by All Things Neonatal | Nov 26, 2015 | Neonatal, resuscitation
As I read through the new NRP recommendations and began posting interesting points on my Facebook Page I came across a section which has left me a little uneasy. With respect to a newborn 36 weeks and above who is born asystolic and by ten minutes of age continues to remain so and has an apgar score of zero the recommendation that has been put forward is this:
An Apgar score of 0 at 10 minutes is a strong predictor of mortality and morbidity in late-preterm and term infants. We suggest that, in babies with an Apgar score of 0 after 10 minutes of resuscitation, if the heart rate remains undetectable, it may be reasonable to stop resuscitation; however, the decision to continue or discontinue resuscitative efforts should be individualized. Variables to be considered may include whether the resuscitation was considered to be optimal, availability of advanced neonatal care, such as therapeutic hypothermia, specific circumstances before delivery (eg, known timing of the insult), and wishes expressed by the family (weak recommendation, very-low-quality evidence).
There are some significant problems with this part of the statement.
- They claim that the apgar score at ten minutes is a strong predictor but when you look at the analysis of the evidence presented in the body of the paper it is weak at best. I am not clear how one declares the prediction is strong in the face of poor evidence but I will acknowledge intuitively that this makes some sense but do challenge them on the use of the word “strong”.
2. They are correct in acknowledging that the introduction of hypothermia in such settings has changed the landscape in as much as I find it quite difficult to prognosticate unless a child is truly moribund after resuscitation. Given such uncertainty it is concerning to me that this recommendation may be committed to memory incorrectly in some places that do have access to cooling and may be used more rigidly as though shalt stop at 10 minutes.
3. In the middle of a resuscitation it is quite difficult to process all of the facts pertaining to a particular newborn while orders for chest compressions, emergency UVCs and epinephrine are being given. Can we really individualize within ten minutes accurately and take the families wishes truly into account? This just does not seem practical.
4. The families wishes are taken into account but inserted as a “weak recommendation”. How can the wishes of the family in any family centred model of care be minimized in such a way even if we believe the situation to be dire?
5. Since the introduction of hypothermia there appears to be a near 50% survival rate in such newborns and as the authors state 27% of survivors who received cooling had no moderate or severe disability. Here in lies my greatest issue with this guideline and that is the hypocrisy this position takes when you compare populations at 23 and 24 weeks gestational age.  Survival at these GA in the recent NEJM study of almost 5000 preterm infants under 27 weeks were 33 and 57 % respectively at 23 & 24 weeks with rates of survival without moderate or severe disability being 16 and 31% in the two groups. The fallout from this and other studies at the extremes of gestational age have been that we should be more aggressive as the outcomes are not as bad as one would predict. How can we argue this for the 23-24 week infants and for term infant with the same likelihood of outcomes we would unilaterally stop in many centres?!
Survival at these GA in the recent NEJM study of almost 5000 preterm infants under 27 weeks were 33 and 57 % respectively at 23 & 24 weeks with rates of survival without moderate or severe disability being 16 and 31% in the two groups. The fallout from this and other studies at the extremes of gestational age have been that we should be more aggressive as the outcomes are not as bad as one would predict. How can we argue this for the 23-24 week infants and for term infant with the same likelihood of outcomes we would unilaterally stop in many centres?!
So Now What Do We Do?
We are supposed to be practising family centred care and much like the argument at the edge of viability the same should apply here. The wishes of the family should never be minimized. Arguably it may be very difficult in such an unexpected scenario to appraise a family of the situation and have clarity around the issue but if a heart rate can be restored after a few more minutes do we not owe it to the family and the child to bring the infant back to the NICU and see what transpires especially if cooling is available?
The million dollar question of course is where do we draw the line? No heart rate at 15, 20 minutes? Based on the evidence thus far it seems to me that a little longer than 10 minutes is reasonable especially in well equipped centres with access to cooling and modern ventilation and treatments for pulmonary hypertension. How long though must be individualized and should be determined in partnership with the team caring for the patient which must include the family.

by All Things Neonatal | Nov 17, 2015 | Neonatal, Neonatology, preemie, Prematurity, Uncategorized
Another year has passed and another World Prematurity Day is upon us. I thought about what to write for this day that draws attention to premature infants worldwide and was hit with many ideas which no doubt will form the basis for many posts to come. There was one thought that struck me though as being so important to think about as we push forward, striving to improve survival across the globe for our smallest patients. There is no doubt that you will have heard the expression “just because we can do something, should we?” In 2015 I don’t think this applies more than at this very moment.
