by All Things Neonatal | Sep 29, 2016 | ventilation
This may sound familiar as I wrote about this topic in the last year but the previous post was restricted to infants who were under 1000g. High Flow Nasal Cannula be careful out there had a main message that suggested the combined outcome of BPD or death was more prevalent when HFNC is used alone or with CPAP than when CPAP is used alone. The question remains though whether this applies to larger infants. Without looking at the evidence for that combined outcome most people would say there is unlikely to be a difference. Larger more mature babies have a much lower risk of BPD or death so proponents of HFNC would say it is simpler to use and helps prevent nasal breakdown as well. The question remains as to whether all outcomes are the same in larger infants and that is the point of this post.
A Non-Inferiority Trial
First off it is important to understand what this type of trial is. The first requirement is that the two treatments have both been compared to a placebo and found to be both effective. Once you establish that you have a choice between two treatment options then you eliminate the placebo and compare them head to head. What you are looking for in this type of trial is to determine not whether one is better than the other but that there is no difference in a clinical outcome of interest. If you find no difference then the next step is to look at other outcomes that might be of interest and see if there are any benefits to picking one versus the other. In the case of CPAP vs HNFC, if a non-inferiority trial showed no difference in an important outcome such as length of stay but nasal breakdown was less with HFNC it might lead a unit to use HFNC for their infants. Okay, now that we have that cleared up we can move on to an actual study examining this very subject.
This was an interesting study with a great name (The HIPSTER trial) that enrolled infants > 28 weeks and 0 days with none of the infants receiving surfactant but either being randomized to HFNC or CPAP after delivery. These infants were your typical modern day cohort of babies who may avoid intubation and surfactant by establishing FRC early with positive pressure applied to the nose through one of these devices. The end point for the study was treatment failure within 72 hours. If an infant failed in the HFNC they could have a trial of CPAP whereas in the CPAP group they were intubated. For each infant in the HFNC group flow was set from 6-8 l/min and for CPAP 6-8 cmH2O.
Treatment was considered to have failed if an infant receiving maximal support (high-flow therapy at a gas flow of 8 liters per minute or CPAP at a pressure of 8 cm of water) met one or more of the following criteria:
- FiO2 of 0.4 or higher
- Arterial or free flowing cap gas with a pH of 7.2 or less plus a pCO2 > 60 mm Hg obtained at least 1 hour after starting treatment
- Two or more episodes of apnea requiring positive-pressure ventilation within a 24-hour period or six or more episodes requiring any intervention within a 6-hour period.
- Infants with an urgent need for intubation and mechanical ventilation.
So what happened?
The trial randomized 583 infants (278 HFNC, 286 CPAP) but was halted by the data and safety monitoring committee after an analysis of the first 515 revealed that the outcome was worse in the HFNC group (25.5% failure rate vs 13.3 for CPAP). Interestingly treatment failures were more common in babies below and above 32 weeks so it was not just the smallest infants who failed.
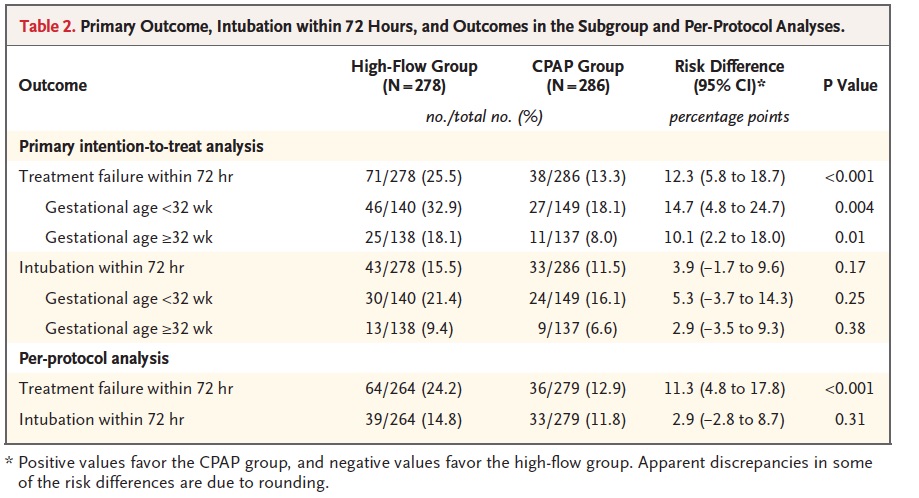 Another interesting finding was that the most common reason for treatment failure was criteria 1 (FiO2 > 40%) while intubation was higher for all infants but did not reach statistical significance. Curiously what did reach a significant difference was criteria #4 (18.4% urgent intubations in the CPAP group vs 5.6% in the HFNC group). You might be tempted to therefore ponder which is worse, a little O2 or being intubated but you need to recall the trial design which was set up to provide this kind of result. If you failed HFNC you were placed on CPAP whereas if you failed CPAP you were intubated. In the HFNC group, 78 infants were deemed to have failed but 28 of them were in fact “rescued by CPAP”. It therefore isn’t a fair comparison when it comes to urgent intubation since if you failed CPAP there wasn’t another option.
