by All Things Neonatal | Feb 11, 2016 | hand hygiene, Infection, Uncategorized
I don’t know about you but I have deeply rooted memories from the 1990s of donning a yellow gown and gloves before examining each and every patient on my list before rounds. This was done as we firmly believed such precautions were needed to prevent the spread of infections in the NICU. As time went on though the gowns were removed and not long after so went the gloves as priority was placed on performance of good hand hygiene to reduce rates of infection in our units.
You can imagine that after having it entrenched in my mind that hand hygiene was the key to success that I would find it surprising to see a paper published a few months ago suggesting that the use of gloves after hand hygiene may offer a benefit after all. Kaufman DA et al published Nonsterile glove use in addition to hand hygiene to prevent late-onset infection in preterm infants: randomized clinical trial and given it’s challenge to a practice that is at least two decades old I thought it may be worth sharing with you the reader.
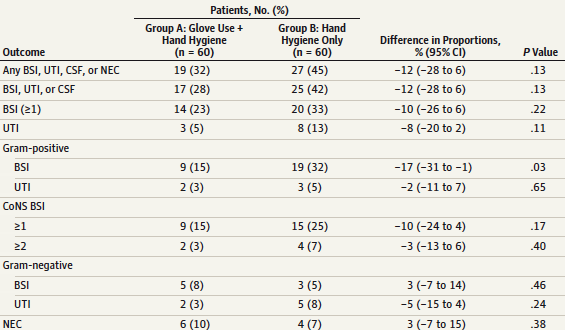
Essentially the authors hypothesized that the use of non-sterile gloves after performing hand hygiene (compared to hand hygiene alone) would reduce late-onset invasive infection (>72 hours after birth), defined as 1 or more episodes per patient of a BSI, urinary tract infection,meningitis, and/orNEC associated with clinical signs and symptoms of infection and treated with antimicrobials. When determining the size of study needed, they used a baseline incidence of 60% and looked to find a 25% reduction in their outcome. Unfortunately for them (although very fortunate for their patients, the incidence of LOS in the experimental arm was 32% with a 45% incidence in the control group (hand hygiene alone). What does this mean when your expected rate is higher than your observed? In short you need more patients to show a difference and indeed they failed to show a significant difference between the two groups. They did however find a difference in gram positive infections being 15 vs 32% p=0.03 and seem to take some comfort in this finding. If you were to give the paper a quick read you might be impressed with the finding and might even shrug your shoulders and say the common expression “Can’t hurt but might help” Maybe we should adopt this?
Not so Fast
There is a significant potential source of error here that needs to be addressed. The definition of a proven blood stream infection as per the CDC is two positive cultures for the same organism. In this study only one culture was required to be positive so the potential for diagnostic error is high. In our own centre although unpublished we have noted since adopting a mandatory two culture collection approach for LOS that there have been a significant number of occasions where one culture was noted to be positive and the other negative. Antibiotics in these cases have been stopped (for gram positive organisms) after 48 hours without consequence. In this study however the findings of increased rates of positive cultures in the hand hygiene only group is heavily influenced by the presence of only one positive culture as is seen in this table.
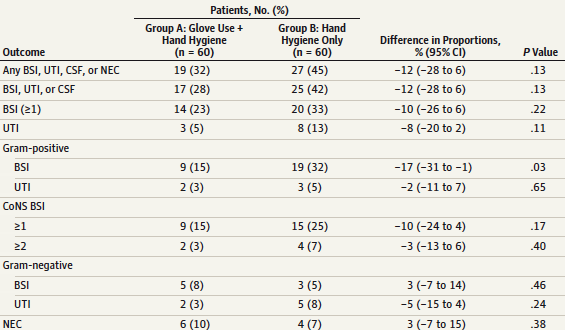
When looking at the numbers of times there were greater than or equal to 2 positive cultures in the CoNS group one sees the vast majority were only based on one culture. Furthermore, of the 20 infections in the hand hygiene only group, 19 were gram positve CoNS of which only 4 had more than one culture. Based on this finding and the lack of any other significant difference in infectious outcomes the proof that gloves add anything to reducing infection rates is tough to argue.