At a Tipping Point
You see we are at a tipping point as Malcolm Gladwell explained so brilliantly in his book by the same name.  In April of 2015 Rysavy et al published the results of survival and morbidity data for infants born in 24 US hospitals between the ages of 22 – 26 weeks. The nearly 5000 infants included demonstrated two very important things. Firstly, survival is possible at 22 and 23 weeks and there is a chance, albeit less than 50% that these infants will survive without moderate or severe disability. Secondly, at these gestational ages 75% of hospitals included provided active resuscitation to these infants. Given that this is the largest study out there and shows that survival is possible and we can expect to see some good outcomes it would seem logical to move forward with universal resuscitation of these infants would it not?
In April of 2015 Rysavy et al published the results of survival and morbidity data for infants born in 24 US hospitals between the ages of 22 – 26 weeks. The nearly 5000 infants included demonstrated two very important things. Firstly, survival is possible at 22 and 23 weeks and there is a chance, albeit less than 50% that these infants will survive without moderate or severe disability. Secondly, at these gestational ages 75% of hospitals included provided active resuscitation to these infants. Given that this is the largest study out there and shows that survival is possible and we can expect to see some good outcomes it would seem logical to move forward with universal resuscitation of these infants would it not?
You Are Going To Practice on What?!
As the saying goes though, “Perfect Practice Makes Perfect”. Not all hospitals have equal performance at these gestational ages which is demonstrated in the ranges of outcomes across hospitals as shown in the Rysavy paper. To even suggest that we need to practice on premature babies will no doubt leave many of you feeling queasy but in essence that is what is truly needed to improve our outcomes further. An infant born at 22 – 24 weeks is vastly different than one born at a later gestational age. Their skin is extremely fragile and prone to breakage with resultant risk of infection. Their lungs are in a stage of development that has yet to produce any real abundance of gas exchanging alveoli and their brains lacking the sulci and gyri that are to come many weeks later. They are in need of meticulous “best practice” care and without that their outcomes are certainly to be influenced. Depending on the centre though, you may see 5, 10, 15, 20 patients a year at these ages. How can a team possibly gain enough experience in treating these children appropriately if they see 1 or 2 every two months? Add to this that you may have 10 different Neonatologists so on average each of you may take care of one patient a year at birth. This is a recipe prone to poor outcomes if you ask me.
The Evolution of the Small Baby Unit
The answer no doubt will lie in creating smaller teams; so called “Small Baby Units”. Such units have small groups of health care providers dedicated to treating such infants thereby increasing the frequency of individuals exposure to these babies. There is some recent evidence published in Pediatrics that supports this notion. Small Baby Unit Improves Quality and Outcomes in Extremely Low Birth Weight Infants. In this study a period of two years before and four years after opening such a unit were compared across a number of measures. The findings were as follows “There was a reduction in chronic lung disease from 47.5% to 35.4% (P = .097). The rate of hospital-acquired infection decreased from 39.3% to 19.4% (P < .001). Infants being discharged with growth restriction (combined weight and head circumference <10th percentile) decreased from 62.3% to 37.3% (P = .001). Reduced resource utilization was demonstrated as the mean number per patient of laboratory tests decreased from 224 to 82 (P < .001) and radiographs decreased from 45 to 22 (P < .001).” I hope you would agree that achievements such as these are worth the effort to create such an environment. Future studies I believe will confirm these findings although having the gold standard RCT may be difficult to achieve as I suspect we will have lost equipoise.
This brings me to the final point though and that is whether we are ready as a health care system for the increase patient load that this change will bring about. Based on an expected stay of 4 months for a baby born at this age and knowing the average number of such babies delivered per year, we would be looking at about 600 patient days per year added to each hospital’s occupancy in our two centres.  This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.
This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.
How do we educate families about what to expect in the long run?
How do we support these families when they make such difficult decisions either way?
How do we support our front line staff who may hold quite discrepant viewpoints about what is “right” yet expect them to function as one team moving clearly in a direction that supports the family?
How do we ensure that our focus on our smallest infants does not distract us from the attention needed by those born at later gestational ages?
