by All Things Neonatal | Sep 6, 2018 | Neonatal, Neonatology, newborn, preemie
It has been a few months now that I have been serving as Chair of the Fetus and Newborn Committee for the Canadian Pediatric Society. Certain statements that we release resonate strongly with me and the one just released this week is certainly one of them. Guidelines for vitamin K prophylaxis in newborns is an important statement about a condition that thankfully so few people ever experience. To read the statement on the CPS website click here.
Similar story to vaccinations
Prior to the American Academy of Pediatrics in 1961 proclaiming that all newborns should receive IM Vitamin K at birth the incidence of Vitamin K deficient bleeding was 0.25 – 1.7%. Think about that for a moment. A new parent could expect that 1/100 babies roughly might have intestinal bleeding or worse an intracranial hemorrhage due to an insufficient amount of vitamin K levels in the newborn. The types of bleeding could be categorized into three different time epochs. Early onset (occurring in the first 24 hours post-birth), classic (occurring at days 2 to 7) and late onset (at 2 to 12 weeks and up to 6 months of age).
With a rate that high detractors of providing Vitamin K at birth would say “why should we give it; I haven’t heard of any baby getting such bleeding?” Looking at it another way though, why don’t you see congenital rubella or kids with measles much these days? It’s due to vaccination. Thankfully as a Neonatologist, I don’t see Vitamin K deficient bleeding since most parents provide Vitamin K to their babies at birth. If you went back to the era prior to 1961 when widespread supplementation of Vitamin K began in the US, I imagine it would not have been too uncommon to hear about a baby who had bleeding issues after birth. Just because we don’t hear about German Measles much anymore doesn’t mean the virus causing it doesn’t still exist!
How Effective is Vitamin K?
How effective is Vitamin K administration at birth in preventing hemorrhagic disease of the newborn (HDNB)? Studies estimate an incidence of 0.25 per 100000 live births or 1 in 400000 babies vs the 1/100 risk without any vitamin K. That is one effective intervention! At this point I would ask those families that are still concerned about giving Vitamin K to their infants if this is a risk they can accept? If they refuse Vitamin K and there is a significant bleed how will they react?
The Change in this CPS Statement From the Past
In the last statement on Vitamin K, the authors suggested that the oral route was a reasonable option. Instead of giving 1 mg of Vitamin K IM one would dose it as 2 mg orally and then repeat at 2-4 weeks and then 6-8 weeks. In looking at the effectiveness though it is worth noting that while we can assure that families will get the first dose, as with any medication that needs repeat dosing there is the risk of forgetfulness leading to missed dosing down the road. In fact when the authors looked at the risk of late HDNB they found the following “The relative risk for VKDB, when comparing PO versus IM vitamin K administration in these two studies, was 28.75 (95% CI 1.64 to 503.45) and 5.97 (95% CI 0.54 to 65.82), respectively [19][20].”
The outcome of course remains rare but the risk based on two studies was almost 30 times higher than if IM dosing was given.
On this basis IM is recommended.
Having said all this I recognize that despite all this information, some families will choose for a number of reasons to still opt for the oral dose. As the statement suggests we need to encourage such use when a family refuses IM vitamin K. The 30 fold risk compared to IM administration is magnitudes lower than the approximate 1/100 risk of giving nothing at all!
In the end I believe that one case of intracranial hemorrhage from inadequate vitamin K is too much. This one vitamin indeed could save a life.

by All Things Neonatal | Jun 30, 2018 | intubation, Neonatal, Neonatology, newborn, preemie, Prematurity
A few weeks back I wrote about the topic of intubations and whether premedication is really needed (Still performing awake intubations in newborns? Maybe this will change your mind.) I was clear in my belief that it is and offered reasons why. There is another group of practitioners though that generally agree that premedication is beneficial but have a different question. Many believe that analgesia or sedation is needed but question the need for paralysis. The usual argument is that if the intubation doesn’t go well and the patient can’t spontaneously ventilate could we be worse off if the patient loses their muscle tone.
Neonatal Intubation Registry
At the CPS meeting last month in Quebec City. I had the pleasure of listening to a talk by Dr. Elizabeth Foglia on the findings from a Neonatal intubation registry that many centres have been contributing to. The National Emergency Airway Registry for Neonates (NEAR4NEOs), records all intubations from a number of centres using an online database and allows for analysis of many different aspects of intubations in neonates.
