
by All Things Neonatal | Mar 8, 2017 | Breastmilk
The rise of donor milk banks and depots in recent years has been a welcome addition to the care of preterm infants. We have known for many years that “breast is best” and advocate for mother’s own milk whenever possible. When this is not possible we previously turned to formula but with the availability of pooled pasteurized donor milk many hospitals have focused on expanding the indications for use. Through personal communications in Canada we are a bit all over the map in terms of indications with some centres restricting use based on birth weight while others taking into account, gestational age as the main criteria. With respect to duration some centres use 2 weeks, others 4 and then others until a gestational age is reached which may mean up to 10 weeks of use for a baby born in that centre at 24 weeks. While variation exists it is hard to find anyone who would suggest this is a bad thing to provide.
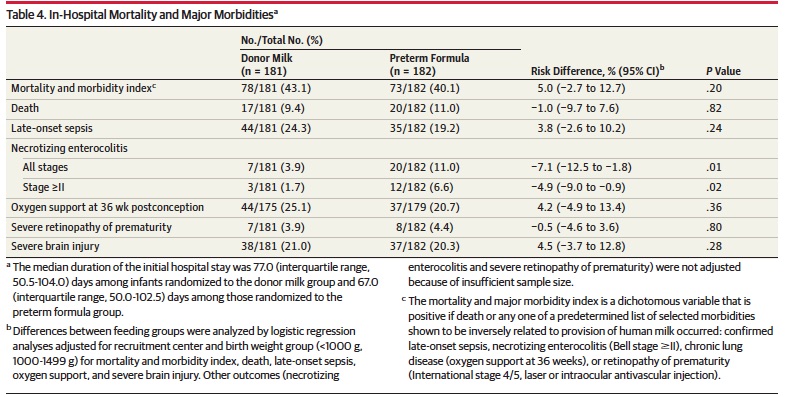
The main reason for pushing expansion of programs is the strong evidence that avoidance of bovine milk is associated with a reduction in the risk of NEC. Many studies have been done in this regard and the Cochrane systematic review concluded that formula increased the risk of necrotising enterocolitis: typical risk ratio 2.77 (95% CI 1.40 to 5.46); risk difference 0.04 (95% CI 0.02 to 0.07).
While donor milk is a wonderful nutritional product for sure it does have one issue which is a lower protein content than mother’s own milk and as such dieticians will commonly increase the protein content from 0.9 g/dL to 1.2 g/dL by adding powder or more recently liquid protein supplements. One might expect then that doing so would provide a reduction is NEC, and an optimal source of nutrition for the growing preterm brain. Avoidance of NEC should reduce the risk of adverse neurodevelopmental outcome as the two have been linked before.
Enter the DOMINO Study
This Ontario, Canada based study utilized four NICUs to provide in a randomized fashion either donor human milk or formula with matching protein and caloric densities to 363 infants (181 donor milk, 182 formula). All infants were preferentially fed mother’s own milk but supplemented with donor or formula if unavailable and planned to use one or the other for up to 90 days or discharge whichever came first. The exposure to donor milk was quite long in comparison to our own units practice (1 month duration if born at < 1500g) . The median number of days for donor milk was 65 (IQR, 41-90). A significant risk to the results would be if there was a difference in amounts of mother’s own milk provided between the two groups but there was none. Exclusive feeding of mother’s own milk occurred in the Donor milk group (28.2%) and formula group (26.9%) respectively. Among infants requiring a supplement, there was no statistically significant difference between the donor milk and formula groups in the proportion of total enteral feeds for each infant consumed as mother’s milk (58.4% [IQR, 13.6%-96.0%] vs 63.3% [IQR, 9.6%-97.2%], respectively, P = .96).
Short term but not long term gains
Curiously (at least to me) I would have expected differences in some of the morbidities other than NEC but such was not the case. 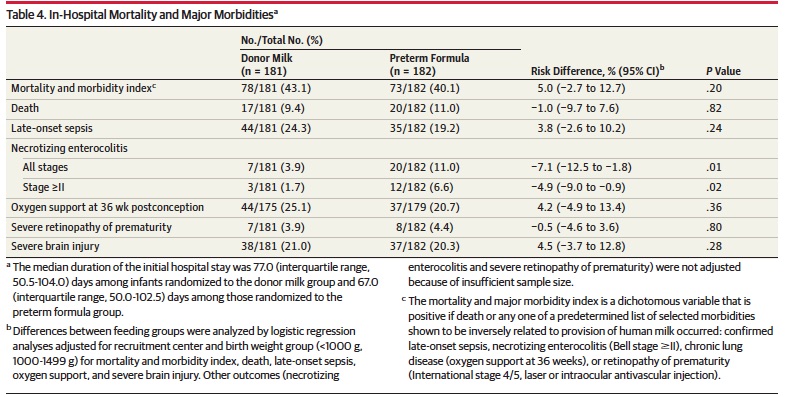
The strength of using human milk though can not be understated as any reduction in NEC is an extremely important outcome regardless of whether long term neurodevelopment is affected positively or not.