I could go on but these are just some of the questions that I hope the next year begins to tackle. We are in the midst of an evolutionary point in Neonatology and we owe it to ourselves and the families we care for to navigate this change as best we can.

by All Things Neonatal | Nov 12, 2015 | Neonatal
In 2018 where do we stand on this question? Upcoming retrospective trials and work by EPIQ-4 may help to resolve this issue. In the meantime what does the existing evidence say?
The decision to extubate an extremely low birthweight infant is one of the most common sources of disagreement and anxiety in the NICU. As a resident, I recall an unwritten rule that “no baby under 750g will have a trial of extubation as they will most certainly fail”. As time went on however, studies suggested that not only is this a false statement but also that the duration of intubation was directly correlated with risk of BPD. As Danan described, for infants less than a 1000g, delaying extubation when they had reached minimal settings did not result in lower rates of BPD. Moreover 60 – 70% of infants who have such extubation attempts are not reintubated within a week, so it is possible to have success.
The detractors however express concern about the 30-40% who do require reintubation and worry that harm will be caused by such acts. Frequent concerns are voiced with respect to potential trauma to the airway leading to subglottic stenosis; potentially increasing the risk of BPD and finally the belief that attempts are futile so why put parents through the stress in the midst of perceived near certain failure. The problem with these perceptions however is that they are mostly the culmination of confirmation bias. Patients that have multiple failed extubations are remembered especially when they develop significant complications, while the ones who extubate successfully are quickly