
by All Things Neonatal | Aug 23, 2017 | donor milk, Neonatology, nutrition, preemie, Prematurity
Exclusive human milk (EHM) diets using either mother’s own milk or donor milk plus a human based human milk fortifier have been the subject of many papers over the last few years. Such papers have demonstrated reductions is such outcomes as NEC, length of stay, days of TPN and number of times feedings are held due to feeding intolerance to name just a few outcomes. There is little argument that a diet for a human child composed of human milk makes a great deal of sense. Although we have come to rely on bovine sources of both milk and fortifier when human milk is unavailable I am often reminded that bovine or cow’s milk is for baby cows.
Challenges with using an exclusive human milk diet.
While it makes intuitive sense to strive for an exclusive human milk diet, there are barriers to the same. Low rates of maternal breastfeeding coupled with limited or no exposure to donor breast milk programs are a clear impediment. Even if you have those first two issues minimized through excellent rates of breast milk provision, there remains the issue of whether one has access to a human based fortifier to achieve the “exclusive” human milk diet.
The “exclusive” approach is one that in the perfect world we would all strive for but in times of fiscal constraint there is no question that any and all programs will be questioned from a cost-benefit standpoint. The issue of cost has been addressed previously by Ganapathy et al in their paper Costs of Necrotizing Enterocolitis and Cost-Effectiveness of Exclusively Human Milk-Based Products in Feeding Extremely Premature Infants. The authors were able to demonstrate that choosing an exclusive human milk diet is cost effective in addition to the benefits observed clinically from such a diet. In Canada where direct costs are more difficult to visualize and a reduction in nursing staff per shift brings about the most direct savings, such an argument becomes more difficult to achieve.
Detractors from the EHM diet argue that we have been using bovine fortification from many years and the vast majority of infants regardless of gestational age have little challenge with it. Growth rates of 15-20 g/kg/d are achievable using such fortification so why would you need to treat all patients with an EHM diet?
A Rescue Approach
In our own centre we were faced with these exact questions and developed a rescue approach. The rescue was designed to identify those infants who seemed to have a clear intolerance to bovine fortifier as all of the patients we care for under 1250g receive either mother’s own or donor milk. The approach used was as follows:
A. < 27 weeks 0 days or < 1250 g
i. 2 episode of intolerance to HMF
ii. Continue for 2 weeks
This month we published our results from using this targeted rescue approach in Winnipeg, Human Based Human Milk Fortifier as Rescue Therapy in Very Low Birth Weight Infants Demonstrating Intolerance to Bovine Based Human Milk Fortifier with Dr. Sandhu being the primary author (who wrote this as a medical student with myself and others. We are thrilled to share our experience and describe the cases we have experienced in detail in the paper. Suffice to say though that we have identified value in such an approach and have now modified our current approach based on this experience to the following protocol for using human derived human milk fortifier in our centre to the current:
A. < 27 weeks 0 days or < 1250 g
i. 1 episode of intolerance to HMF
ii. Continue for 4 weeks
B. ≥ 27 week 0 days or ≥ 750g
i. 2 episodes of intolerance to HMF
ii. Continue for 4 weeks or to 32 weeks 0 days whichever comes sooner
We believe given our current contraints, this approach will reduce the risk of NEC, feeding intolerance and ultimately length of stay while being fiscally prudent in these challenging times. Given the interest at least in Canada with what we have been doing here in Winnipeg and with the publication of our results it seemed like the right time to share this with you. Whether this approach or one that is based on providing human based human milk fortifier to all infants <1250g is a matter of choice for each institution that chooses to use a product such as Prolacta. In no way is this meant to be a promotional piece but rather to provide an option for those centres that would like to use such products to offer an EHM diet but for a variety of reasons have opted not to provide it to all.