This year, J. Krick et al published Premedication with paralysis improves intubation success and decreases adverse events in very low birth weight infants: a prospective cohort study. This study compared results from the registry of two centres, the University of Washington Medical Center (UWMC) and Seattle Children’s Hospital where the former rarely uses paralysis and the latter in almost all instances of non-emergent intubation. In all, 237 encounters were analyzed in the NICU for babies < 1500g with the majority of encounters (181) being from UWMC. The median PMA at intubation was 28 completed weeks (IQR: 27, 30), chronological age was 9 days (IQR: 2, 26) and weight was 953 g (IQR: 742,1200). The babies were compared based on the following groups. Premedication with a paralytic 21%, without a paralytic 46% and no premedication 31%.
This was an observational study that examined the rates of adverse events and subdivided into severe (cardiac arrest, esophageal intubation with delayed recognition, emesis with witnessed aspiration, hypotension requiring intervention (fluid and/or vasopressors), laryngospasm, malignant hyperthermia, pneumothorax/pneumomediastinum, or direct airway injury) vs non-severe (mainstem bronchial intuba- tion, esophageal intubation with immediate recognition, emesis without aspiration, hypertension requiring therapy, epistaxis, lip trauma, gum or oral trauma, dysrhythmia, and pain and/or agitation requiring additional medication and causing a delay in intubation.).
How did the groups compare?
It turns out paralysis seems to be a big deal (at least in this group of infants). Use of paralysis resulted in less attempts to intubate (median 1 attempt; IQR: 1, 2.25 vs. 2; IQR: 1, 3, p < 0.05)). In fact success was no different between the groups with no paralysis or no premedication at all! When it comes to tracheal intubation adverse events the impact of using paralysis becomes more evident. 
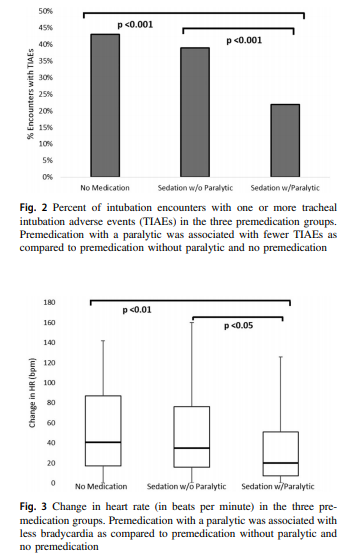 Paralysis does make a difference in reducing the incidence of such events and moreover when only looking at the rate of severe adverse events as defined above the finding was that none occurred when paralysis was used vs 9 when no paralysis was employed and 5 when no premedication was used at all. The rate of bradycardic events was less in the paralytic group but rates of oxygen desaturation between the three arms were no different.
Paralysis does make a difference in reducing the incidence of such events and moreover when only looking at the rate of severe adverse events as defined above the finding was that none occurred when paralysis was used vs 9 when no paralysis was employed and 5 when no premedication was used at all. The rate of bradycardic events was less in the paralytic group but rates of oxygen desaturation between the three arms were no different.
How do we interpret the results?
Based on the results from the registry it looks like paralysis is a good thing here when electively intubating infants. If we try to determine the reason for it I suspect it may have much to do with the higher likelihood of success on the first attempt at placing an ETT. The longer it takes to place the ETT or the more number of attempts requiring intermittent PPV in a patient who truly needs a tube the greater the likelihood that you will see adverse events including bradycardia. It may simply be that a calm and still patient is an easier intubation and getting the tube in faster yields a more stable patient.
I am biased though and I think it is worth pointing out another possible reason for the differing results. One hospital in this study routinely used premedication and the other did not. Almost 3/4 of the patients came from one hospital which raises the possibility that skill set could be playing a role. If the skill of providers at the two hospitals differed, the results could reflect the variable skill in the practitioners versus the difference in the medications used themselves. What I don’t know though is whether the two share the same training program or not. Are the trainees the same at both sites (google maps says the two sites are 11 minutes away by car)? The difference still might be in local respiratory therapists or Neonatologists intubating as well. Regardless, the study provides evidence that paralysis makes a difference. To convince those out there though who remain skeptical I think we are going to need the registry to take part in a prospective trial using many centres. A format in which several centres that don’t use paralysis are compared to several who do routinely would help to sort out the concern in skill when looking only at two centres. This wouldn’t be randomized of course but I think it would be very difficult at this point to get a centre that strongly believes in using paralysis to randomize so a prospective study using groups chosen by the individual centre might be the next best thing. If anyone using the registry is reading this let me know what you think?