forgotten. This is not intentional in any way but simply a human tendency to follow the pattern of “the squeaky wheel getting the grease”. The preemies who do poorly are front and centre as they take up a great deal of our time & attention while the ones who do very well while celebrated, are not as easily remembered for the success they demonstrated when extubated.
Being someone who believes in extubating as soon as possible though I was surprised several months ago to find a paucity of data demonstrating that there was in fact support for the practice in terms of better outcomes being associated with early extubation. While small studies certainly pointed in that direction the real question was about to be answered in the study that follows.
Is it better to fail multiple times or be intubated once for the duration of ventilation.
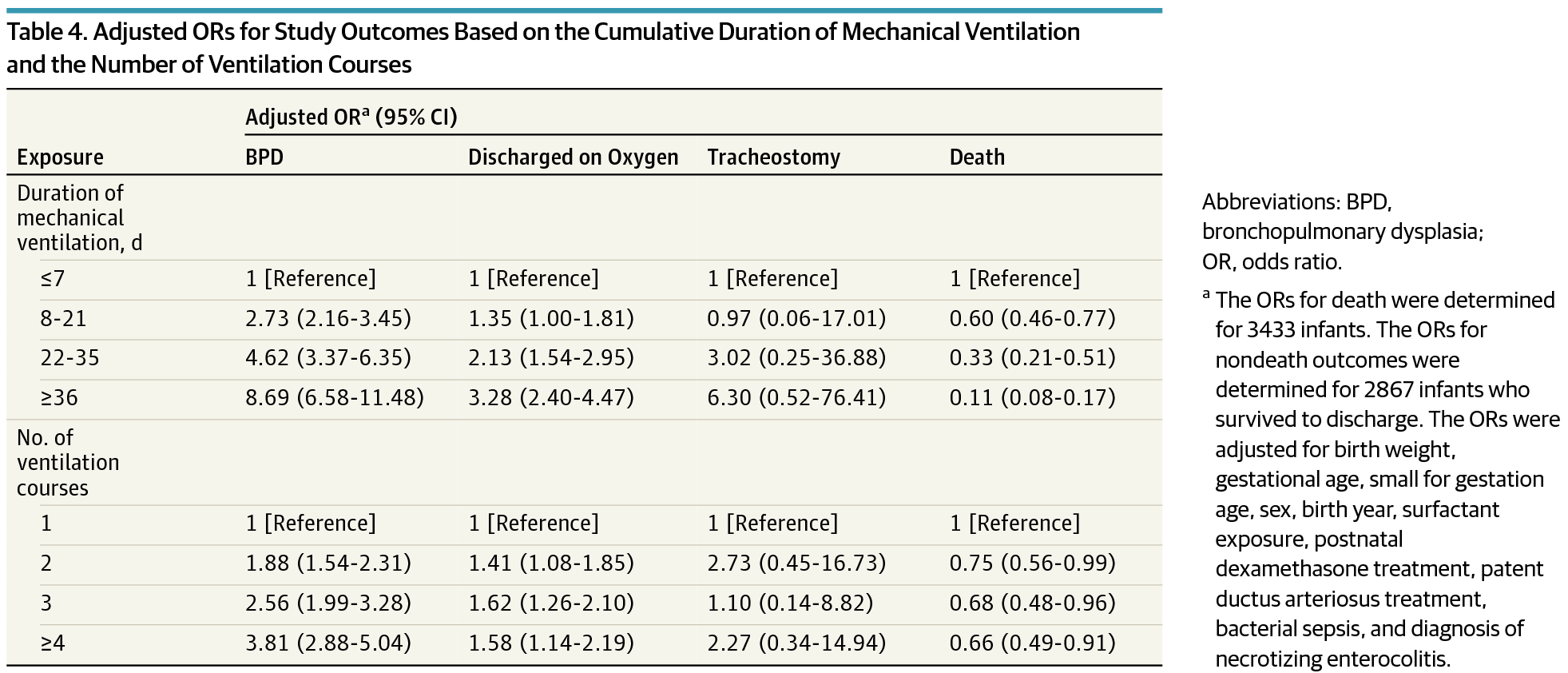
This is the central question that I believe has been answered as good as it will ever be by EA Jensen et al in JAMA this past month “Effects of Multiple Ventilation Courses and Duration of Mechanical Ventilation on Respiratory Outcomes in Extremely Low-Birth-Weight Infants.” This retrospective review included 3343 infants below 1000g and examined the primary outcome of BPD and secondary outcomes of death, continued supplemental oxygen use at the time of discharge, and tracheostomy among survivors. As you might expect, regardless of whether one compared duration of ventilation or number of reintubations, variables such as need for surfactant, postnatal dexamethasone, PDA treatment and NEC became more common as exposure to either outcome increased. 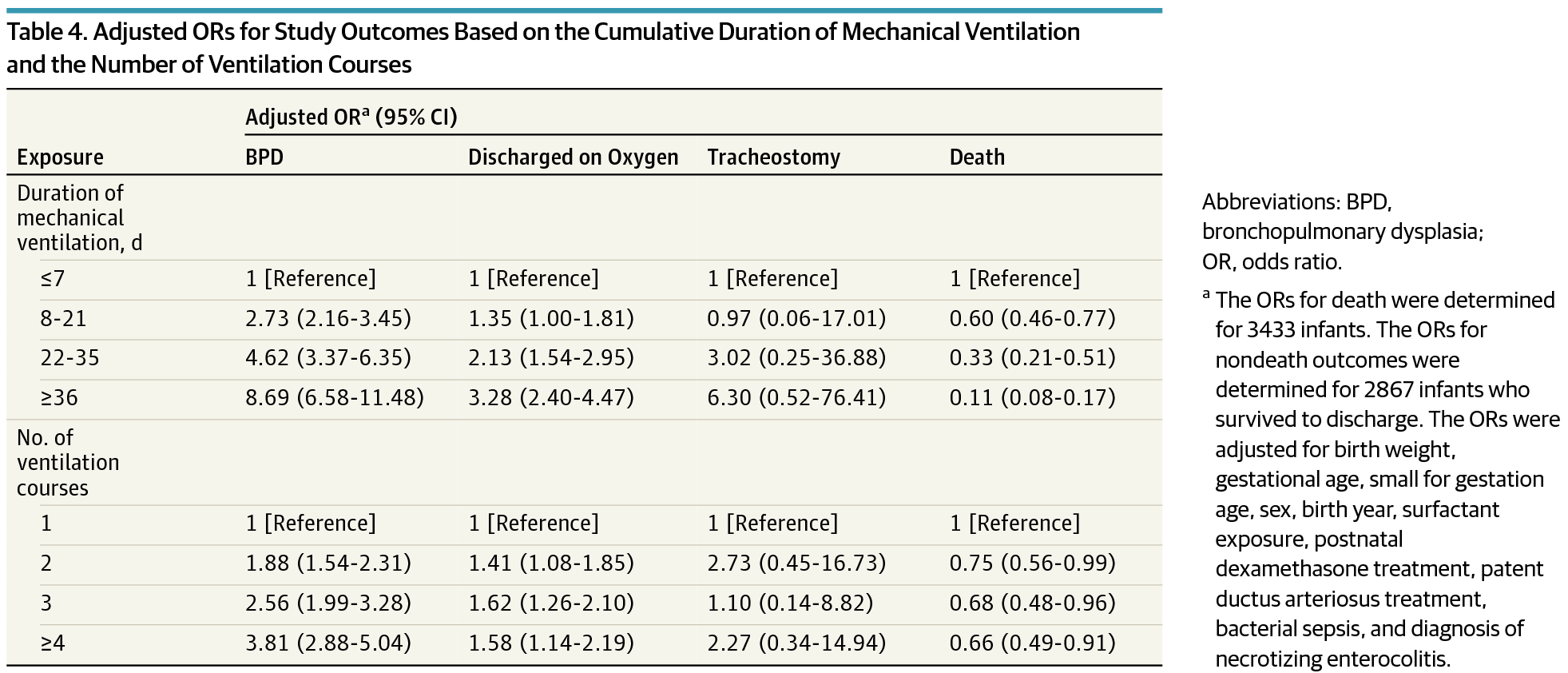 When a logistic regression model was applied though it became evident that the odds ratio for BPD increased to a much greater degree with increasing duration of ventilation than the number of attempts.