Another interesting finding was that the most common reason for treatment failure was criteria 1 (FiO2 > 40%) while intubation was higher for all infants but did not reach statistical significance. Curiously what did reach a significant difference was criteria #4 (18.4% urgent intubations in the CPAP group vs 5.6% in the HFNC group). You might be tempted to therefore ponder which is worse, a little O2 or being intubated but you need to recall the trial design which was set up to provide this kind of result. If you failed HFNC you were placed on CPAP whereas if you failed CPAP you were intubated. In the HFNC group, 78 infants were deemed to have failed but 28 of them were in fact “rescued by CPAP”. It therefore isn’t a fair comparison when it comes to urgent intubation since if you failed CPAP there wasn’t another option.
Not a total loss
Nasal trauma was indeed much lower in the HFNC group, occurring only 8.3% vs 18.5% of the time with CPAP. Pneumothorax was also found to be significantly different with none of the patients in the HFNC group having that complication vs 2.1% in the CPAP group. What this study tells us is that as a primary modality to treat newborns with RDS who have not received surfactant it is preferable to use CPAP in the first 72 hours. Some of you may say it might not say that at all but consider the impact of having more babies exposed to high FiO2. We know from other studies that high FiO2 can be quite damaging to preterm infants and this study was certainly not powered to look at all those important outcomes such as ROP, PVL and BPD. The authors report them and found no difference but without adequate power to show a difference I wouldn’t take much comfort in those findings.
I think were things may settle out though is what to do in more mature infants. There is no question that for those on chronic respiratory support there is some risk of nasal breakdown. Although I don’t have much experience with HFNC I would think that for the older patient who either already has BPD at 36 weeks or is close to that point but reliant on +4 or +5 CPAP that HFNC might help “give them a break”. As such I don’t see this as a total loss but rather an option to try when CPAP for whatever reason is not tolerated.
As a primary therapy for non-invasive management RDS I will keep my CPAP for all babies thank you.

by All Things Neonatal | Sep 21, 2016 | bioethics, preemie
While we draw the line at 22 5/7 weeks for offering active resuscitation where I work, what does one do when the family requests resuscitation prior to that point. While I am a clear fan of social media, one consequence of having such widely available information at our fingertips is that families may already know before you come to speak with them that were they only to have been born in another place like Montreal, the cutoff would have been lower. When faced with such demands what does one do? Well, in the case of my own experience it was to give in to the demands of the parents. While I certainly discourage such heroic attempts, what is one to say when the family having received your opinion states “I want everything done”. Informed consent is a tricky one in that if you approach a family for informed consent and they refuse to accept your desired direction of care where does that leave you? It leaves you with informed refusal and if we are being fair to our families we have to accept that informed refusal is just as important as informed consent.
Nothing New?
The truth is informed refusal has been recognized as being critically important to decisions in patient care for many years. Previous papers on the subject include a nice review by Ridley DT, Informed consent, informed refusal, informed choice–what is it that makes a patient’s medical treatment decisions informed? What this really comes down to is a patient’s right to personal autonomy and self determination. Does a parent in this case have the right to do what they want even in the face of dismal odds? Furthermore where are we placing the importance of values? Is it physician or patient centric? In the physician centric world, after we impart our experience and wisdom we expect the patient to generally follow through with what we are steering them towards in cases such as this. Informed consent of course is meant to be free of coercion but let’s face it, when we truly believe something is fairly futile are we honestly playing an impartial role or using our tone, body language and choice of words to direct families down the path that fits with our own beliefs and values? I would offer that in most cases when we seek informed consent what we are really doing is seeking to pass along the justification for what we are wanting to do and then moving forward once obtained.
What do we do though when after hearing the pros and cons the family still opts to move forward and worse yet is in disagreement with our preferred plan. Well there you arrive at informed refusal. If after hearing our best transfer of information the family still wants to proceed what does one do? As a physician if I believe something is completely futile and I find myself in this position then I am truly at fault. Seeking informed consent in this situation was completely inappropriate. One should have simply said there is nothing that can be done.