Could Gloves Actually Make Things Worse?
Several studies have actually indicated that wearing gloves reduces hand hygiene compliance. One such study although in adults “The dirty hand in the latex glove”: a study of hand hygiene compliance when gloves are worn. suggests that this is indeed the case with a 9% decrease in proper hand hygiene when gloves were worn. Others such as Flores in 2006 found similar poor perfomance when gloves were used Healthcare workers’ compliance with glove use and the effect of glove use on hand hygiene. I would speculate that although we all want to do what is best for our patients there may be a psychological trick being played here. Perhaps knowing we will cover up with gloves leads people to take shortcuts on hand hygiene as they subconciously think they will be covered anyway. Never mind that the “dirty” hand touches the gloves they will put on making proper hand hygiene a must.
Conclusion
It certainly was a shock to see such a paper as I saw flashes of my past yellow gowned self coming back to haunt me. Based on my take of this paper however I would say that at least for the time being I will take my time, wash my hands before and after every patient encounter and keep the gloves around for handling those yet unbathed newborns. Spend your energy where it counts and that is ensuring your hands are properly cleaned before touching your patient or lines.
by All Things Neonatal | Apr 2, 2015 | cancer, Infection, Innovation, oncology, Vaccination
The following piece is by my first guest blogger Dr. Simon Trepel MD, FRCPC whom I have known most of my life and am delighted to present his work here. Simon is a Child Psychiatrist who has been touched by cnacer and has written a fascinating and touching piece below.
My wife, Kerri Tymchuk, died a bit over 2 years ago, at age 35, from metastatic breast cnacer. She left behind a loving husband and 2 beautiful daughters, ages 1 and 3, at the time of her death, at the claws of cnacer. I still can barely look at that word, or give it the decency of either spelling it correctly, or ever capitalizing it again. I remember having a similar reaction as a naive young child learning about the Jewish faith, and having a hard time with the word Jesus, as I could not reconcile a Messiah to come with one who had already come. Since then, Jesus and I are fine, and I am getting along well hoping for another. My point was that the word cnacer, to me, has become so strong, its power rivals the very existentialist crisis I had as a young boy.
The reason I am telling you this, is because anything relating to cnacer now sets off alarm bells in my head, as if my mortal enemy has mutated in rage again. I feel fear, and remember Kerri. And I whisper to her that she will be avenged when we learn which types of silver bullets work best on this beast that steals lives in every phase of the moon.
So I was captivated to learn on 60 minutes that there is a physician and research team that has seemingly discovered a possible miracle breakthrough in treating a very specific and deadly brain cnacer, called glioblastoma, or gb for short, spelled correctly. It seems that Dr. Annick Desjardins and the Duke cnacer Research Team have found that if you inject the polio virus directly into even the most aggressive gb tumors, the tumors replication, or ability to make unlimited copies of itself, is permanently stopped. It’s like unplugging cnacer’s Xerox machine. Once that happens, the polio virus then wreaks havoc in the gb cells themselves, and over the weeks and months to follow, your immune system beats up the schoolyard cranial bully until there is NOTHING LEFT.
Well, this got me thinking a bit about what we can do to potentially protect ourselves even better, in case we ever get gb ourselves, or it occurs, heaven forbid, in one of our children or extended family. The speed at which the cnacer cells in gb are destroyed depends on the immune system of white blood cells and other special cells. Some of these immune cells remember very well the viruses that egged the front porch of our face with a head cold or caused pneumonia or fever. If that same bacteria or virus comes around again, the immune system is exponentially better at mounting a response and ending the illness much quicker. The immune system also has the ability to recognize and destroy cnacer cells. Most cnacers are tricky, and go unnoticed in your body, wearing a disguise with a name tag that says ‘please look away while I kill you’. Incredibly, the polio virus, once it affects gb cells, seems to pull the mask off, and once this occurs, your own personal secret service, the immune system, rushes in, and blasts the cnacer dead like 007 (at least so far in the more than dozen formerly terminal patients who have responded to this form of treatment) .