When a logistic regression model was applied though it became evident that the odds ratio for BPD increased to a much greater degree with increasing duration of ventilation than the number of attempts.
To quote the authors:
“After adjustment for the cumulative duration of mechanical ventilation, a greater number of ventilation courses was not associated with an increase in the risk-adjusted odds of supplemental oxygen use at discharge. The number of ventilation courses remained associated with increased risk of BPD only among infants exposed to 4 or more courses.”
The Needs of The Many Outweigh The Needs of The Few
In other words, for an infant to have an increased risk of BPD they would need to have failed extubation four or more times! It is not easy to predict with certainty who these children will be but if we take these findings as accurate (since I believe we will not see an RCT of this magnitude anytime soon) is it ethical to keep a child intubated due to the belief that they might fail? On the contrary, how can we not try when failure is not associated with adverse outcome? In fact none of the secondary outcomes were found to be increased either. Importantly, there was no difference in the need for a tracheostomy in this population which may serve as a proxy for lack significant airway injury from multiple intubations. The goal of this post is to provide all of us who care for these preemies with the reassurance that if they fail extubation, once, twice and even three times that is still a good thing. For the ones that fail more than that, if only we had a crystal ball we might have spared them that risk but given that we live in a world without this ability, we owe it to our patients to try. Moreover, we owe it to the parents of these children to educate them that failure can still be a good thing.
May I never have a near 100% success at extubating my patients on the first try. If I truly care for them I will embrace my failures and know that I have done the right thing.

by All Things Neonatal | Nov 7, 2015 | Neonatology
Something kind of big happened today. I received a notice on my Facebook Page that there were now 3000 “likes” for this little community that I started back in February of this year.  I was asked early on what the purpose of this blog and Facebook page were and in response I wrote the piece Inside the mind of a Neonatal Blogger. Why am I doing this?. If you are curious, this gives you a good glimpse into my motivations.
I was asked early on what the purpose of this blog and Facebook page were and in response I wrote the piece Inside the mind of a Neonatal Blogger. Why am I doing this?. If you are curious, this gives you a good glimpse into my motivations.
Truth be told though I wasn’t really sure what this would become and early on my goal was to have 300 likes and then when that was passed 1000. What has happened since has been quite the surprise. I could not have imagined the growth in the page and the blog since that time.