The Montreal Example
Getting back to the example that started this piece, if a family knows that there are places in Canada (or let’s be honest, if I know there are survivors in Canada at 22 weeks) that resuscitate and have survivors then it isn’t really futile is it. I know many of you would say “but the odds are so stacked against the baby” and “they don’t know what they are getting themselves into” but what does one say in this circumstance when despite your best attempts the family still wants to resuscitate?
Therein lies the challenge. If we approach this as an opportunity for informed consent we need to accept that we may find ourselves face to face with “informed refusal”. Now I need to be careful here. I am not advocating a wide open optimistic approach to resuscitation at 22 weeks. What I am suggesting though is that if you find yourself coming into a unit somewhere in the next few months and find yourselves looking at a 22 week infant don’t jump to conclusions! Did the family despite all the warnings want this? Don’t leap to the thought that the Neonatologist is pushing for this but rather it may indeed be a case of a family advocating for their child against all odds. It may not be something that we agree with in many cases but are we thinking from the perspective of the family or our own value system?

by All Things Neonatal | Sep 16, 2016 | Uncategorized
Campaign Closed October 13,2016! Thank you everyone for the $9359.00 raised!
First off I would like to thank everyone who has contributed to the fundraiser that All Things Neonatal has organized. Each gift no matter how small makes a difference one person at a time. I am overwhelmed not just by the generosity of the people who follow the Facebook page and this blog but by the numbers of people that have an interest in well… All things that are neonatal! The same day as the campaign began the Facebook page passed 10000 likes and that is saying something. When I started I had no idea where this would go and here we are just a year and a half in and by definition we can now say goodbye to our classification as a town and consider ourselves a city having reached 10000!
With respect to the subject of generosity though I would like to make special mention and a public thank you to two very large donations that came today. The first is from Vickar Community Chevrolet who gave $500 towards the cause. Given that I was looking for donations as small as $1 per member on the site I consider this to be quite amazing. It is quite inspiring to think that a company operating completely outside of the health care field still takes the time to recognize the importance of the needs of babies in our hospital.
The second “shout out” I feel the need to give is to a company that to be honest I had not heard of until today. The company is The Nanny Company Inc who operate out of Winnipeg and I am sure would be of use to many of the families that I have discharged who themselves may find themselves in need of such help. The Nanny Company today gave $1000 towards the fundraiser and with their donation I am proud to say we crossed the first threshold of $2000 and I am proud to announce we can officially buy one milk warmer for the NICU in Winnipeg!
By the way the Nanny Company also have a Facebook page as do Vickar Community Chevrolet so check them out to see what they do!
It is these kind of selfless acts that make me believe in the power of community. Whether you live in Winnipeg or not it doesn’t really matter. We all share space on this planet of ours and whether a baby is in Winnipeg, LA, Auckland or Capetown they all need our help. With that I ask you again whether you have followed this page or not if you can spare the cost of a cheap cup of coffee and use the power that we have with 10000 members to reach our goal of at least 4 milk warmers. If you would consider it click on this link below to Hold Their Hand and do something that you will feel great about this Weekend!
Hold Their Hand

by All Things Neonatal | Sep 15, 2016 | Neonatal, Neonatology, Uncategorized
Campaign Closed October 13,2016! Thank you everyone for the $9359.00 raised!
Each day the number of people following these sites grows and at the time of this post, the largest following on Facebook has over 8200 people who receive the feed on a daily basis. That is nothing short of remarkable and I hope that each of you gets something out of my writings and postings. I recognise that each post may not “light it up” in your mind but if you get at least a few “a ha” moments along the way then I am very happy that you have found these sites!
What This Is Not!
As I begin hinting at money, many of you may be thinking “here we go”, he is finally asking for some payment for this site! To be clear I have no interest in personal financial gain from this hobby I have developed, but rather find my joy in sharing ideas, getting your feedback and helping to generate interest overall in topics pertaining to Neonatology. I have no intention of ever asking for such payment but that doesn’t mean that I might not want to help someone else. For those of you who make philanthropy a part of your lives you will know the joy that comes from helping others. Being able to help others need not take tremendous dollars per donor when you have many people banding together to help a cause. This is the power that I am hoping to harness through this initiative and make a difference in care to our babies in hospital.
For the past year and a half, I have put my fingers to the keyboard to hopefully share my knowledge and expertise with you about an industry I am so passionate about.