by All Things Neonatal | Mar 22, 2018 | Developmental care, kangaroo care, Neonatology, newborn
Skin to skin care or kangaroo care is all the rage and I am the first one to offer my support for it. Questions persist though as to whether from a physiological standpoint, babies are more stable in an isolette in a quiet environment or out in the open on their mother or father’s chests. Bornhorst et al expressed caution in their study Skin-to-skin (kangaroo) care, respiratory control, and thermoregulation. In a surprising finding, babies with an average gestational age of 29 weeks were monitored for a number of physiological parameters and found to have more frequent apnea and higher heart rates than when in an isolette. The study was small though and while there were statistical differences in these parameters they may not have had much clinical significance (1.5 to 2.8 per hour for apnea, bradycardia or desaturation events). Furthermore, does an increase in such events translate into any changes in cerebral oxygenation that might in turn have implications for later development? Tough to say based on a study of this magnitude but it certainly does raise some eyebrows.
What if we could look at cerebral oxygenation?
As you might have guessed, that is exactly what has been done by Lorenz L et al in their recent paper Cerebral oxygenation during skin-to-skin care in preterm infants not receiving respiratory support.The goal of this study was to look at 40 preterm infants without any respiratory distress and determine whether cerebral oxygenation (rStO2)was better in their isolette or in skin to skin care (SSC). They allowed each infant to serve as their own control by have three 90 minute periods each including the first thirty minutes as a washout period. Each infant started their monitoring in the isolette then went to SSC then back to the isolette. The primary outcome the power calculation was based on was the difference in rStO2 between SSC and in the isolette. Secondary measures looked at such outcomes as HR, O2 sat, active and quiet sleep percentages, bradycardic events as lastly periods of cerebral hypoxia or hyperoxia. Normal cerebral oxygenation was defined as being between 55 to 85%.
Surprising results?
Perhaps its the start of a trend but again the results were a bit surprising showing a better rStO2 when in the isolette (−1.3 (−2.2 to −0.4)%, p<0.01). Other results are summarized in the table below:
| Mean difference in outcomes |
| Variable |
SSC |
Isolette |
Difference in mean |
p |
| rStO2 |
73.6 |
74.8 |
-1.3 |
<0.01 |
| SpO2 (median) |
97 |
97 |
-1.1 |
0.02 |
| HR |
161 |
156 |
5 |
<0.01 |
| % time in quiet sleep |
58.6 |
34.6 |
24 |
<0.01 |
No differences were seen in bradycardic events, apnea, cerebral hypoexmia or hyperoxemia. The authors found that SSC periods in fact failed the “non-inferiority” testing indicating that from a rStO2 standpoint, babies were more stable when not doing SSC! Taking a closer look though one could argue that even if this is true does it really matter? What is the impact on a growing preterm infant if their cerebral oxygenation is 1.3 percentage points on average lower during SSC or if their HR is 5 beats per minute faster? I can’t help but think that this is an example of statistical significance without clinical significance. Nonetheless, if there isn’t a superiority of these parameters it does leave one asking “should we keep at it?”
Benefits of skin to skin care
Important outcomes such as reductions in mortality and improved breastfeeding rates cannot be ignored or the positive effects on family bonding that ensue. Some will argue though that the impacts on mortality certainly may be relevant in developing countries where resources are scarce but would we see the same benefits in developed nations. The authors did find a difference though in this study that I think benefits developing preterm infants across the board no matter which country you are in. That benefit is that of Quiet Sleep (QS). As preterm infants develop they tend to spend more time in QS compared to active sleep (AS). From Doussard- Roossevelt J, “Quiet sleep consists of periods of quiescence with regular respiration and heart rate, and synchronous EEG patterns. Active sleep consists of periods of movement with irregular respiration and heart rate, and desynchronous EEG patterns.” In the above table one sees that the percentage of time in QS was significantly increased compared to AS when in SSC. This is important as neurodevelopment is thought to advance during periods of QS as preterm infants age.