in terms of the latter outcome no difference was observed between the two groups. The Bayley III findings were quite similar at 18 months which on the surface may cause everyone’s shoulders to sag as the benefit everyone hoped for did not transpire. Additionally, linear growth, head circumference and weight gain were not different between groups. This may simply reflect that protein and caloric intakes were indeed matched between groups whereas in the past, the lack of protein fortification led to delays in growth in the donor milk groups.
At the risk of sounding like the end of a Cochrane review I am not sure this is the final word on donor milk and outcome. Larger studies may be needed to get at the real truth. This was not a pure sample of donor milk vs formula as a significant percentage (over 20% in both groups) received purely mother’s own milk. Furthermore, in those that received supplements there was still a significant percentage that received some of mother’s own milk. The authors suggest that a larger sample size would unlikely have detected a difference and that may be the case but is it so due to where the study was done. What if the study were done in a centre with a very low rate of breastfeeding? I am concerned that the lack of response in outcome may reflect a dilution of the impact of the strategy by having such a successful rate of providing mother’s own milk.
All Is Not Lost
Using a glass is half full view, I think it is worth pointing out that this study should also provide some comfort for those centres that use formula as a supplement. Clearly the higher rate of NEC is not comforting to anyone but for those who survive to discharge the neurodevelopmental outcome is promising. Formula in some circles has taken on a view as almost a toxic substance but I often remind residents and fellows that while we prefer breast milk, formula has been used in NICUs for decades and not every patient who receives it will develop NEC. Yes it is a risk factor for NEC and when you don’t have an alternative it is an acceptable form of nutrition to use. What I think may be lost in the DOMINO study is that if you are a centre that uses formula as there is no access to DBM this should help provide reassurance to the families you care for. All is not lost after the DOMINO study. Every cloud has a silver lining and fear not this will not be the last study to test this hypothesis. At the moment it is just the best we have and this is not the last we will hear on this topic.

by All Things Neonatal | Dec 15, 2016 | Breastmilk, Uncategorized
Producing milk for your newborn and perhaps even more so when you have had a very preterm infant with all the added stress is not easy. The benefits of human milk have been documented many times over for preterm infants. In a cochrane review from 2014 use of donor human milk instead of formula was associated with a reduction in necrotizing enterocolitis. More recently similar reductions have been seen in retinopathy of prematurity. Interestingly with respect to the latter it would appear that any amount of breast milk leads to a reduction in ROP. Knowing this finding we should celebrate every millilitre of milk that a mother brings to the bedside and support them when it does not flow as easily as they wish. While it would be wonderful for all mothers to supply enough for their infant and even more so that excess could be donated for those who can’t themselves we know this not to be the case. What we can do is minimize stress around the issue by informing parents that every drop counts and to celebrate it as such!
Why Is Breast Milk So Protective
Whether the outcome is necrotizing enterocolitis or ROP the common pathway is one of inflammation. Mother’s own milk contains many anti-inflammatory properties and has been demonstrated to be superior to formula in that regard by Friel and no difference exists between preterm and term versions. Aside from the anti-inflammatory protection there may be other factors at work such as constituents of milk like lactoferrin that may have a protective effect as well although a recent trial would not be supportive of this claim.
Could Mother’s Own Milk Have a Dose Response Effect in Reducing The Risk of BPD?
This is what is being proposed by a study published in early November entitled Influence of own mother’s milk on bronchopulmonary dysplasia and costs. What is special about this study and is the reason I chose to write this post is that the study is unusual in that it didn’t look at the effect of an exclusive human milk diet but rather attempted to isolate the role of mother’s own milk as it pertains to BPD. Patients in this trial were enrolled prospectively in a non randomized fashion with the key difference being the quantity of mothers own milk consumed in terms of a percentage of oral intake. Although donor breast milk existed in this unit, the patients included in this particular cohort only received mother’s own milk versus formula. All told, 254 infants were enrolled in the study. As with many studies looking at risks for BPD the usual culprits were found with male sex being a risk along with smaller and less mature babies and receipt of more fluid in the first 7 days of age. What also came up and turned out after adjusting for other risk factors to be significant as well in terms of contribution was the percentage of mother’s own milk received in the diet.
Every ↑ of 10% = reduction in risk of BPD at 36 weeks PMA by 9.5%
That is a really big effect! Now what about a reduction in costs due to milk? That was difficult to show an independent difference but consider this. Each case of BPD had an additional cost in the US health care system of $41929!