by All Things Neonatal | Aug 10, 2017 | newborn, preemie, Prematurity, resuscitation, ventilation
I know how to bag a baby. At least I think I do. Providing PPV with a bag-valve mask is something that you are taught in NRP and is likely one of the first skills you learned in the NICU. We are told to squeeze the bag at a rate of 40-60 breaths a minute. According to the Laerdal website, the volume of the preterm silicone bag that we typically use is 240 mL. Imagine then that you are wanting to ventilate a baby who is 1 kg. How much should you compress the bag if you wish to delivery 5 mL/kg. Five ml out of a 240 mL bag is not a lot of squeeze is it? Think about that the next time you find yourself squeezing one. You might then say but what about a t-piece resuscitator? A good choice option as well but how much volume are you delivering if you set the initial pressures at 20/5 for example? That would depend on the compliance of the lung of course. The greater the compliance the more volume would go in. Would it be 5 mL, 10 ml or even 2.5 mL based on the initial setting? Hard to say as it really depends on your seal and the compliance of the lung at the pressure you have chosen. If only we had a device that could deliver a preset volume just like on a ventilator with a volume guarantee setting!
Why is this holy grail so important?
It has been over 30 years since the importance of volutrauma was demonstrated in a rabbit model. Hernandez LA et al published Chest wall restriction limits high airway pressure-induced lung injury in young rabbits. The study used three models to demonstrate the impact of volume as opposed to pressure on injuring the lung of preterm rabbits. Group 1 were rabbit ventilated at pressures of 15/30/45 cm H2O for one hour, group 2 rabbits with a cast around their thorax to limit volume expansion and group 3 sets of excised lungs with no restriction to distension based on the applied pressures. As you might expect, limitation of over distension by the plaster cast led the greatest reduction in injury (measured as microvascular permeability) with the excised lungs being the worst. In doing this study the authors demonstrated the importance of over distension and made the case for controlling volume more than pressure when delivering breaths to avoid excessive tidal volume and resultant lung injury.
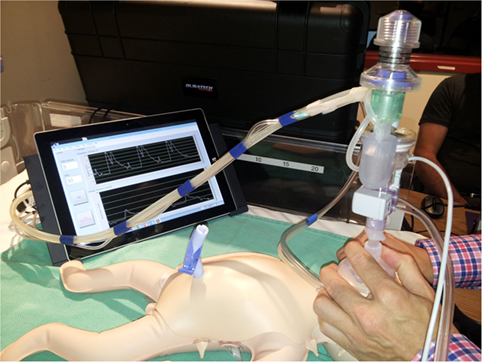
The “Next Step” Volume Ventilator BVM
Perhaps I am becoming a fan of the Edmonton group. In 2015 they published A Novel Prototype Neonatal Resuscitator That Controls Tidal Volume and Ventilation Rate: A Comparative Study of Mask Ventilation in a Newborn Manikin. The device is tablet based and as described, rather than setting a PIP to deliver a Vt, a rate is set along with a volume to be delivered with a peep in this case set at +5. 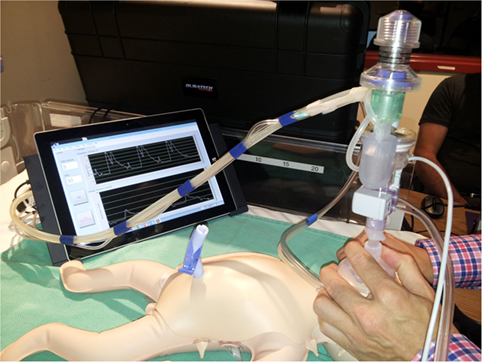 This study compared 5 different methods of delivering PPV to a 1 kg preterm manikin. The first was a standard self inflating bag, the next three different t-piece resuscitators and then the Next Step. For the first four the goal was to deliver a pressure of 20/5 at a rate of 40-60 breaths per minute. A test lung was connected to the manikin such that each device was used for a one minute period at three different levels of compliance (0.5 ml/cmH2O, 1.0 ml/cmH2O and then 2.0 ml/cm H2O representing increasing compliance. The goal of the study was to compare the methods in terms of delivering a volume of 5 mL to this 1 kg model lung. The order in which the devices were used was randomized for the 25 participants in the study who were all certified in NRP and included some Neonatologists.