There may be little difference favouring less oxygen extraction during isolette times but maybe that isn’t such a good thing? Could it be that the small statistical difference in oxygen extraction is because the brain is more active in laying down tracks and making connections? Totally speculative on my part but all that extra quiet sleep has got to be good for something.
To answer the question of this post in the title I think the answer is a resounding yes for the more stable infant. What we don’t know at the moment except from anecdotal reports of babies doing better in SSC when really sick is whether on average critically ill babies will be better off in SSC. I suspect the answer is that some will and some won’t. While we like to keep things simple and have a one size fits all answer for most of our questions in the NICU, this one may not be so simple. For now I think we keep promoting SSC for even our sick patients but need to be honest with ourselves and when a patient just isn’t ready for the handling admit it and try again when more stable. For the more stable patient though I think giving more time for neurons to find other neurons and make new connections is a good thing to pursue!

by All Things Neonatal | Jan 15, 2018 | BPD, Neonatal, Neonatology, newborn, outcome, preemie, Prematurity, steroids
This must be one of my favourite topics as I have been following the story of early hydrocortisone to reduce BPD for quite some time. It becomes even more enticing when I have met the authors of the studies previously and can see how passionate they are about the possibilities. The PREMILOC study was covered on my site twice now, with the first post being A Shocking Change in Position. Postnatal steroids for ALL microprems? and the second reviewing the 22 month outcome afterwards /2017/05/07/early-hydrocortisone-short-term-gain-without-long-term-pain/.
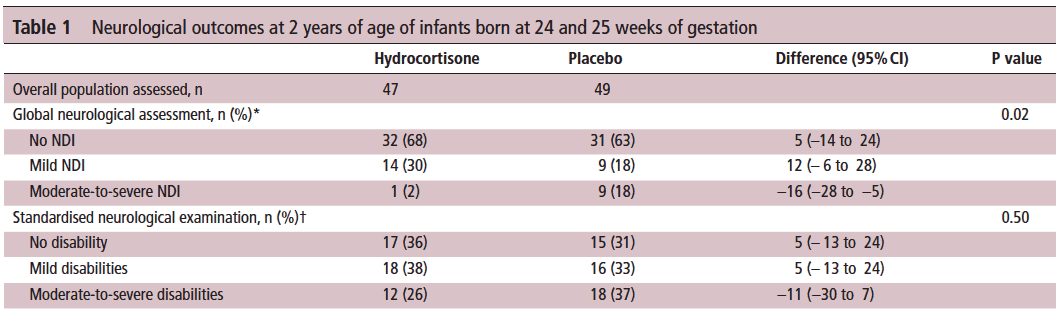
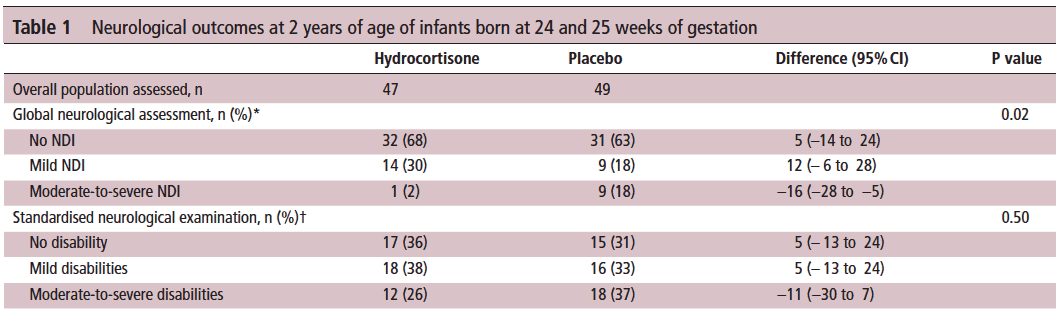
The intervention here was that within 24 hours of birth babies born between 24-27 weeks gestational age were randomized to receive placebo or hydrocortisone 1 mg/kg/d divided q12h for one week followed by 0.5 mg/kg/d for three days. The primary outcome was rate of survival without BPD at 36 weeks PMA. The finding was a positive one with a 9% reduction in this outcome with the use of this strategy. Following these results were the two year follow-up which reported no evidence of harm but the planned analysis by gestational age groupings of 24-25 and 26-27 weeks was not reported at that time but it has just been released this month.