What Lesson Can be Learned Here?
Donor breast milk programs are a very important addition to the toolkit in the NICU. Minimizing the reliance on formula for our infants particularly those below 1500g has reaped many benefits as mentioned above. The availability of such sources though should not deter us from supporting the mothers of these infants in the NICU from striving to produce as much as they can for their infants. Every drop counts! A mother for example who produces only 20% of the needed volume of milk from birth to 36 weeks corrected age may reduce the risk of her baby developing BPD by almost 20%. That number is astounding in terms of effect size. What it also means is that every drop should be celebrated and every mother congratulated for producing what they can. We should encourage more production but rejoice in every 10% milestone.
What it also means in terms of cost is that the provision of lactation consultants in the NICU may be worth their weight in gold. I don’t know what someone performing such services earns in different institutions but if you could avoid two cases of BPD a year in the US I would suspect that nearly $84000 in cost savings would go a long way towards paying for such extra support.
Lastly, it is worth noting that with the NICU environment being as busy as it is sometimes the question “are you planning on breastfeeding?” may be missed. As teams we should not assume that the question was discussed on admission. We need to ask with intention whether a mother is planning on breastfeeding and take the time if the answer is “no” to discuss why it may be worth reconsidering. Results like these are worth the extra effort!

by All Things Neonatal | Mar 5, 2016 | Breastfeeding, Breastmilk, Uncategorized
I woke up this morning and as I do everyday, scanned the media outlets for news that would be of interest to you the reader. One such article today was about how breast milk may give babies a metabolic boost due to micro RNA present in the milk. This got me thinking about how natural a thing this breast milk is and how substances within interact with the baby receiving it. After that point I recalled writing about a challenge to the statement that breast milk is natural and thought you might like to see what I considered to be an outrageous piece of journalism from last year.
The premise of the article is that by reinforcing that breastfeeding is natural we may hamper initiatives to increase vaccination in many parts of the world and in particular North America I would think. The idea here is that if we firmly entrench in women’s heads that natural is better then this will strengthen the conviction that we should not vaccinate with these “man made” unnatural vaccines. I am sorry to be dramatic about this but I think the argument is ridiculous and in fact dangerous.
The Definition of Natural
“existing in nature and not made or caused by people : coming from nature”
From the Mirriam Webster dictionary
Breastfeeding satisfies this definition pure and simple and there is nothing that anyone should say to suggest otherwise no matter what the motive is. The shift from formula to breastfeeding has been predicated on this notion and a plethora of literature on the subject demonstrating reductions in such things as infections of many kinds, diarrhoea, atopic disease in the first year of life as examples. In my world of premature infants additional reductions in NEC, bloody stools, have been seen and more recently in some cases improved neurodevelopmental outcomes.
In this case of irresponsible journalism a better approach if you were wanting to use the natural argument with respect to vaccines is to promote just that.
Vaccines are Natural
Someone will no doubt challenge me on this point as it would be a fair comment to say that there are artificial substances added to vaccines but there is no question the organisms that we vaccinate against are natural.
Think about this for a moment. All of the vaccines out there are meant to protect us against organisms that exists in NATURE. These are all bacteria or viruses that have likely existed on this planet of ours for millions of years. They are found everywhere and in many cases what we are doing when we give such vaccines are providing parts of or weakened versions of these natural organisms in order for us the human to mount a protective response.
This protective response is NATURAL. If we didn’t vaccinate and came across the fully virulent pathogen in NATURE our bodies would do exactly what they do when a vaccine is given to us. Our immune system would mount a response to the organism and start producing protective antibodies. Unfortunately in many cases this will be too little too late as the bacteria or virus will cause it’s damage before we have a chance to rid ourselves of this natural organism.
This is the basis of vaccination. Allow our bodies a chance to have protection against an organism that we haven’t been exposed to yet so that when it comes we have a legion of antibodies just waiting to attach this natural organism.
CNN Didn’t Get It Right

In the article which is based on a paper entitled the Unintended Consequences of Invoking the “Natural” in Breastfeeding Promotion by Jessica Martucci & Anne Barnhill the authors admit that the number of families that this actually would impact is small. the question then is why publish this at all. Steering families away from thinking that breastfeeding is natural is wrong. Plain and simple.
If the goal is to improve vaccination rates, focus on informing the public about how NATURAL vaccinations actually are and don’t drag breastfeeding down in order to achieve such goals. As a someone who writes themselves I am well aware of how personal biases creep into everything we write. I am aware of the irony of that statement since it is clear what side of the argument I sit on. While I peruse CNN myself almost daily I think the editors either missed the larger message in this piece or perhaps felt the same way. A disclosure that “the opinions of the author do not necessarily represent those of the network” does not cut it for what I would consider responsible journalism in this case.