This study compared 5 different methods of delivering PPV to a 1 kg preterm manikin. The first was a standard self inflating bag, the next three different t-piece resuscitators and then the Next Step. For the first four the goal was to deliver a pressure of 20/5 at a rate of 40-60 breaths per minute. A test lung was connected to the manikin such that each device was used for a one minute period at three different levels of compliance (0.5 ml/cmH2O, 1.0 ml/cmH2O and then 2.0 ml/cm H2O representing increasing compliance. The goal of the study was to compare the methods in terms of delivering a volume of 5 mL to this 1 kg model lung. The order in which the devices were used was randomized for the 25 participants in the study who were all certified in NRP and included some Neonatologists.
Some Concerning Findings
As I said at the beginning, we all like to think we know how to ventilate a newborn with BVM. The results though suggest that as compliance increases our ability to control how much volume we deliver to a lung based on a best guess for pressures needed is lacking. One caveat here is that the pressures set on the t-piece resucitators were unchanged during the 1 minute trials but then again how often during one minute would we change settings from a starting point of 20/5?
|
|
Vt (mL) |
|
|
0.5 mL/cmH20 |
1.0 mL/cmH20 |
2.0mL/cmH20 |
| Self inflating |
11.4 |
17.6 |
23.5 |
| Neo-Tee |
5.6 |
11.2 |
19.3 |
| Neopuff |
6.1 |
10 |
21.3 |
| Giraffe |
5.7 |
10.9 |
19.8 |
| Next Step |
3.7 |
4.9 |
4.5 |
Without putting in all the confidence intervals I can tell you that the Next Step was the tightest. What you notice immediately (or at least I did) was that no matter what the compliance, the self inflating bag delivers quite an excessive volume even in experienced hands regardless of compliance. At low compliance the t-piece resuscitators do an admirable job as 5-6 ml/kg of delivered Vt is reasonable but as compliance improves the volumes increase substantially. It is worth pointing out that at low compliance the Next Step was unable to deliver the prescribed Vt but knowing that if you had a baby who wasn’t responding to ventilation I would imagine you would then try a setting of 6 ml/kg to compensate much like you would increase the pressure on a typical device. How might these devices do in a 29 week infant for example with better compliance than say a 24 week infant? You can’t help but wonder how many babies are given minutes of excessive Vt after birth during PPV with the traditional pressure limited BVM setup and then down the road how many have BPD in part because of that exposure.
I wanted to share this piece as I think volume resuscitation will be the future. This is just a prototype or at least back then it was. Interestingly in terms of satisfaction of use, the Next Step was rated by the participants in the study as being the easiest and most comfortable to use of all the devices studied. Adding this finding to the accuracy of the delivered volume and I think we could have a winner.
by All Things Neonatal | Aug 2, 2017 | Neonatal, Neonatology, newborn, Pain in the Neonate, preemie
I would consider myself fairly open minded when it comes to care in the NICU. I wouldn’t call myself a maverick or careless but I certainly am open to new techniques or technologies that may offer a better level of care for the babies in our unit. When it comes to “non-Western” concepts though such as therapeutic touch, chiropractic manipulations of infants and acupuncture (needle or otherwise) I have generally been a skeptic. I have written about such topics before with the most popular post being Laser acupuncture for neonatal abstinence syndrome. My conclusion there was that I was not a fan of the strategy but perhaps I could be more open to non traditional therapies.
