
by All Things Neonatal | May 26, 2017 | Neonatal, Neonatology
I have often said that if this came to pass as a mandatory requirement that I would make an announcement shortly thereafter that I was moving on to another career. I think people thought I was kidding but I can put in writing for all to see that I am serious! The subject has been discussed for some time as I can recall such talks with colleagues both in my current position and in other centres. The gist of the argument for staying in-house is that continuity is improved over that period and efficiency gained by avoiding handovers twice a day . How many times have you heard at signover that extubation will be considered for the following morning or to keep the status quo for another issue such as feeding until the next day. No doubt this is influenced by a new set of eyes being in the unit and a change in approach to being one of “putting out fires” overnight. The question then is whether having one Neonatologist there for 24 hours leads to better consistency and with it better outcomes. With respect to PICUs the AAP has previously recommended that 24 hour in-house coverage by an intensivist be the standard so should Neonatology follow suit?
A Tale of Two Periods
My friends in Calgary, Alberta underwent a change in practice in 2001 in which they transitioned from having an in-house model of Neonatologist coverage for 24 hours a day to one similar to our own centres where the Neonatologist after handover late afternoon could take call from home. An article hot off the presses entitled Twenty-Four hour in-house neonatologist coverage and long-term neurodevelopmental outcomes of preterm infants seeks to help answer this question. The team undertook a retrospective analysis of 387 infants born at < 28 weeks gestational age during the periods of 1998-2000 (24 hour period, N=179 infants) vs 2002 – 2004 (day coverage, N= 208 infants) with the goal of looking at the big picture being follow-up for developmental outcome at 3 years. This is an important outcome as one can look at lots of short term outcomes (which they also did) but in the end what matters most is whether the infants survive and if they do are they any different in the long term.
As with any such study it is important to look at whether the infants in the two periods are comparable in terms of risk factors for adverse outcome. Some differences do exist that are worth noting.
Increased risk factors in the 24 hour group
- Chorioamnionitis
- Maternal smoking
- Smaller birthweight (875 vs 922 g)
- Confirmed sepsis (23% vs 14%)
- Postnatal steroids (45% vs 8%) – but duration of ventilation longer in the day coverage group likely due to less postnatal steroids ( 31 vs 21 days)
All of these factors would predict a worse outcome for these infants but in the end for the primary outcome of neurodevelopmental impairment there was no difference. Even after controlling for postnatal steroids, birth weight, sex and 5 minute apgar score there was still no difference.
What might this mean?
Looking at this with a glass is half full view one might say that with all of the factors above predicting worse outcome for infants, the fact that the groups are not different in outcome may mean that the 24 hour model does indeed confer a benefit. Maybe having a Neonatologist around the clock means that care is made that much better to offset the effect of these other risk factors? On the other hand another explanation could also be that the reason there is no difference is that the sample just isn’t big enough to show a difference. In other words the size of the study might be underpowered to find a difference in developmental outcome.
One of the conclusions in this study is that the presence of a Neonatologist around the clock may have led to earlier extubation and account for the nearly 10 day difference in duration of ventilation. While I would love to believe that for personal reasons I don’t think we can ignore the fact that in the earlier epoch almost 50% of the babies received postnatal steroids compared to 8% in the later period. Postnatal steroids work and they do so by helping us get babies off ventilators. It is hard to ignore that point although I woudl like to take credit for such an achievement.
For now it would appear that I don’t feel compelled to stay overnight in the hospital unless it is necessary due to patient condition necessitating me having my eye on the patient. I am not sure where our field will go in the future but for now I don’t see the evidence being there for a change in practice. With that I will retire to my bedroom while I am on call and get some rest (I hope).

by All Things Neonatal | May 11, 2017 | kangaroo care, Neonatal, Neonatology, outcome, Parents Corner
Aside from me donning the costume in the above picture for the Kangaroo Challenge 2017 I learned something new today. Before I get into what I learned, let me say that I had the opportunity to put so many smiles on parents faces by walking around in this full body costume that I am grateful to Diane for finding this costume and Sue (you both know who you are) for purchasing it. Handing out cookies to the parents and children at the bedside and seeing them smile while knowing that they were under significant stress gave me the opportunity to interact with parents in a very different way than I am accustomed to as a Neonatologist so I am so thankful to have had that experience and yes if called upon I will do it again!