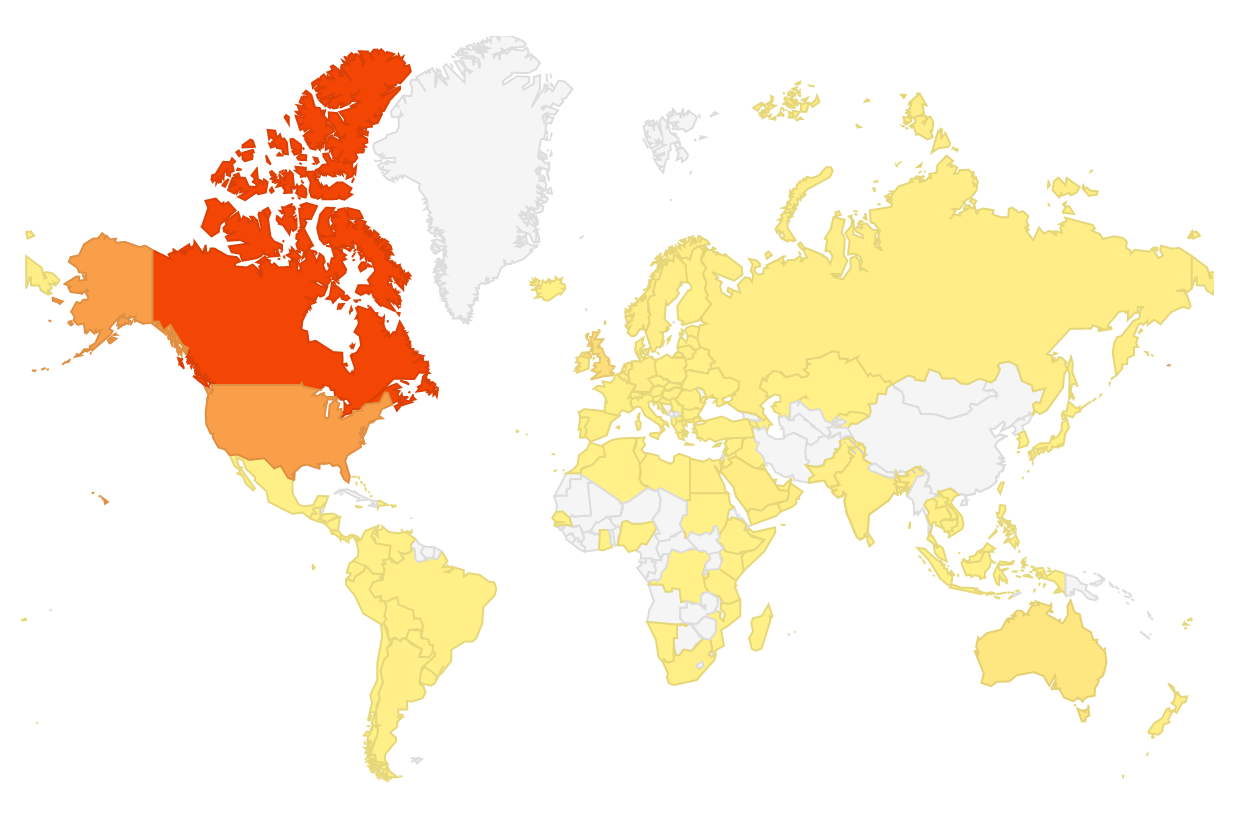
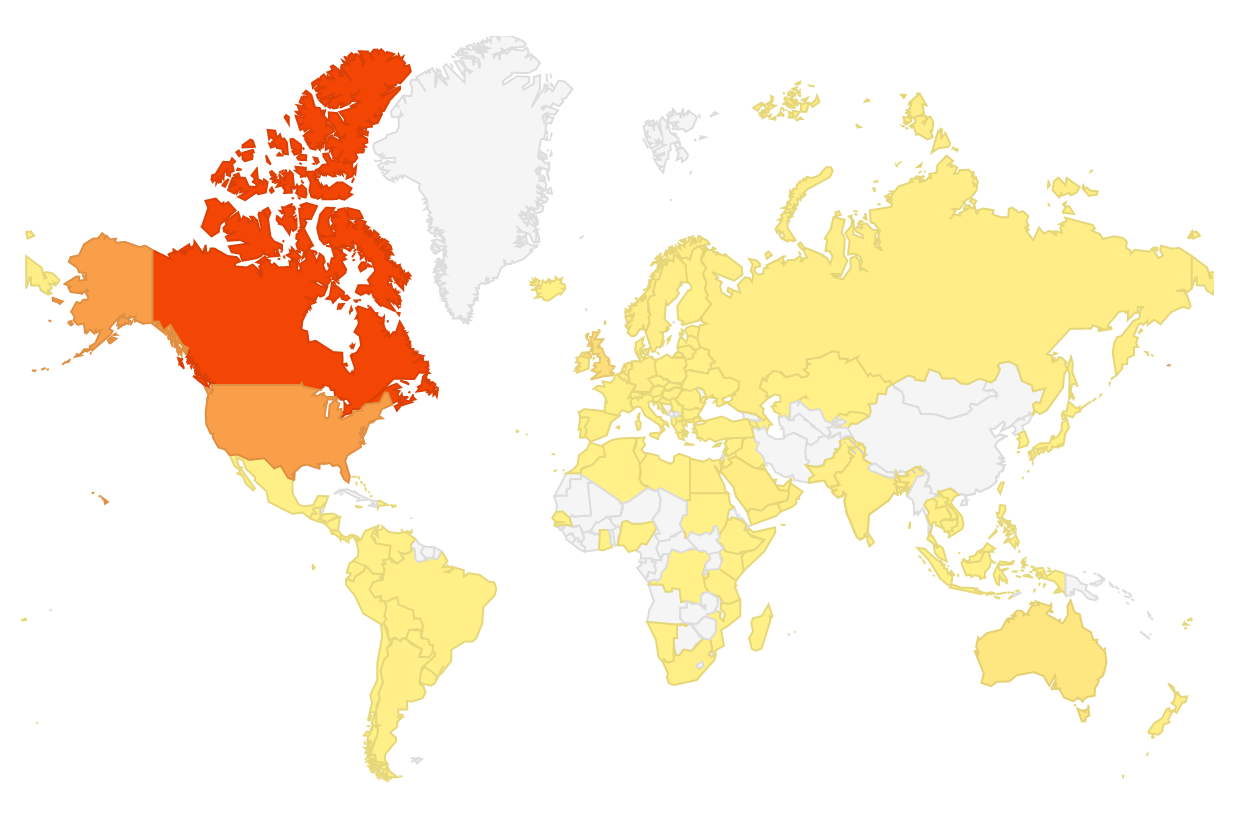
The map above actually represents all the countries that have read posts from this blog. The red colour aside from being Canada indicates the top country in terms of views, the USA is second in orange and then yellow being the rest of the countries on the map. The white areas are as of yet countries that have not read a piece but who knows what will happen given a little more time!
An interesting shift though has occurred on the Facebook page and that is over the last month a real community has evolved. Up until recently a given post might generate one or two comments but I have noticed something quite special evolving on this site. That is that not only have the comments increased with each post but you the readers are beginning to use this site as I had envisioned. Comments are being made and you are responding rather than leaving it all up to me. Don’t take this the wrong way though, I am more than happy to respond but I am enjoying reading your own thoughts as well. We come from such a wide variety of backgrounds and experiences and these differences are beginning to express themselves in your written words.
As much as I enjoy finding interesting Neonatal content to share with you, I equally enjoy seeing how you respond. An additional complement is that the interactions are almost always respectful, productive and generating of even more dialogue. I learn from you just as you learn from me so let me say thank you for that!
Lastly, I have come to understand that “All Things Neonatal” really does have to be just that. Try as I might I have not been able to unlock the secret of what truly interests the reader. Topics that I would have predicted would “go viral” have been put out into the internet only to produce a sound “thud” as they fall flat which others that I might have thought would generate mild interest have exploded. It is this unpredictability that keeps me excited about putting out each post as I continue to be fascinated by my inability to predict what leads to a boom or a bust.