My Philanthropic Side
When I am not busy finding content for the sites or being a Neonatologist, I am quite dedicated to philanthropy. One thing people may not realise about our province/country is that the government helps out the best they can financially but with the heavy demands of our province, they can’t meet all the needs. That’s why I’m proud of my partnership with the Children’s Hospital Foundation of Manitoba. The Foundation’s donors have helped bridge the gap so our hospital doesn’t go without the specialised items they need. From ultrasounds, starting a breast milk depot, specialised pediatric equipment and funding a position to support Quality Improvement in our unit to a soon to be announced Family Support coordinator position and so much more. But now, I turn to you to help us make the next difference in our unit.
The other day as the Facebook page hit 8,000 followers a thought struck me. What if I asked everyone on the page to just give $1 towards the purchase of a piece of equipment for babies in our units?
Hold Their Hand
In the Neonatal Intensive Care Unit (NICU), they are watched closely to make sure they are getting the right balance of fluids and nutrition. Incubators or special warmers help babies maintain their body temperature. This reduces the energy the babies have to use to stay warm and allow them to use that energy elsewhere.
Premature babies need to receive good nutrition so they grow at a rate close to that of babies still inside the womb. Babies born under 38 weeks have different nutritional needs than babies born at full term (after 38 weeks). They often have problems feeding from a bottle or a breast. This is because they are not yet mature enough to coordinate sucking, breathing, and swallowing.
Many NICUs will give donor milk from a milk bank to high-risk babies who cannot get enough milk from their own mother. But because the baby must be kept at a certain temperature to stay warm, so does their milk. 
Thanks to the generous support of donors to the Children’s Hospital Foundation of Manitoba, 12 milk warmers have been purchased. However, we need 24 more warmers to keep up with demand. Each one costs $2,000 and will make a huge impact. An impact to help our babies get the nutrition they need at the temperature they require to survive and thrive.
So let’s hold their hand and let’s do it together! Has this journey of learning been worth at least $1 to you? If it has, then please help make a difference by giving at least $1. Giving more will only increase the power of this campaign! If you aren’t able to donate $1 or more, I ask that you share this post and challenge your friends to help make a difference to the over 1,000 patients we see a year. Click the link below to donate and make your difference today.
chfm.convio.net/help-hold-their-hand

by All Things Neonatal | Sep 7, 2016 | apnea of prematurity, Uncategorized
A question that we are asked from time to time is whether a home apnea monitor should be purchased after discharge from the hospital. The typical parent is one who has experienced the ups and downs of apnea of prematurity and is faced with the disturbing notion of coming off monitors and going home. “What if he has an event at home and I don’t know”? This leads to a search on the web for home monitors which finds numerous options to choose from. This is where things get interesting from a North American perspective.
In the two centres I have worked at in Canada our answer to such a question is to save your money and not buy one. Contrast this with two families I know in the US who were sent home by the hospital with home apnea monitors. How can the advice between the two nations be so different? I suspect the great risk of a lawsuit in the US is responsible at least in part but it may have to do with risk tolerance as well.
What does the evidence say?
First off, one might surmise that the use of a home apnea monitor helps hospitals move patients to the home faster than those centres that don’t prescribe them. A 2001 Cochrane systematic review on the subject noted that this was not the case and determined that out of nearly 15000 neonates studied the greatest predictor of sending such babies home on monitors was physician preference.
In the largest home monitoring study of its kind, the Collaborative Home Infant Monitoring Evaluation (CHIME) demonstrated some very important information. First off, ex-preterm infants have events and some of them quite significant after discharge. What the study which followed discharged infants at risk of SIDS in the home environment found though was that term infants also have events although less severe. Does this mean that everyone should run out and buy such monitoring equipment though? No! The main reason was that while the study did show that events may continue after discharge, it failed to show that these events had any relation to SIDS. The apneic events noted in hospital disappeared long before the arrival of a risk for SIDS. They really are separate entities.
The other issue with such monitors pertains to false alarms which can lead to sleepless nights, anxiety in parents and eventual abandonment of such technology. This led the AAP in 2005 to declare that they did not endorse such practice. Having said that, it is clear from my own experience with two US ex-preterm infants that this practice remains alive and well.
Could this be the solution?
One of my followers sent me this tonight and I have to say at the very least I am intrigued. The device is called the Owlet and was featured in this article The Sock That Could Save Your Babies Life. 
Watch the video here.