by All Things Neonatal | Dec 2, 2015 | Breastmilk, donor milk, preemie, Uncategorized
What follows is a news release from today that begins a new chapter in supporting preemies here in Manitoba. There are far too many people to thank who made this possible but to all I say THANK YOU!
New Breast Milk Drop Site at the Birth Centre Benefits Premature and Sick Infants
DECEMBER 2, 2015 (WINNIPEG, MB) – The Winnipeg Regional Health Authority (WRHA) announced today a milk drop site is being established at the Birth Centre (603 St. Mary’s Road) in Winnipeg. Minister Blady announced the collaboration between Women’s Health Clinic and the NorthernStar Mother’s Milk Bank.
Registered donations of breast milk will be accepted by the Birth Centre in Winnipeg and transported for pasteurization at NorthernStar’s lab in Calgary. The pasteurized human milk from donors will be used to help premature and sick babies in neonatal intensive care units in hospitals, and in the community, across Canada.
“There can be a number of reasons why a mother may not be able to provide breast milk for her baby,” said Health Minister Sharon Blady. “This new Milk Drop site will help families ensure premature and sick babies get the best possible start in life by providing pasteurized donor human milk an infant needs to not only survive, but thrive.”
The minister noted that establishing a human milk drop supports recommendations made in the Manitoba Breastfeeding Strategy, released in 2013.
The WRHA purchased a freezer for the milk drop with funds provided by the Winnipeg-based Siobhan Richardson Foundation. The Birth Centre will house the freezer and ensure the safe handling and storage of donated human milk before it is shipped to Calgary for processing.
“My thanks and appreciation goes out to the Siobhan Richardson Foundation for supporting new moms as well as our tiniest patients,” said Dana Erickson, Chief Operating Officer, Health Sciences Centre and WRHA executive responsible for child health and women’s health. “This milk drop initiative in Manitoba is a reality because of their vision and generosity along with the commitment and hard work of our excellent health care team.”
Studies have shown premature infants who receive the nutrients of pasteurized human milk from donors, when their mother’s own milk is not available, have fewer long-term health needs. The use of pasteurized donor human milk instead of formula can reduce the risk of serious health complications in pre-term infants. Having a dedicated milk supply for these babies can save lives.
“Several health outcomes for preterm infants are improved when pasteurized donor human milk, rather than formula, is used in these high risk infants,” said Dr. Michael Narvey, section head of neonatology for the Winnipeg Regional Health Authority. “Pasteurized donor human milk has been proven to reduce the chances of an infant developing a serious condition of the bowel which can lead to lifelong and serious health consequences. Babies weighing less than 1500 grams are significantly less likely to develop this serious condition when they are given pasteurized human milk from donors as opposed to formula.”
Starting January 4, 2016, the Birth Centre will accept breast milk from donors approved by NorthernStar Mothers Milk Bank (formerly the Calgary Mothers Milk Bank). Women must first contact the NorthernStar Mothers Milk Bank to be screened prior to dropping off their donation at the Birth Centre. Women will then need to have further screening including blood tests by their primary care provider to confirm if they qualify as a donor. These donations will be sent to the milk bank’s lab in Calgary where the donor milk is tested, pasteurized, and then prioritized for premature and sick infants.
“We are excited to see Manitoba’s first Milk Drop opening in Winnipeg,” said Janette Festival, Executive Director, NorthernStar Mothers Milk Bank. “This Milk Drop is a testament to cooperation of multiple groups who believe in the medical power of donor human milk for babies in need. We hope this new ‘drop’ will encourage women in the Winnipeg area to consider becoming a milk donor.”
Women’s Health Clinic operates the Birth Centre facility and community programming, and will be collecting the donations and shipping them to the milk bank for testing and pasteurizing.
“Women and families come to the Birth Centre every day for a range of maternal health and wellness services, making it an ideal location for the new Milk Drop site,” said Joan Dawkins, Executive Director of Women’s Health Clinic. “Women who are interested in donating can get the process underway now by contacting NorthernStar Mothers Milk Bank.”
To donate, mothers can contact the milk bank at 1-403-475-6455 or visit NorthernStarmilkbank.ca.