We even made the local news! CTV newscast
I posted the above picture on my Facebook page and to my surprise many of the comments led me to believe that Kangaroo Care is still something that needs a little nudging to get the word out about. I found this actually quite surprising given how immersed we are in Winnipeg with this strategy. When I think about new interventions in Neonatology it is synonymous in virtually all cases with an influx of dollars to achieve usher in the new program. Here is a program that is virtually free but only requires a commitment from families to spend the time at the bedside with their baby in the NICU.
I have been asked by many of my nursing colleagues to write something about Kangaroo care on this site and so here it is…
What is it?
You have likely heard of Kangaroo Care and you may have even seen some children receiving it in your hospital. Why is this so important?
Kangaroo Care (KC) or Skin to Skin Care (STS) is an ideal method of involving parents in the care of their premature infant. It fosters bonding between parents and their hospitalized infant, encourages the family to be with their child and thereby exposes them to other elements of neonatal care that they can take part in. While we know that many units are practising Kangaroo Care there is a big difference between having KC in your unit and doing everything you can to maximize the opportunity that your families have to participate.
There is much more to KC than simply holding a baby against your chest. For a demonstration of KC please watch the accompanying video and show it to any one in your units that may need a visual demonstration. This excellent video is from Nationwide Children’s Hospital and walks you through all of the important steps to get it right and maximize benefit.
Kangaroo Care Video
Before you reach the conclusion that KC only serves to enhance the parental experience it does so much more than that. The practice began in Bogota Columbia in 1979 in order to deal with a shortage of incubators and associated rampant hospital infections. The results of their intervention were dramatic and lead to the spread of this strategy worldwide. The person credited with helping to spread the word and establish KC as a standard of care in many NICUs is Nils Bergman and his story and commentary can be found here http://bit.ly/1cqIXlm
The effects of KC are dramatic and effective to reduce many important morbidities and conclusively has led to a reduction in death arguably the most important outcome. An analysis of effect has been the subject of several Cochrane Collaboration reviews with the most recent one being found here.
To summarize though, the use of KC or STS care has resulted in the following overall benefits to premature infants at discharge or 40 – 41 weeks’ postmenstrual age:
Reduction in
mortality (typical RR 0.68, 95% CI 0.48 to 0.96)
nosocomial infection/sepsis (typical RR 0.57, 95% CI 0.40 to 0.80)
hypothermia (typical RR 0.23, 95% CI 0.10 to 0.55)
Increase in
KMC was found to increase some measures of infant growth, breastfeeding, and mother-infant attachment
To put this in perspective, medicine is littered with great medications that never achieved such impact as simply putting your child against your chest. This is another shining example of doing more with less. This is not to say that modern medicine and technology does not have its place in the NICU but KC is simply too powerful a strategy not to use and promote routinely in the NICU.
Please join me in championing this wonderful technique and make a difference to all of our babies!
A sample of our parent letter to promote KC is found in the link below.
Parent letter II

by All Things Neonatal | May 7, 2017 | outcome, steroids
In our journey as Neonatologists and interdisciplinary teams we are forever seeking to rid or at least reduce the plague of BPD in the patients we care for. The PREMILOC trial was a double-blind, multicenter, randomized, placebo-controlled trial designed to test just that concept by introducing a low dose of hydrocortisone within 24 hours of birth. They enrolled infants born between 24 – 26+6 weeks of gestation and assigned them to receive either placebo or low-dose hydrocortisone 0.5mg/kg twice per day for 7 days, followed by 0.5 mg/kg per day for 3 days. The trial has been the subject of a previous post A Shocking Change in Position. Postnatal steroids for ALL microprems? Although the trial was stopped early due to financial concerns the authors demonstrated a 9% reduction in BPD using this strategy. The theory here in part is that the presence of hydrocortisone reduces inflammation and that this in turn may allow for better growth of lungs with time.
