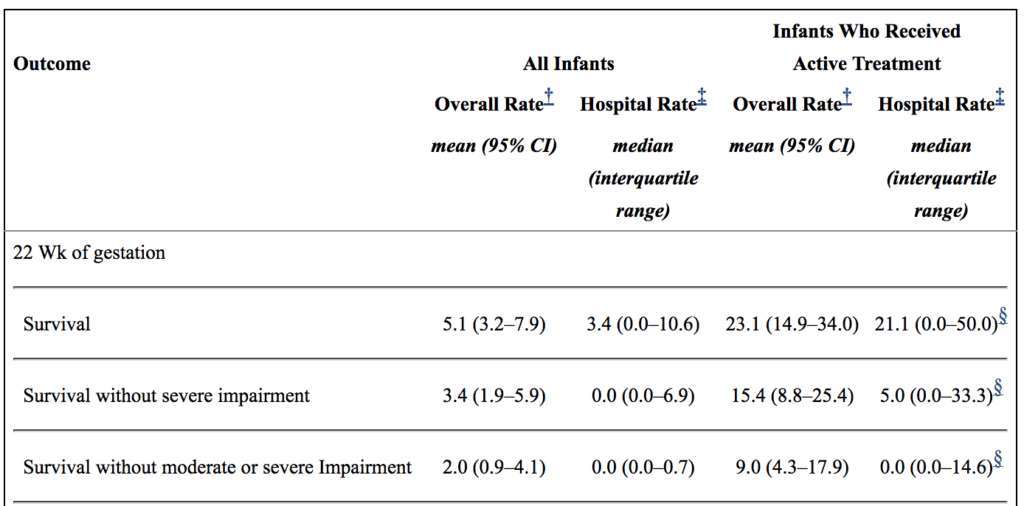
 Even getting a few more weeks of growth before aerating those lungs is necessary may make all the difference. The NICUs of tomorrow certainly may look quite different than they do now.
Even getting a few more weeks of growth before aerating those lungs is necessary may make all the difference. The NICUs of tomorrow certainly may look quite different than they do now.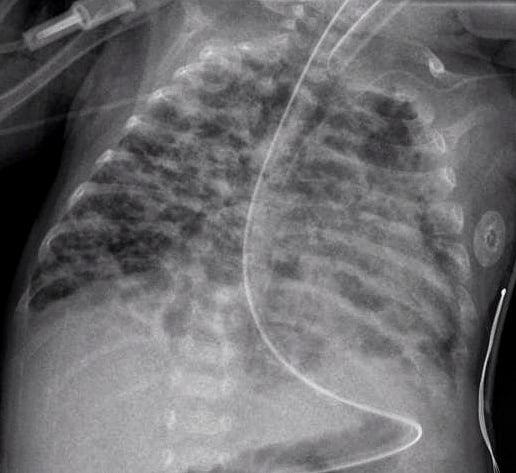
 The patterns they were looking at are demonstrated in this figure from the paper. Essentially what the authors noted was that having the worst pattern of the lot predicted the development of later BPD. The odds ratio was 4.0 with a confidence interval of 1.1 – 14.4 for this marker of BPD. Moreover, birthweight below 1000g, gestational age < 28 weeks and need for invasive ventilation at 7 days were also linked to the development of the interstitial pneumonia pattern.
The patterns they were looking at are demonstrated in this figure from the paper. Essentially what the authors noted was that having the worst pattern of the lot predicted the development of later BPD. The odds ratio was 4.0 with a confidence interval of 1.1 – 14.4 for this marker of BPD. Moreover, birthweight below 1000g, gestational age < 28 weeks and need for invasive ventilation at 7 days were also linked to the development of the interstitial pneumonia pattern.

 This study compared 5 different methods of delivering PPV to a 1 kg preterm manikin. The first was a standard self inflating bag, the next three different t-piece resuscitators and then the Next Step. For the first four the goal was to deliver a pressure of 20/5 at a rate of 40-60 breaths per minute. A test lung was connected to the manikin such that each device was used for a one minute period at three different levels of compliance (0.5 ml/cmH2O, 1.0 ml/cmH2O and then 2.0 ml/cm H2O representing increasing compliance. The goal of the study was to compare the methods in terms of delivering a volume of 5 mL to this 1 kg model lung. The order in which the devices were used was randomized for the 25 participants in the study who were all certified in NRP and included some Neonatologists.
This study compared 5 different methods of delivering PPV to a 1 kg preterm manikin. The first was a standard self inflating bag, the next three different t-piece resuscitators and then the Next Step. For the first four the goal was to deliver a pressure of 20/5 at a rate of 40-60 breaths per minute. A test lung was connected to the manikin such that each device was used for a one minute period at three different levels of compliance (0.5 ml/cmH2O, 1.0 ml/cmH2O and then 2.0 ml/cm H2O representing increasing compliance. The goal of the study was to compare the methods in terms of delivering a volume of 5 mL to this 1 kg model lung. The order in which the devices were used was randomized for the 25 participants in the study who were all certified in NRP and included some Neonatologists.