In case you are wondering though the top three posts have been:
- Winnipeg hospital now resuscitating all infants at 22 weeks! A media led case of broken telephone.
- Automatic adjustments of FiO2. Ready for prime time?
- Marijuana Coming Soon To An NICU Near You!
If you haven’t read these then you may be missing out as your fellow readers seemed to think these were a big hit.
Thanks to each of you for following and keep the comments coming. Also if you try something out that you see on this site and adopt it in your hospital please let me know how it has gone. We can all learn plenty from each other. As our base grows so does our collective knowledge and in my opinion that is a good thing.

by All Things Neonatal | Nov 5, 2015 | feeding, marijuana
October 17th, 2018 the personal use of marijuana became legal in Canada. With this change in status I felt it was appropriate to consider a couple things. First it would address an issue that affects almost all preterm infants and secondly finally acknowledge that with legalization of marijuana, the door has opened to acceptance perhaps of further medicinal uses for cannabinoids. Who knows where things will go from here…
Marijuana and babies have for the most part had a unfriendly past. Marijuana’s effect on the growing fetus has been a concern in past publications and women for years have been screened for it’s use along with other more illicit drugs. More recently a large study by Warshack found increased rates of NICU admission and infants who were SGA among users but did not reveal any other significant adverse outcomes with use. Those who have identified themselves as users have been subjected to being labelled as addicts & stoners among other names but with Canada on the verge of becoming a marijuana friendly country this is likely to change. Interestingly, caffeine, a drug that we are all familiar with though, has a similar story in that excessive quantities have been deemed harmful in pregnancy yet it is one of the most commonly used medications in the NICU due to its beneficial effects on apnea of prematurity.