Is there a benefit?
Of the original cohort the authors are to be commended here as they were able to follow-up 93% of all infants studied at a mean age of 22 months. The methods of assessing their neurological status have been discussed previously but essentially comprised standardized questionnaires for parents, assessment tools and physical examinations.
Let’s start off with what they didn’t find. There was no difference between those who received placebo vs hydrocortisone in the 26-27 week group but where it perhaps matters most there was. The infants born at 24-25 weeks are certainly some of our highest risk infants in the NICU. It is in this group that the use of hydrocortisone translated into a statistically significant reduction in the rate of neurodevelopmental impairment. The Global Neurological Assessement scores demonstrated a significant improvement in the hydrocortisone group with a p value of 0.02. Specifically moderate to severe disability was noted in 18% compared to 2% in the group receiving hydrocortisone.They did not find a difference in the neurological exam but that may reflect the lack of physical abnormalities with cognitive deficit remaining. It could also be explained perhaps by the physical examination not being sensitive enough to capture subtle differences.
Why might this be?
Adding an anti-inflammatory agent into the early phase of a preemies life might spare the brain from white matter damage. Inflammation is well known to inflict injury upon the developing brain and other organs (think BPD, ROP) so dampening these factors in the first ten days of life could bring about such results via a mechanism such as that. When you look at the original findings of the study though, a couple other factors also pop up that likely contribute to these findings as well. Infants in the hydrocortisone group had a statistical reduction in the rate of BPD and PDA ligations. Both of these outcomes have been independently linked to adverse neurodevelopmental outcome so it stands to reason that reducing each of these outcomes in the most vulnerable infants could have a benefit.
In fact when you add everything up, is there much reason not to try this approach? Ten days of hydrocortisone has now been shown to reduce BPD, decrease PDA ligations and importantly in the most vulnerable of our infants improve their developmental outcome. I think with this information at our fingertips it becomes increasingly difficult to ignore this approach. Do I think this will become adopted widely? I suspect there will be those who take the Cochrane approach to this and will ask for more well designed RCTs to be done in order to replicate these results or at least confirm a direction of effect which can then be studied as part of a systematic review. There will be those early adopters though who may well take this on. It will be interesting to see as these centres in turn report their before and after comparisons in the literature what the real world impact of this approach might be.
Stay tuned as I am sure this is not the last we will hear on this topic!

by All Things Neonatal | Sep 22, 2017 | neonatal abstinence, Neonatology, newborn
As someone with an interest in neonatal abstinence (NAS) I am surprised that I missed this study back in May. Anyone who says they aren’t interested in NAS research must be turning a blind eye to the North American epidemic of patients filling neonatal units or postpartum wards in need of treatment for the same. News feeds such as CNN have covered this story many times with concerning articles such as this published “Opioid Crisis Fast Facts” even the Trump White House has officially declared it as an emergency at this point. With NICU resources stretched and care providers fatigue levels wearing thin (these patients are typically very challenging to take care of due to the crying and agitation with neurological excitability that is at the core of the symptoms, something needs to be done. The vast majority of neonatal care providers treat such patients with an approach that promotes first non pharmacologic strategies such as keeping mom and baby together when possible, breast feeding and disturbing these infants as little as possible to name a few points. For those patients though who require pharmacologic support though, the mainstay has been oral morphine. At least in our units though once a patient is admitted and undergoes treatment we are still looking at anywhere from 3-4 weeks on average that they will occupy a hospital bed. If only there was a better way.
Could Buprenorphine do the trick?
While morphine is widely used to treat NAS symptoms unresponsive to other non pharmacologic methods of control, buprenorphine has a similar profile as an opioid but has less risk of respiratory depression as a partial agonist. A small but important trial has been published directly comparing the use of morphine to buprenorphine for treatment of NAS symptoms with the primary outcome being days of treatment and the second important point being length of stay. The trial, Buprenorphine for the Treatment of the Neonatal Abstinence Syndrome.by Kraft WK et al was entitled the BBORN trial for short. This was a single centre trial in which a double blind/double dummy approach was used. By double dummy this meant that after randomization those babies randomized to morphine received morphine plus a buprenorphine placebo and the other arm received a buprenorphine dose and a morphine placebo. In total 33 infants were randomized to buprenorphine and 30 to morphine (hence my comment about this being a small study). Their power calculation had called for 40 infants per arm to detect a 28% difference in the primary end point of duration of treatment but in the end that didn’t matter so much as they found a significant difference exceeding their estimate anyway. A lack of power would have become important mind you had they not found a difference as they wouldn’t have actually had the numbers to do so.