The punch line of this short essay is to say that right now, you have the ability to potentially greatly improve your chances of surviving cnacer! At the very least, this breakthrough has been demonstrated in a highly malignant (able to double in size every 2 weeks) form of cnacer. If infecting other types of cnacers in a similar way, or with a different virus, also works, we may have a bona fide potential cure for cnacer on our hands. And our loved one’s can stay longer to live their lives.
This is not an infomercial for a new tropical berry juice or something that Jenny McCarthy is going to like. Getting immunized as a child with the regularly scheduled polio vaccination causes your immune system to recognize and destroy ANY cell (including cnacer cells) that have been infected with polio. Your immune system will respond more efficiently and faster, compared to never being immunized against polio. If infecting other types of cancers shows the same result, you may immediately get a huge head start on your future cnacer treatment by ensuring that you and your children are immunized according to the Health Canada Vaccination Schedule. For those anti vaccination people out there, at least consider the polio one. Once you are vaccinated against polio, your immune system will act like it is on steroids (the Ben Johnson kind) and you will beat polio infected glioblastoma, or perhaps all cnacers, in a similar fashion. Please think about it.

by All Things Neonatal | Mar 23, 2015 | Infection, Innovation
I came across an article from the BBC about a company in Israel that has developed a kit which can determine the presence of bacteria or virus in the blood of a patient within a two-hour window. More than that the kit has a point of care device as shown below.
Imagine for a moment the impact of being able to determine the presence or absence of sepsis within a two-hour window. Infants who have respiratory distress with a plan to assess in four-hours to determine need for antibiotics would never receive a dose. Other infants who were given one dose of ampicillin and gentamicin at birth would not need any further doses if the test indicated no bacteria or viruses present. Now you might say what is the harm in providing 48 hours of antibiotics or even 5 days if you are unsure of the presence of sepsis? There probably is little harm in a couple of days but the practice of prolonging antibiotics for fear that a patient has suspected sepsis is quite common in Neonatal circles. A recent article by Greenwood C et al (http://1.usa.gov/1Ex4qlH) examined stools at 1, 2 and 3 weeks of premature infants exposed to either short 1-4 day or longer 5-7 day courses of antibiotics. The results were quite striking in that the neonates exposed to the longer duration experienced less bacterial diversity than the other group and a preponderance of Enterobacter. Curiously levels of Lactobacillus and Bifidobacteria were low in all groups which might suggest a role for probiotics or explain why they might have been shown to reduce NEC. In fact in this study higher rates of NEC, sepsis and death were noted in the group receiving prolonged courses!
I have written other posts in which I have commented on Probiotics so to be clear I am not advocating that we use them routinely but one does have to wonder if it would be worthwhile repopulating the intestine of an infant who legitimately needed a 7 day course for a proven infection. Perhaps this post will stimulate someone to do that very study.
Aside from the perturbed microbiome leading to NEC, sepsis and death we also now have evidence of many long-term effects from antibiotics. The one creating the most alarm in press is no doubt the emergence of “superbugs” but more recently evidence has started to mount that repeated courses of antibiotics in infancy may lead to adult obesity (http://bit.ly/18JIIj7) and childhood allergy (http://bit.ly/1LwBmBc).
Getting back to this new technology it would still seem to be in the early stages. Looking through the company’s website they are allowing people to apply to be an early adopter. Additionally the links to their publications are really presentations at this time. A Pubmed search failed to come up with any specific articles regarding these products to I would have to say we are still in this products infancy. That being said it is certainly exciting to speculate about the impact that this innovation could have especially the point of care device pictured above which would bring the diagnosis to the bedside! I would encourage you to look at MeMeds website as it has a lot of very good information and if you check in from time to time who knows, you might be the first to hear that the two-hour test for sepsis is ready for use in your unit somewhere.