This monitor has me a little excited as it brings the home apnea monitor into the modern era with smart phone connectivity and at the same time helps the developers of this technology use data collected every two seconds to get a clearer picture on breathing patterns in infants that have been sent home. The saturation monitor in a sock is at the core of this technology which is meant to keep the probe in a relatively stable location. It brings another angle to the concept of wearable tech! What I find most interesting is the claim by the manufacturer that the device has a false alarm rate similar to that of a hospital saturation probe which would make it quite reliable.
I note though that the product has not received FDA approval yet (at least on the source I looked at) but is being worked on. The challenge though is whether this will truly make a difference. It may well have an excellent detection rate and it may in fact detect true apnea leading to bradycardia and cyanosis. What it won’t do though is change the natural history of these events once home. It may capture them very well but I suspect the four events that the mother in the video describes may have been self resolving if she hadn’t intervened. We know from the CHIME study that the events seen in the home did not lead to death from SIDS so I see no reason why these would be different.
Is it useless?
I suppose that depends on your perspective. From a data collection point, obtaining data every two seconds in a cloud based storage environment will allow this company to describe the natural history of respiratory patterns in ex-preterm infants better than I suspect has ever been done before. From a population standpoint I suppose that is something! At an individual level I suppose it depends on your strength of “needing to know”. This may well be the best monitor out there and it may one day be the most reliable. Will it save your baby’s life? I doubt it but might it give you peace of mind if it false alarms very infrequently? I think it just might but based on the low likelihood of it changing the outcome of your baby you won’t see me recommending it. If I come across one make no mistake about it, I will want to play with it myself!

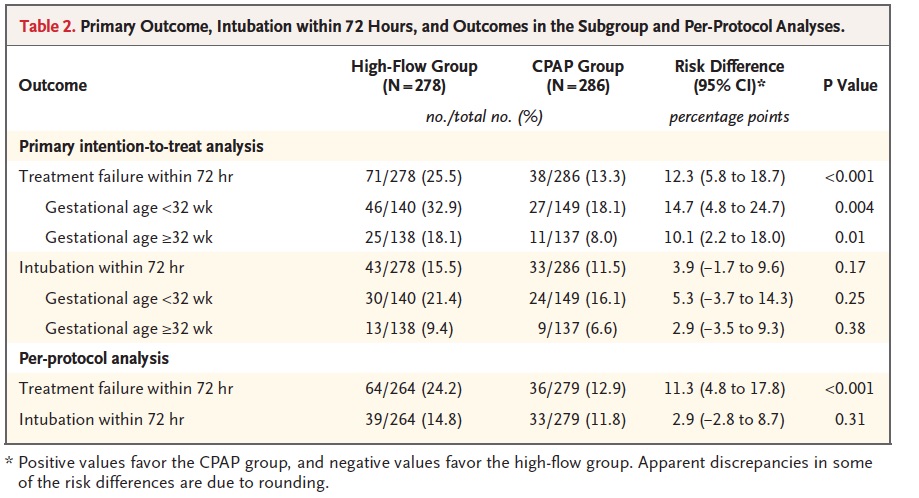 Another interesting finding was that the most common reason for treatment failure was criteria 1 (FiO2 > 40%) while intubation was higher for all infants but did not reach statistical significance. Curiously what did reach a significant difference was criteria #4 (18.4% urgent intubations in the CPAP group vs 5.6% in the HFNC group). You might be tempted to therefore ponder which is worse, a little O2 or being intubated but you need to recall the trial design which was set up to provide this kind of result. If you failed HFNC you were placed on CPAP whereas if you failed CPAP you were intubated. In the HFNC group, 78 infants were deemed to have failed but 28 of them were in fact “rescued by CPAP”. It therefore isn’t a fair comparison when it comes to urgent intubation since if you failed CPAP there wasn’t another option.
Another interesting finding was that the most common reason for treatment failure was criteria 1 (FiO2 > 40%) while intubation was higher for all infants but did not reach statistical significance. Curiously what did reach a significant difference was criteria #4 (18.4% urgent intubations in the CPAP group vs 5.6% in the HFNC group). You might be tempted to therefore ponder which is worse, a little O2 or being intubated but you need to recall the trial design which was set up to provide this kind of result. If you failed HFNC you were placed on CPAP whereas if you failed CPAP you were intubated. In the HFNC group, 78 infants were deemed to have failed but 28 of them were in fact “rescued by CPAP”. It therefore isn’t a fair comparison when it comes to urgent intubation since if you failed CPAP there wasn’t another option.