For more information contact:
Melissa Hoft
Winnipeg Regional Health Authority
P: (204) 926-7180 C: (204) 299-0152 E: [email protected]
Amy Tuckett
Women’s Health Clinic (Birth Centre)
P: (204) 947-2422 ext. 147 C: (204) 996-6289 E: [email protected]
Janette Festival
NorthernStar Mothers Milk Bank
P: (403) 475-6455 E: [email protected]

by All Things Neonatal | Jul 4, 2015 | Breastmilk, LGBT
There is the potential for a very significant issue to arise in the NICU environment in the coming years. As I was preparing the last blog piece following the decision by SCOTUS to allow same-sex marriage in all 50 states I began to think about the so-called ripple effect. In other words, now that the law has been changed, what impacts could this have that might have been unforeseen. The first thought that crept into my mind was that as male same-sex parents they would read the same literature that promotes breast milk feeding in the NICU and no doubt want the best for their infant in the NICU or for that matter any baby. In many NICUs however there are weight or gestational age restrictions indicating who will receive donor breast milk if the mother is not able or not willing to produce her own. In our unit for example we given DBM to all babies currently under 1250g and those recovering from NEC or other bowel surgery. Might men in a same-sex marriage who have adopted a child or used a surrogate who is not willing to breastfeed demand the same?
In looking into this I came across a very strange story from 2013 in which a nurse in the UK offered to “rent her breasts” to gay parents. The story at the time caused a fairly big stir as it raised a number of questions as to safety and the morality of it all. In some ways it was ahead of its time as there have been a number of articles recently addressing the very issue of safety of milk (will be addressed further in the article obtained outside of HMBANA approved breast milk banks.
As same-sex couples increase and many then choose to have children of their own to raise what demands will be made of access to breast milk? There is no question “breast is best” and I have either written or posted to Facebook many articles suggesting decreased incidence of allergy, necrotizing enterocolitis, improvements in the microbiome and many other benefits as well. What do we do in the situation of the same-sex family who declares that they want to provide breast milk to their infant in hospital as it is the best source of nutrition for their infant. If we say for example that their 2 kg, 34 week infant is too big to qualify for DBM is this fair given that they have no option for producing their own milk in the setting of male same-sex partners? Could we as health care providers be labelled as discriminating?
One option is to allow such parents to bring in their own milk but then where do they source it from? Milk purchased online or from the community may be contaminated with bacteria, viruses or contain some cow’s milk as some recent publications have demonstrated. Can we knowingly allow families to bring such milk into the hospital to feed their infant? Perhaps, but only if we have medical legal safeguards in place that protect the hospital from knowingly allowing patients to bring in milk which could be contaminated. Waivers of liability would need to be in place in each hospital permitting such sourcing of milk. If however we strongly discourage such practice will we direct them to the milk bank supplying our local hospital. Herein lies the challenge though. If availability of volume was not an issue, we could provide to all infants in the unit but the reality is there is simply not enough to go around. Furthermore, the larger the infant, the more donor milk they utilize and the more depleted the supply becomes for those of our smallest infants who are most in need of avoiding formula. Finally, who should pay for this milk if the family cannot produce any as in this situation. This is not a case of a mother who could produce but chooses not to but rather a family who is desperate to use what they have read is best but physically is incapable of producing. The same of course could be said for those women who try and cannot or due to prior surgery are unable to produce milk. I believe this is an issue that will come up across the US and Canada and I will be interested to see how it plays out and what role Bioethics may play in helping to resolve some of these questions.
This will be a slippery slope. If male same-sex parents are provided with free access to donor milk I don’t see how donor milk will not be made available to all families who cannot provide their own. Why would the male parents who biologically be unable to provide milk be given this “liquid gold” while other mothers who are pumping round the clock, taking domperidone and seeing a lactation consultant and getting only drops be denied as their newborn is 1600g and above the weight cutoff. I hope you can see the issue of equity popping up in this discussion.
Finally why not allow those parents who are male same-sex partners to simply pay for the milk they need if they don’t qualify for “free” milk under a unit’s program? Sadly the issue then becomes one of equity again. Do we want to care for infants in an environment where the wealthy who can afford to pay for the donor milk from an HMBANA milk bank get it and the poor are only offered formula? I have to admit I realize there are health care systems where this is the case but in Canada where we have a socialized medical system this kind of two tiered system would cause many to become nauseated.
I fear that this issue will come up as the number of people marrying and choosing to have children in same-sex relationships increases. If it leads to a 100% human milk diet for infants in the NICU I would say that is a good thing but I think the road like Winnipeg will be paved with many potholes that we will have to do our best to navigate around.