Why Not Adopt The Results Based on These Fantastic Results?
Steroids in preterm infants have a bad name. As discussed in previous posts on the topic the concern in all trials has been the potential impact of such medications on the developing brain. A nice summary of these concerns can be found in a paper in the CMAJ by the other “Canadian Neonatal Blogger” from 2001 in which he quoted the risk of cerebral palsy increasing from about 1 in 6 babies to 1 in 3 if babies born at < 28 weeks were exposed to postnatal steroids. Neurodevelopmental impairment overall would change from 1 in 4 to 1 in 3 if such exposure occurred. This paper and others expressing concerns over the effect of postnatal steroids led to a change in practice from more ubiquitous use to one restrained to only in those cases where the patient was nearing the end of all other options. This meant holding out for such therapy until such patients were at 90% or more O2 and on high mean airway pressures. Although not formally studied I was very concerned at the time with using this approach as I felt it was a “fait de complet” that they would either die or have significant developmental impairment should they survive due to the complications of having such severe BPD. It is critical to note though that the outcomes from these long term studies were in infants exposed to much longer courses of dexamethasone and at high doses that are used today.
Over the years with the development of the DART protocol and other more gentle approaches to steroids we as a group relaxed and certainly rescue courses of lower dose steroids have crept into practice when patients seem to be “stuck” on the ventilator.
Drumroll Please…
