In 2015 the Pediatric Endocrine Society (PES) published new recommendations for defining and managing hypoglycaemia in the newborn. A colleague of mine and I discussed the changes and came to the conclusion that the changes suggested were reasonable with some “tweaks”. The PES suggested a change from 2.6 mmol/L (47 mg/dL) at 48 hours of age as a minimum goal glucose to 3.3 mmol/L (60 mg/dL) as the big change in approach. The arguments for this change was largely based on data from normal preterm and term infants achieving the higher levels by 48-72 hours and some neuroendocrine data suggesting physiologically, the body would respond with counter regulatory hormones below 3.3 mmol/L.
As it turned out, we were “early adopters” as we learned in the coming year that no other centre in Canada had paid much attention to the recommendations. The inertia to change was likely centred around a few main arguments.
1. How compelling was the data really that a target of 2.6 and above was a bad idea?
2. Fear! Would using a higher threshold result in many “well newborns” being admitted to NICU for treatment when they were really just experiencing a prolonged period of transitional hypoglycaemia.
3. If its not broken don’t fix it. In other word, people were resistant to change itself after everyone was finally accustomed to algorithms for treatment of hypoglcyemia in their own centres.
What effect did it actually have?
My colleagues along with one of our residents decided to do a before and after retrospective comparison to answer a few questions since we embraced this change. Their answers to what effect the change brought about are interesting and therefore at least a in my opinion worth sharing. If any of you are wondering what effect such change might have in your centre then read on!
Skovrlj R, Marks S and C. Rodd published Frequency and etiology of persistent neonatal hypoglycemia using the more stringent 2015 Pediatric Endocrine Society hypoglycemia guidelines. They had a total of 58 infants in the study with a primary outcome being the number of endocrine consults before and after the change in practice.  Not surprisingly as the graph demonstrates the number went up.
Not surprisingly as the graph demonstrates the number went up.
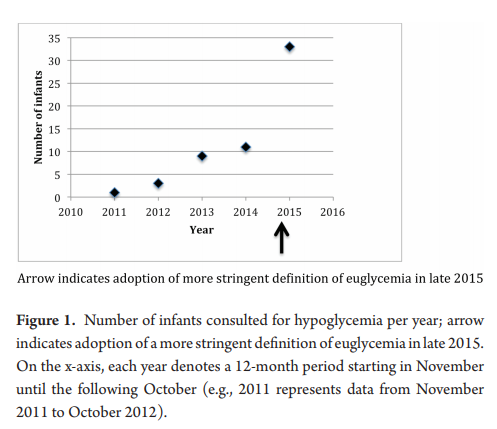
Once the protocol was in place we went from arbitrary consults to mandatory so these results are not surprising. What is surprising though is that the median critical plasma glucose was 2.2 mmol/L, with no significant difference pre or post (2.0 mmol/L pre versus 2.6 mmol/L post, P=0.4) Ninety percent of the infants who were hypoglycemic beyond 72 hours of age were so in the first 72 hours. Of these infants, 90% were diagnosed with hyperinsulinemia. What this tells us is that those who are going to go on to have persistent hypoglycemia will demonstrate similar blood sugars whether you use the cutoff of 2.6 or 3.3 mmol/L. You will just catch more that present a little later using the higher thresholds. How would these kids do at home if discharged with true hyperinsulinemia that wasn’t treated? I can only speculate but that can’t be good for the brain…
Now comes the really interesting part!
Of the total infants in the study, thirteen infants or 40% had plasma glucose values of 2.6 to 3.2 mmol/L at the time of consultation after November 2015. Think about that for a moment. None of these infants would have been identified using the old protocol. Nine of these infants went on to require treatment with diazoxide for persistent hyperinsulinemia. All of these infants would have been missed using the old protocol. You might ask at this point “what about the admission rate?”. Curiously an internal audit of our admission rates for hypoglycemia during this period identified a decline in our admission rates. Concurrent with this change we also rolled out the use of dextrose gels so the reduction may have been due to that as one would have expected admission rates to rise otherwise. The other thing you might ask is whether in the end we did the right thing as who says that a plasma blood glucose threshold of 3.3 mmol/L is better than using the tried and true 2.6 mmol/L cutoff?
While I don’t have a definitive answer to give you to that last question, I can leave you with something provocative to chew on. In the sugar babies study the goal glucose threshold for the first 7 days of life was 2.6 mmol/L. This cohort has been followed up and I have written about these studies before in Dextrose gel for hypoglycemia. Safe in the long run? One of the curious findings in this study was in the following table. 
Although the majority of the babies in the study had only mild neurosensory impairment detectable using sophisticated testing the question is why should so many have had anything at all? I have often wondered whether the goal of keeping the blood sugar above 2.6 mmol/L as opposed to a higher level of say 3.3 mmol/L may be at play. Time will tell if we begin to see centres adopt the higher thresholds and then follow these children up. I don’t know about you but a child with a blood sugar of 2.7 mmol/L at 5 or 6 days of age would raise my eyebrow. These levels that we have used for some time seem to make sense in the first few days but for discharge something higher seems sensible.