by All Things Neonatal | Jun 6, 2015 | Breastfeeding, Breastmilk, newborn
Nineteen seventy two was notable for many things aside from the year of my birth. Canada defeated the Soviets in the summer series, the Watergate scandal took down a Presidency, The GodFather was released and for the purposes of this post breastfeeding rates in the US reached an all time low of 22%. For an excellent review of the history of breastfeeding the article by AL Wright is excellent.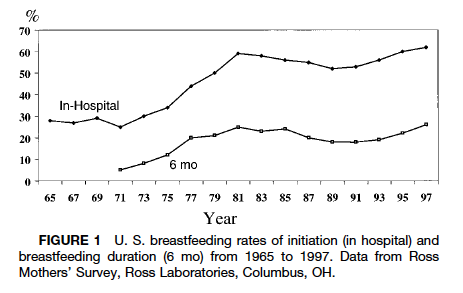
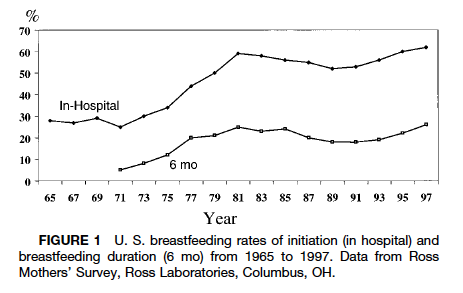
Rates of breastfeeding began a steady decline in the 1960s as more and more women entered the workforce and seemingly had to choose between employment and breastfeeding. This was a time when it was not seen as being acceptable to breastfeed in public (although that is not the case in many places still to this day) and the workplace was not as conducive to supporting women as in current times (think onsite daycares). Add to this that the 1970s also saw a backlash of sorts in the appeal of breastfeeding due to science “perfecting” a better source of nutrition in formula and we had the low rates that we did. In fact through discussions with parents from that generation, mother’s who chose to breastfeed may have been viewed by some as being silly for not using something like formula that could let the whole family in on the experience. Mom, Dad, kids and grandparents could all take part in the wonderful act of feeding. Why be so selfish?
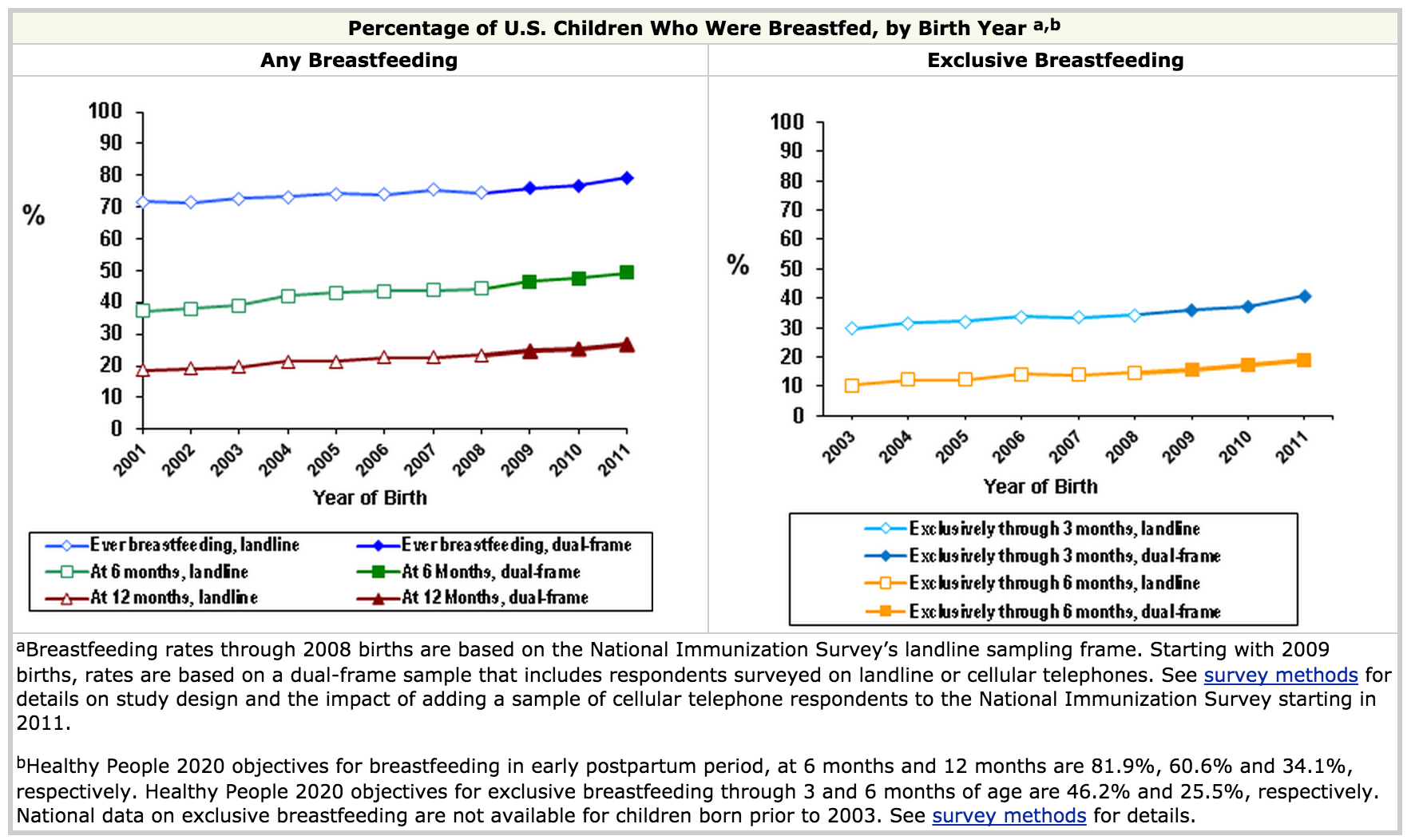
Following this period as research began to demonstrate improved outcomes with breastfeeding including reductions in atopic disease, less hospital admissions and more recently positive impacts on intelligence and your microbiome the trend reversed. In fact, as the above graph demonstrates, rates approximating 70% were reached by the late 1990s. Since that time the CDC has shown that initiation rates have continued to rise and currently are at the highest documented levels in history.