The results of the PREMILOC follow-up study are now here and in short they look good. Patients were followed up at an average age of 22 months and included a medical history, anthropometric measures, respiratory status, standardized neurological examination based on specific definitions of disabilities, and quantitative neurodevelopmental assessment using the revised Brunet-L.zine (RBL) scale. Follow-up was 93% in the hydrocortisone and 90% in the placebo arm which is important as we need not worry about the missed patients influencing the results to a significant degree if they had been included. Although some post-hoc analyses were done what I am most interested in is the primary outcome which is shown below.
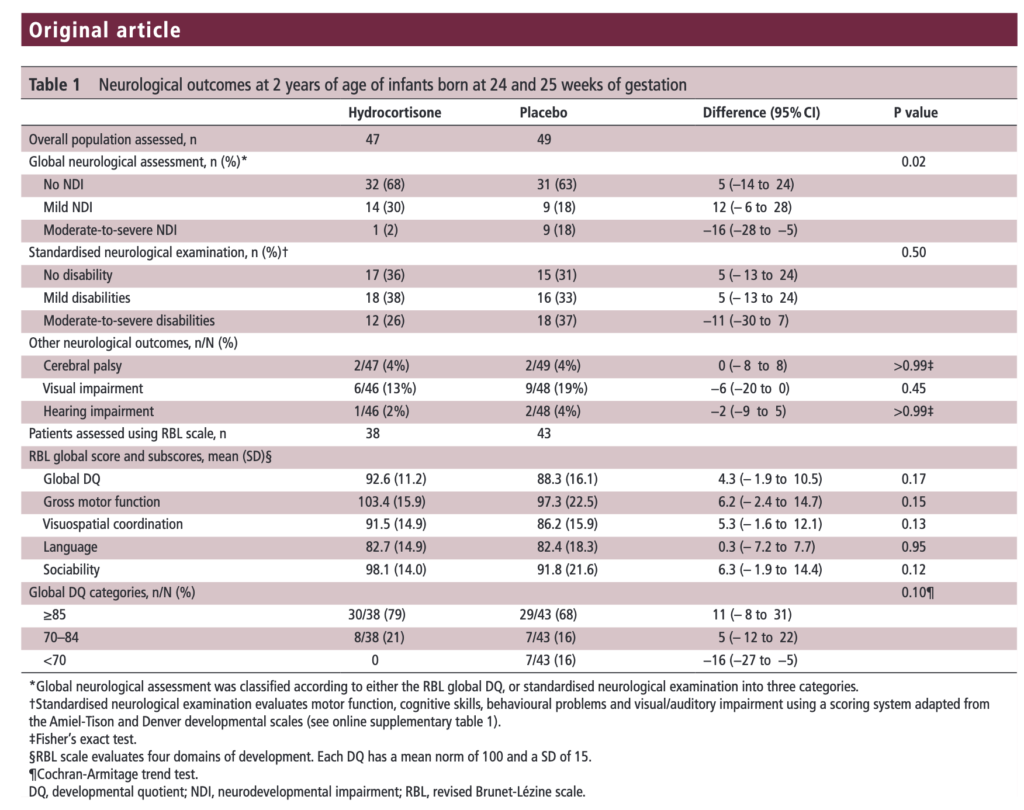
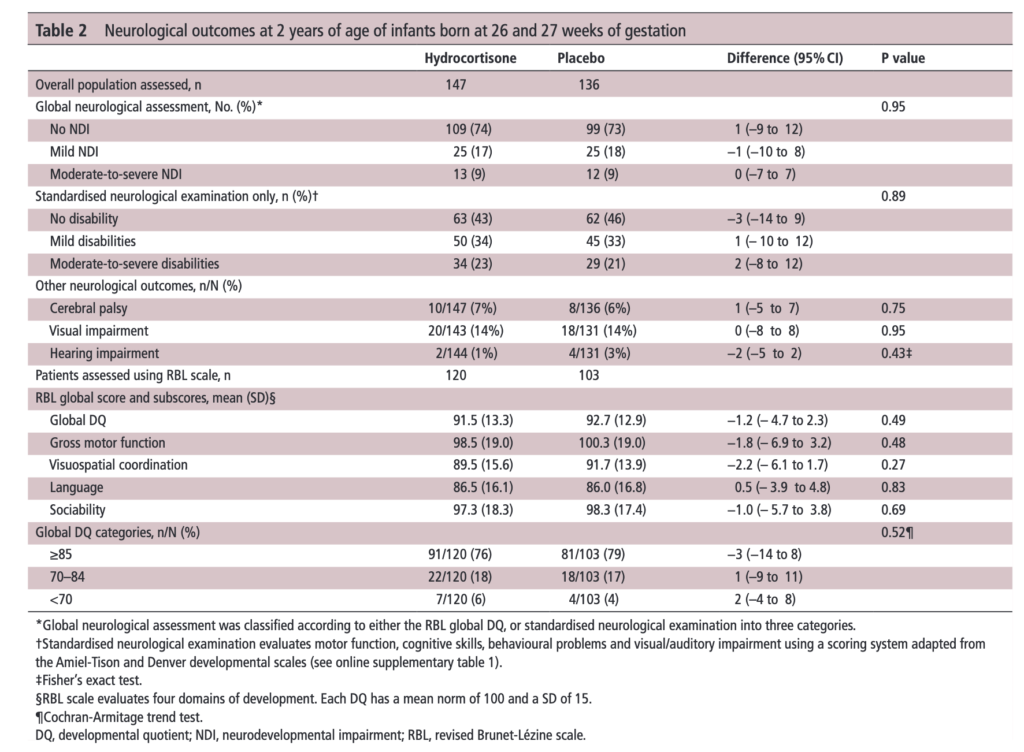 There was no difference in either neurodevelopment overall or any of the subcategories. This provides a great deal of reassurance to those who provide steroids this way. There will be those however that argue the study is too small. While a larger study might be better able to address whether there is a small difference in outcome I don’t think we will see one anytime soon. It is one of the challenges we face in Neonatology. Unlike the adult world with studies of thousands of patients, due to the small number of patients born at <28 weeks it is always a challenge to recruit into such large volume trials. We can compare trials by doing meta analyses or systematic reviews and perhaps that is where we will head with this study although given that different steroids will have been used (thinking dexamethasone as in the DART study) this will always be left open to question.