A strength of the study up front was that all care providers scored NAS symptoms the same way (need to take into account there is some subjectivity in scoring altogether though) and escalations and decreases of medication were done following a strict protocol both ways. In both arms, once a maximal dose of 60 mcg/kg of body weight for buprenorphine and 1.2 mg/kg for morphine was reached phenobarbital was added. When comparing the two groups at the outset there were no significant differences in characteristics so two generally similar populations of infants were being treated.
The Results Were Indeed Impressive
Before launching into the table, there were 21 babies in both groups that were bottle fed and 12 in the burprenorphine group and 9 in the morphine group that breastfed.
| Outcome |
Buprenorphine |
Morphine |
p |
| Median days of treatment |
15 (3-67) |
28 (13-67) |
<0.001 |
| Bottle feeding |
15 (3-67) |
28 (13-67) |
|
| Breast feeding |
20 (3-55) |
28 (16-52) |
|
|
|
|
|
| Hospital stay in days |
21 (7-71) |
33 (18-70) |
<0.001 |
| Bottle feeding |
21 (7-71) |
33 (18-70) |
|
| Breast feeding |
26 (7-58) |
32 (20-58) |
|
No difference was seen in those who needed phenobarbital. Looking at the table, a couple things really stand out to me. They were looking for a 28% reduction in days of treatment. The results came in far excess of that at a 46% reduction. Curiously, breastfeeding which has classically been associated with a reduction in scores and therefore faster weaning due to less symptoms seemed to have the opposite effect here. Does this imply that breastfeeding slows down both duration of treatment and length of stay as a result? With a study this small it is difficult to say with so few breastfed babies but if I had to guess I would suggest those mothers that worked at breastfeeding may have had longer stays.
Should we all jump on the buprenorphine train?
For now I would give this a big maybe. One of the concerns about burprenorphine is that it comes as a solution of 30% alcohol. Giving multiple doses (3 per day in this study) of such a solution could in part contribute to these results of lower NAS symptoms. Is giving alcohol to reduce symptoms a good idea here? Not sure if there are any long term effects and moreover if the cumulative dose of this medication would be of a concern. Definitely something to check with your local pharmacist before rolling this out. On the other hand if the dose of alcohol provided was truly significant I might have expected the burprenorphine group to be poorer feeders due to intoxication which we certainly did not see.
With increasing volumes of newborns afflicted with symptoms of NAS we do need to find a way to stem the tide. Ideally, primary preventative strategies would be best but until that solution is found could burprenorphine be the next step in tackling this epidemic?

by All Things Neonatal | Sep 13, 2017 | Neonatal, Neonatology, newborn, preemie, Prematurity, resuscitation, ventilation
We can always learn and we can always do better. At least that is something that I believe in. In our approach to resuscitating newborns one simple rule is clear. Fluid must be replaced by air after birth and the way to oxygenate and remove CO2 is to establish a functional residual capacity. The functional residual capacity is the volume of air left in the lung after a tidal volume of air is expelled in a spontaneously breathing infant and is shown in the figure. Traditionally, to establish this volume in a newborn who is apneic, you begin PPV or in the spontaneously breathing baby with respiratory distress provide CPAP to help inflate the lungs and establish FRC.
Is there another way?
Something that has been discussed now for some time and was commented on in the most recent version of NRP was the concept of using sustained inflation (SI) to achieve FRC. I have written about this topic previously and came to a conclusion that it wasn’t quite ready for prime time yet in the piece Is It Time To Use Sustained Lung Inflation In NRP?
The conclusion as well in the NRP textbook was the following:
“There are insufficient data regarding short and long-term safety and the most appropriate duration and pressure of inflation to support routine application of sustained inflation of greater than 5 seconds’ duration to the transitioning newborn (Class IIb, LOE B-R). Further studies using carefully designed protocols are needed”
So what now could be causing me to revisit this concept? I will be frank and admit that whenever I see research out of my old unit in Edmonton I feel compelled to read it and this time was no different. The Edmonton group continues to do wonderful work in the area of resuscitation and expand the body of literature in such areas as sustained inflation.