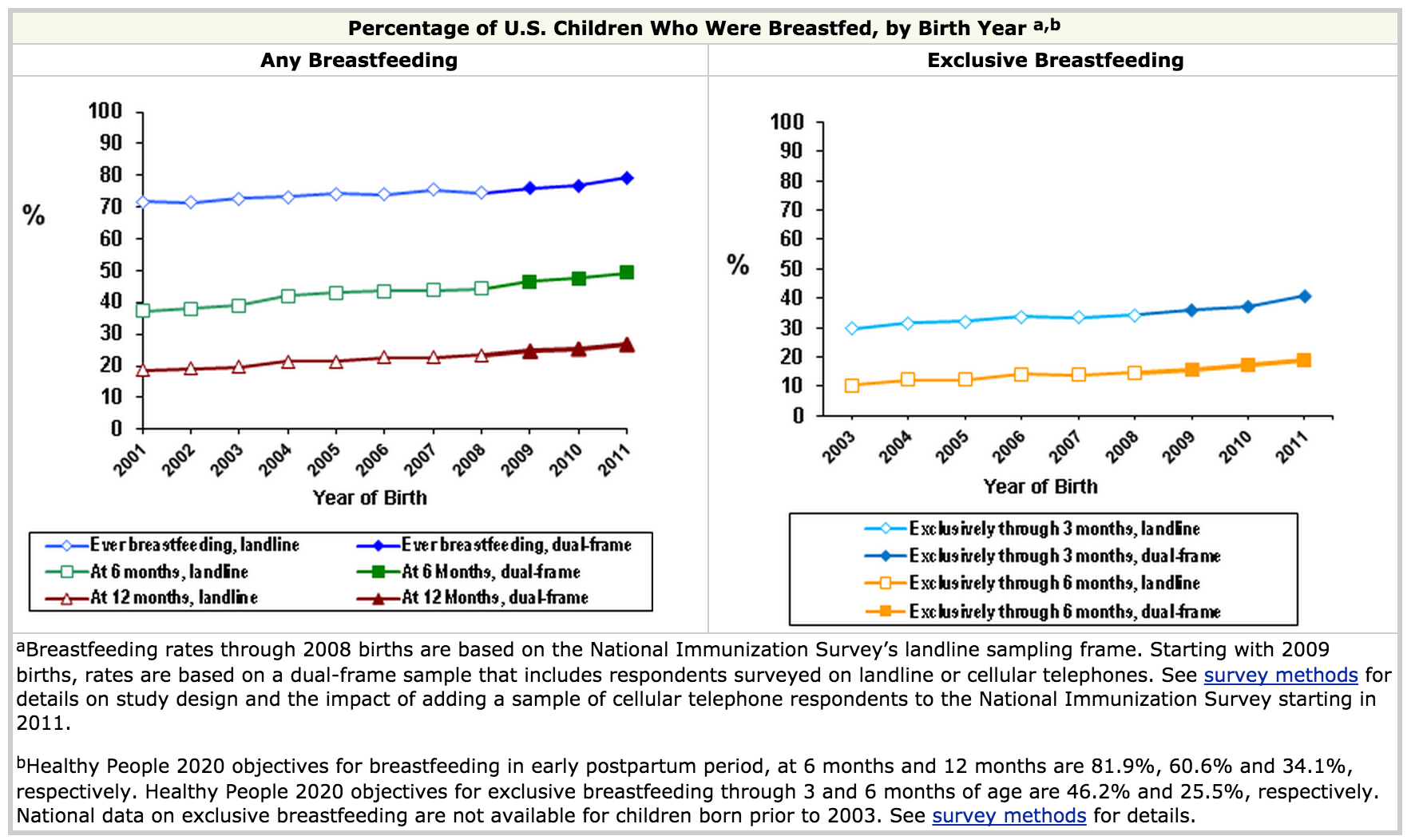
Looking at the CDC data though reveals some very important information. While the rates of any breastfeeding reach 80%, the rates at 6 months hover around 50%. This means that a significant portion of US women are using some formula when they come home and from the graph on the right about 35% by three months are exclusively breastfeeding. This number is far short of the goal the WHO has set to encourage exclusive breastfeeding for the first 6 months however it is a remarkable achievement for infant health.