There was no difference in either neurodevelopment overall or any of the subcategories. This provides a great deal of reassurance to those who provide steroids this way. There will be those however that argue the study is too small. While a larger study might be better able to address whether there is a small difference in outcome I don’t think we will see one anytime soon. It is one of the challenges we face in Neonatology. Unlike the adult world with studies of thousands of patients, due to the small number of patients born at <28 weeks it is always a challenge to recruit into such large volume trials. We can compare trials by doing meta analyses or systematic reviews and perhaps that is where we will head with this study although given that different steroids will have been used (thinking dexamethasone as in the DART study) this will always be left open to question.
Is it worth it?
I suppose the real question here is the following for a parent to consider. “Would you like your baby to receive hydrocortisone shortly after birth with a 7% reduction in the risk of BPD at 36 weeks bearing in mind that although we don’t think there is an impact on long term development we aren’t certain yet”.
I guess to answer this question you need to think about the first part of the question. Is BPD at 36 weeks a good outcome to look at for benefit? The Canadian Neonatal Network has recently called for a rethink on this The New BPD That Matters. It turns out that it is 40 weeks and not 36 weeks that has the greatest prediction for respiratory morbidity after discharge. If you were to move the goal post to 40 weeks from 36 I strongly suspect one would see the 9% reduction in BPD as shown in the PREMILOC trial vanish. If that is the case, would a slightly earlier extubation time be enough to motivate families to take the plunge?
Although I often cringe at the expression “more trials are needed”, I think at least a combination of studies to achieve greater confidence in outcome may be needed. Barring that, we might just have to sit tight and accept that while there may be a little bit to be gained with the use of the PREMILOC protocol it may just not be enough to be clinically warranted at this time. May want to wait for the next big thing to tackle BPD…