MeMed
http://www.me-med.com/html5/sbs.py?_id=11045&did=2466&G=2466
by All Things Neonatal | Mar 17, 2015 | Breastfeeding, Breastmilk, Infection, Pregnancy
Its hard not to hear about probiotics these days. They are in our grocery stores as supplements to yoghurt and other foods and can be purchased in health food stores or at your local pharmacy. They appear to be everywhere as word spreads about the importance of your microbiome in maintaining good overall health.
It didn’t take long for clinician scientists to turn their attention to the neonate who is at risk of necrotizing enterocolits (NEC). It has been known for some time that formula feeding versus breast milk plays a role in the development of NEC as premature infants fed formula repeatedly were found across studies to have a higher incidence of NEC. The evidence is so strong in fact that the Cochrane review on the subject states “Enteral supplementation of probiotics prevents severe NEC and all cause mortality in preterm infants. Our updated review of available evidence strongly supports a change in practice.“ If you have read such reviews you know that they rarely come out this strong in their support of something! Furthermore, infants fed formula may have a different preponderance of more pathogenic bacteria in the colon and less lactobacillus and bifidobacterium species. The idea behind providing probiotics to neonates would therefore be to repopulate the intestine of these vulnerable infants with good bacteria and potentially reduce the incidence of a devastating condition like NEC.
If only it were that easy though
The issue of using Probiotics in preterm infants is a contentious one to say the least. While the evidence appears to indicate an overall benefit in terms of reducing rates of NEC there remain concerns regarding the safety of providing bacteria to this population even though the bacteria are thought to be beneficial. The people who urge caution in the use of probiotics say so due to a few reports of sepsis after the introduction of probiotics with the organism that the patient was provided or with a different species that was could be traced to a contaminated product. As noted in an article on CBC recently these products fall under the category of a nutritional product rather than a medication with Health Canada and therefore are not subject to the same rigorous quality control standards as other comparable medications would be.
Others while recognizing the potential for contamination and sepsis would argue that the risk is low compared to the benefit provided to the infants overall and therefore claim benefits outweigh risks.
Manipulating Breastmilk in a Double Bling RCT
Given the above concerns regarding administration of these products to neonates I was excited to see the randomized double blinded study by Benor S et al; Probiotic supplementation in mothers of very low birth weight infants. This study enrolled mother and infant pairs within 72 hours after birth to commence on maternal treatment with Lactobacillus acidodphilus and Bifidobatera lactis versus placebo until discharge. The rationale for giving probiotics to lactating mothers was based on a previous study showing less atopic dermatitis in the offspring of mothers who took such treatment while breastfeeding and in a study of breast milk demonstrating lower levels of the inflammatory cytokine transforming growth factor beta (TNF-B). Less inflammation might equate to less NEC.
The primary outcome was Bell Stage II NEC and the investigators required 90 mothers in each arm to show a difference in the incidence of NEC based on previous work in their centre. All included pairs needed to be providing >50% EBM in order to minimize any effect from formula. The overall incidence of NEC at the completion of the study was 27% in the placebo group vs 12% probiotic group and for NEC II 18% vs 4% in those treated with probiotics. The rates of NEC were quite high compared to what we typically see and the authors noted that even for their site (for uncertain reasons) there was a higher rate than they expected. Neither of the rates of NEC were statistically different (both reached p=0.15 levels) but there was a significant issue with this study.
The total recruitment was 25 in the probiotic and 33 in the control arm. This was a far cry from the estimated 90 needed per side. The reason for this goes back to the start of this blog entry. The study needed to be stopped due to poor enrolment. Why so low? The majority of mothers approached for this study did not want to risk not getting probiotics so they opted to simply take them due to the perceived health benefits that as adults they already believe exist. Sadly I think this problem would resurface in many places if the study was replicated. This loss of equipoise by the families will make obtaining consent for such studies very difficult and we may not get a satisfactory answer.
Interestingly the authors of this study also measured TNF-B and found a strong trend towards lower levels in the breast milk of the probiotic supplemented group matching the trend towards less NEC.
I sincerely hope that another study such as this can be done without such issues in recruitment as the strategy would address the issue of not providing the bacteria directly to the neonate while still potentially reaping the benefits of less NEC. For now we will have to wait and see.