Magnetic Acupuncture
This would appear to be the newest and perhaps strangest (to me at least) approach to pain relief that I have seen. I do love name of this study; the MAGNIFIC trial consisted of a pilot study on the use of auricular magnetic acupuncture to alleviate pain in the NICU from heel lances. The study was published in Acta Paediatrica this month; Magnetic Non-Invasive Acupuncture for Infant Comfort (MAGNIFIC) – A single-blinded randomized controlled pilot trial. The goal here was to measure pain scores using the PIPP scoring system for pain in the neonate before during and after a painful experience (heel lance) in the NICU. Being a pilot study it was small with only 20 needed per arm based on the power calculation to detect a 20% difference in scores. The intervention used small magnets placed at specific locations on the ear of the infant at least two hours before the heel lance was to occur. Before I get into the results, the authors of the study provide references to explain how the therapy works. Looking at the references I have to admit I was not able to obtain complete papers but the evidence is generally it would appear from adult patients. The explanation has to do with the magnetic field increasing blood flow to the area the magnet is applied to and in addition another reference suggests that there are affects the orbitofrontal and limbic regions which then impacts neurohormonal responses as seen in functional MRI. The evidence to support this is I would have thought would be pretty sparse but I was surprised to find a literature review on the subject that looked at 42 studies on the topic. The finding was that 88% of the studies reported a therapeutic effect. The conclusion though of the review was that the quality of the included studies was a bit sketchy for the most part so was not able to find that this should be a recommended therapy.
So what were the results?
Despite my clear skepticism what this study did well was that aside from the magnets, the intervention was the same. Twenty one babies received the magnetic treatments vs 19 placebo. There was a difference in the gestational ages of the babies with the magnet treated infants being about two weeks older (35 vs 33 weeks). What difference that might in and of itself have on the PIPPs scoring I am not sure. The stickers were applied to the ears with and without magnets in a randomized fashion and the nurses instructed to score them using the PIPP scoring system. Interestingly, as per their unit policy all babies received sucrose as well before the intervention of a heel lance so I suppose the information gleaned here would be the use of magnets as an adjunctive treatment. No difference was noted in the two groups before and after the heel lance but during the procedure the magnet treated infants had a difference in means (SD): 5.9 (3.7) v 8.3 (4.7), p=0.04). No differences were found in secondary measures such as HR or saturation and no adverse effects were noted. The authors conclusions were that it was feasible and appears safe and as with most pilot studies warrants further larger studies to verify the results.
Should we run out and buy it?
One of the issues I have with the study is that in the introduction they mention that this treatment might be useful where kangaroo care (KC) is not such as a critically ill infant. Having placed infants who are quite sick in KC and watched wonderful stability arise I am not sure if the unit in question under utilizes this important modality for comfort.
The second and perhaps biggest issue I have here is that although the primary outcome was reached it does seem that there was some fishing going on here. By that I mean there were three PIPP scores examined (before, during and after) and one barely reached statistical significance. My hunch is that indeed this was reached by chance rather than it being a real difference.
The last concern is that while the intervention was done in a blinded and randomized fashion, the evidence supporting the use of this in the first place is not strong. Taking this into account and adding the previous concern in as well and I have strong doubts that this is indeed “for real”. I doubt this will be the last we will hear about it and while my skepticism continues I have to admit if a larger study is produced I will be willing and interested to read it.



 This study compared 5 different methods of delivering PPV to a 1 kg preterm manikin. The first was a standard self inflating bag, the next three different t-piece resuscitators and then the Next Step. For the first four the goal was to deliver a pressure of 20/5 at a rate of 40-60 breaths per minute. A test lung was connected to the manikin such that each device was used for a one minute period at three different levels of compliance (0.5 ml/cmH2O, 1.0 ml/cmH2O and then 2.0 ml/cm H2O representing increasing compliance. The goal of the study was to compare the methods in terms of delivering a volume of 5 mL to this 1 kg model lung. The order in which the devices were used was randomized for the 25 participants in the study who were all certified in NRP and included some Neonatologists.
This study compared 5 different methods of delivering PPV to a 1 kg preterm manikin. The first was a standard self inflating bag, the next three different t-piece resuscitators and then the Next Step. For the first four the goal was to deliver a pressure of 20/5 at a rate of 40-60 breaths per minute. A test lung was connected to the manikin such that each device was used for a one minute period at three different levels of compliance (0.5 ml/cmH2O, 1.0 ml/cmH2O and then 2.0 ml/cm H2O representing increasing compliance. The goal of the study was to compare the methods in terms of delivering a volume of 5 mL to this 1 kg model lung. The order in which the devices were used was randomized for the 25 participants in the study who were all certified in NRP and included some Neonatologists.