Can you predict how much of a sustained inflation is needed?
This is the crux of a recent study using end tidal CO2 measurement to determine whether the lung has indeed established an FRC or not. Dr. Schmolzer’s group in their paper (Using exhaled CO2 to guide initial respiratory support at birth: a randomised controlled trial) used end tidal CO2 levels above 20 mmHg to indicate that FRC had been established. If you have less CO2 being released the concept would be that the lung is actually not open. There are some important numbers in this study that need to be acknowledged. The first is the population that they looked at which were infants under 32 6/7 weeks and the second is the incidence of BPD (need for O2 or respiratory support at 36 weeks) which in their unit was 49%. This is a BIG number as in comparison for infants under 1500g our own local incidence is about 11%. If you were to add larger infants closer to 33 weeks our number would be lower due to dilution. With such a large number though in Edmonton it allowed them to shoot for a 40% reduction in BPD (50% down to 30%). To accomplish this they needed 93 infants in each group to show a difference this big.
So what did they do?
For this study they divided the groups in two when the infant wouldn’t breathe in the delivery room. The SI group received a PIP of 24 using a T-piece resuscitator for an initial 20 seconds. If the pCO2 as measured by the ETCO2 remained less than 20 they received an additional 10 seconds of SI. In the PPV group after 30 seconds of PPV the infants received an increase of PIP if pCO2 remained below 20 or a decrease in PIP if above 20. In both arms after this phase of the study NRP was then followed as per usual guidelines.
The results though just didn’t come through for the primary outcome although ventilation did show a difference.
| Outcome |
SI |
PPV |
p |
| BPD |
23% |
33% |
0.09 |
| Duration of mechanical ventilation (hrs) |
63 |
204 |
0.045 |
The reduction in hours of ventilation was impressive although no difference in BPD was seen. The problem though with all of this is what happened after recruitment into the study. Although they started with many more patients than they needed, by the end they had only 76 in the SI group and 86 in the PPV group. Why is this a problem? If you have less patients than you needed based on the power calculation then you actually didn’t have enough patients enrolled to show a difference. The additional compounding fact here is that of the Hawthorne Effect. Simply put, patients who are in a study tend to do better by being in a study. The observed rate of BPD was 33% during the study. If the observed rate is lower than expected when the power calculation was done it means that the number needed to show a difference was even larger than the amount they originally thought was needed. In the end they just didn’t have the numbers to show a difference so there isn’t much to conclude.
What I do like though
I have a feeling or a hunch that with a larger sample size there could be something here. Using end tidal pCO2 to determine if the lung is open is in and of itself I believe a strategy to consider whether giving PPV or one day SI. We already use colorimetric devices to determine ETT placement but using a quantitative measure to ascertain the extent of open lung seems promising to me. I for one look forward to the continued work of the Neonatal Resuscitation–Stabilization–Triage team (RST team) and congratulate them on the great work that they continue doing.




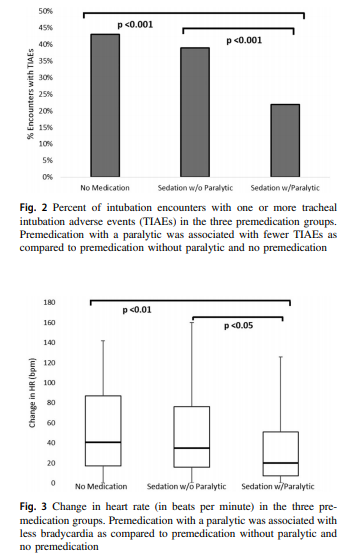 Paralysis does make a difference in reducing the incidence of such events and moreover when only looking at the rate of severe adverse events as defined above the finding was that none occurred when paralysis was used vs 9 when no paralysis was employed and 5 when no premedication was used at all. The rate of bradycardic events was less in the paralytic group but rates of oxygen desaturation between the three arms were no different.
Paralysis does make a difference in reducing the incidence of such events and moreover when only looking at the rate of severe adverse events as defined above the finding was that none occurred when paralysis was used vs 9 when no paralysis was employed and 5 when no premedication was used at all. The rate of bradycardic events was less in the paralytic group but rates of oxygen desaturation between the three arms were no different.