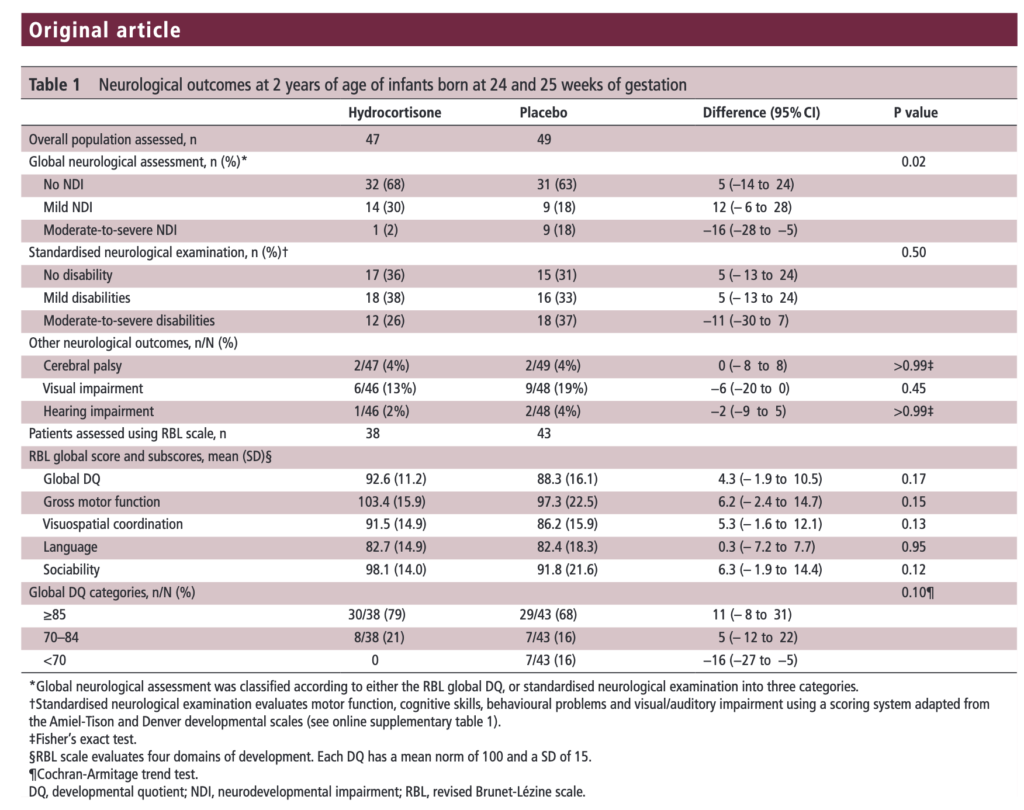
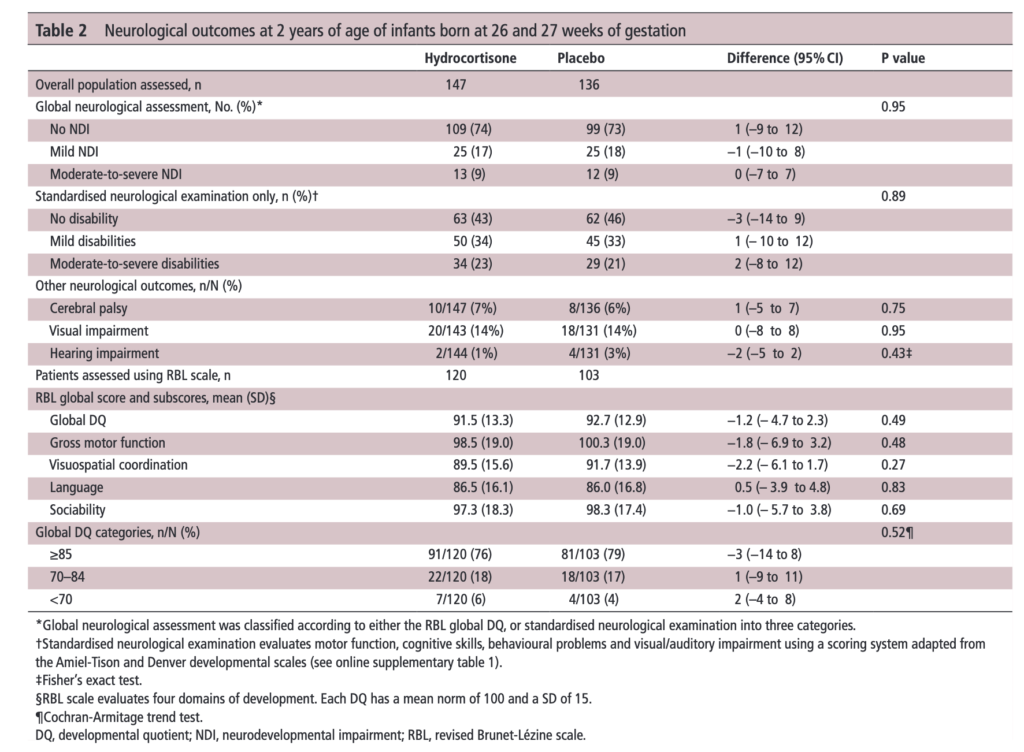 There was no difference in either neurodevelopment overall or any of the subcategories. This provides a great deal of reassurance to those who provide steroids this way. There will be those however that argue the study is too small. While a larger study might be better able to address whether there is a small difference in outcome I don’t think we will see one anytime soon. It is one of the challenges we face in Neonatology. Unlike the adult world with studies of thousands of patients, due to the small number of patients born at <28 weeks it is always a challenge to recruit into such large volume trials. We can compare trials by doing meta analyses or systematic reviews and perhaps that is where we will head with this study although given that different steroids will have been used (thinking dexamethasone as in the DART study) this will always be left open to question.
There was no difference in either neurodevelopment overall or any of the subcategories. This provides a great deal of reassurance to those who provide steroids this way. There will be those however that argue the study is too small. While a larger study might be better able to address whether there is a small difference in outcome I don’t think we will see one anytime soon. It is one of the challenges we face in Neonatology. Unlike the adult world with studies of thousands of patients, due to the small number of patients born at <28 weeks it is always a challenge to recruit into such large volume trials. We can compare trials by doing meta analyses or systematic reviews and perhaps that is where we will head with this study although given that different steroids will have been used (thinking dexamethasone as in the DART study) this will always be left open to question.