http://www.who.int/topics/breastfeeding/en/
A recent trend on social media and print media has been the Brelfie. As you may know, this involves taking a picture of yourself breastfeeding your baby and posting it in one forum or another. This has been popularized by many celebrities and made it’s way onto the cover of Elle magazine this month.
 So called Lactavists have been overjoyed to see such public acceptance and promotion of breastfeeding. As a Neonatologist I am delighted to see such high rates of breastfeeding and with it the beneficial effects that it brings.
So called Lactavists have been overjoyed to see such public acceptance and promotion of breastfeeding. As a Neonatologist I am delighted to see such high rates of breastfeeding and with it the beneficial effects that it brings.
Curiously, though all of this attention and promotion of breastfeeding has created a culture that is now being called bressure. This is defined as pressure to breastfeed and was the subject of a recent survey by Channel Mum in the UK. The highlights of the survey that went out to 2,075 mums showed:
– 16 per cent of bottle-feeding mums have been on the receiving end of cruel comments from other mothers they know
– one in 20 being attacked on social media
– 69 per cent of bottle-feeding mums said they had been judged negatively
– 41 per cent made to feel they have ‘failed as a mum and failed their child’ by not breastfeeding
– 15 per cent of mums have even lied to cover up their bottle-feeding and appear to be ‘better’ mums.
This so called bressure has led to a public campaign to increase awareness of the harassment that some mothers feel which involves taking selfies with cards having one word describing what breastfeeding meant for them. A video from Channel Mum can be seen here
Channel Mum Video Response to Brelfies
While I am all for breastfeeding, I find it peculiar that the experience that breastfeeding mothers (all 22% of them) had in 1972 is now being felt by a larger percentage in 2015 who are bottle feeding. It is unfortunate that assumptions are being made of many of these women who put a bottle in the mouths of their infants. How many times does one conclude that the mother simply chose not to breastfeed because they were worried about the way their breasts would be affected cosmetically or that they simply chose to go back to work and breastfeeding would just get in the way. I suspect in most cases the truth is much different. Many of these mothers have tried to breastfeed but couldn’t produce enough. Others may have suffered from cracked nipples, mastitis, abscesses or due to prior surgery were unable to produce milk. Many such mothers have agonized over their “failure” to do something that they hear “everyone can do”. While they are told it takes some work for many that is a huge understatement. Is it not bad enough that these women have suffered the feeling of failure? To be looked at or spoken to in a disapproving way does nothing to support them. Add to this that by 3 months of age at least in the US 65% of mothers are providing some formula and it seems silly to take the “high and mighty” approach in the first couple of months and assume the worst of these women. Many of the “breastfeeders” will soon enough join the ranks of those using some formula.
Maybe the better option is to try and help. Many of the above problems whether it be producing enough quantity or pain related to breastfeeding can be addressed through tips on technique. While I am not an expert in this, hospitals would do well to increase staffing of on site lactation consultants to help mothers who wish to breastfeed get off on the right foot so to speak. A larger working force of midwives in North America in particular could certainly provide help in this regard. What I can say is that if a woman suffers a bad experience with breastfeeding in their first pregnancy the likelihood they will try again the next time is lower especially if we as a society make them feel like a failure.
Yes we need to promote breastfeeding and we should do what we can to follow the WHO recommendations and minimize the use of formula when possible. While bressure may have been intended to yield something good we need to be sensitive. Perhaps a better strategy next time a friend says they are going to use formula is to ask if they are having trouble with breastfeeding and if they need some help. Not having the discussion will ensure that nothing changes and a chance to do something will be lost due to misdirected bressure.








 So called Lactavists have been overjoyed to see such public acceptance and promotion of breastfeeding. As a Neonatologist I am delighted to see such high rates of breastfeeding and with it the beneficial effects that it brings.
So called Lactavists have been overjoyed to see such public acceptance and promotion of breastfeeding. As a Neonatologist I am delighted to see such high rates of breastfeeding and with it the beneficial effects that it brings.