It’s Only Natural
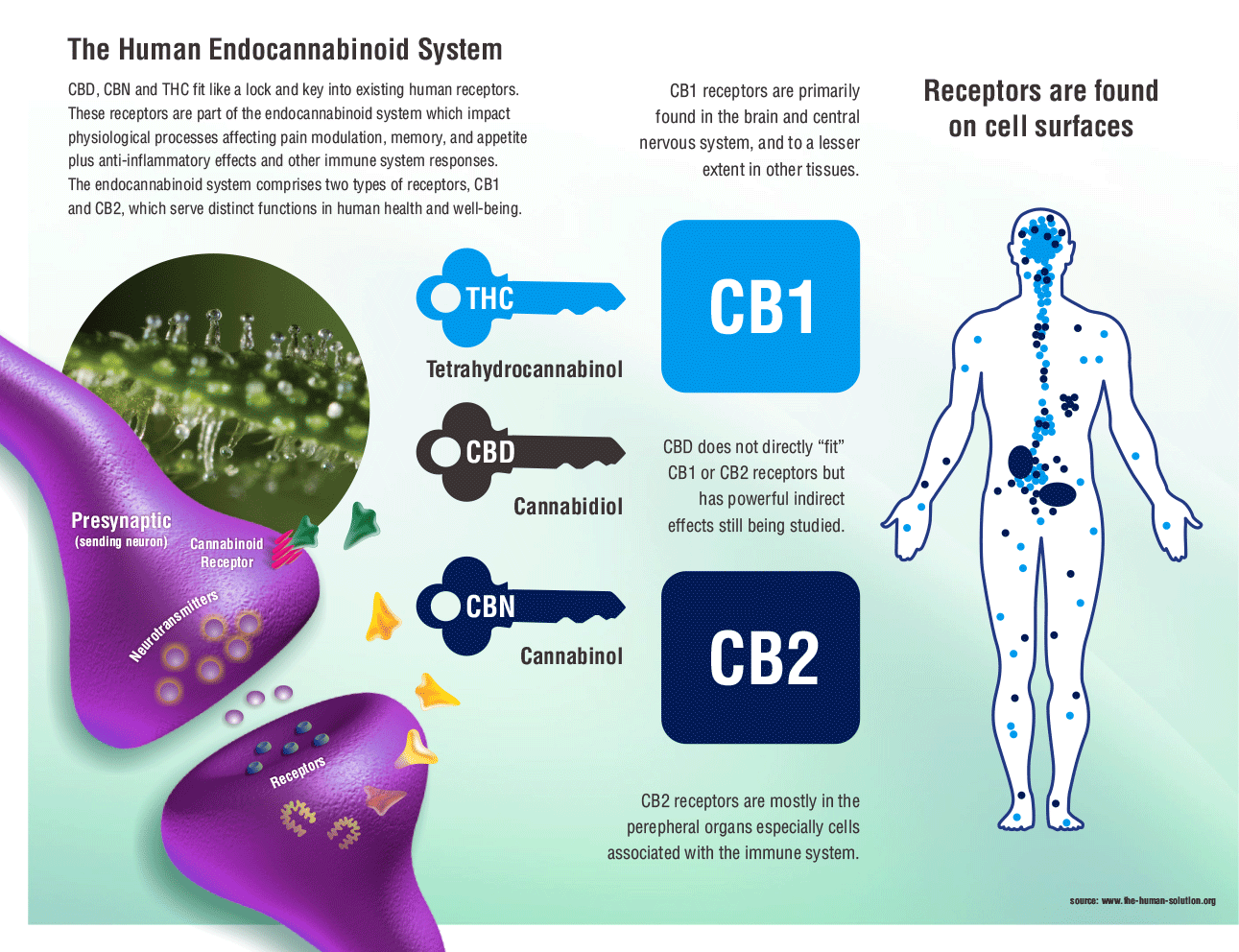
Now before people think I have come completely off the rails, I am not envisioning a future world of hazy smoke filled isolettes or NICUs for that matter. It is not the burning plant that may work its way into the NICU but rather the active class of drug; cannabinoids. 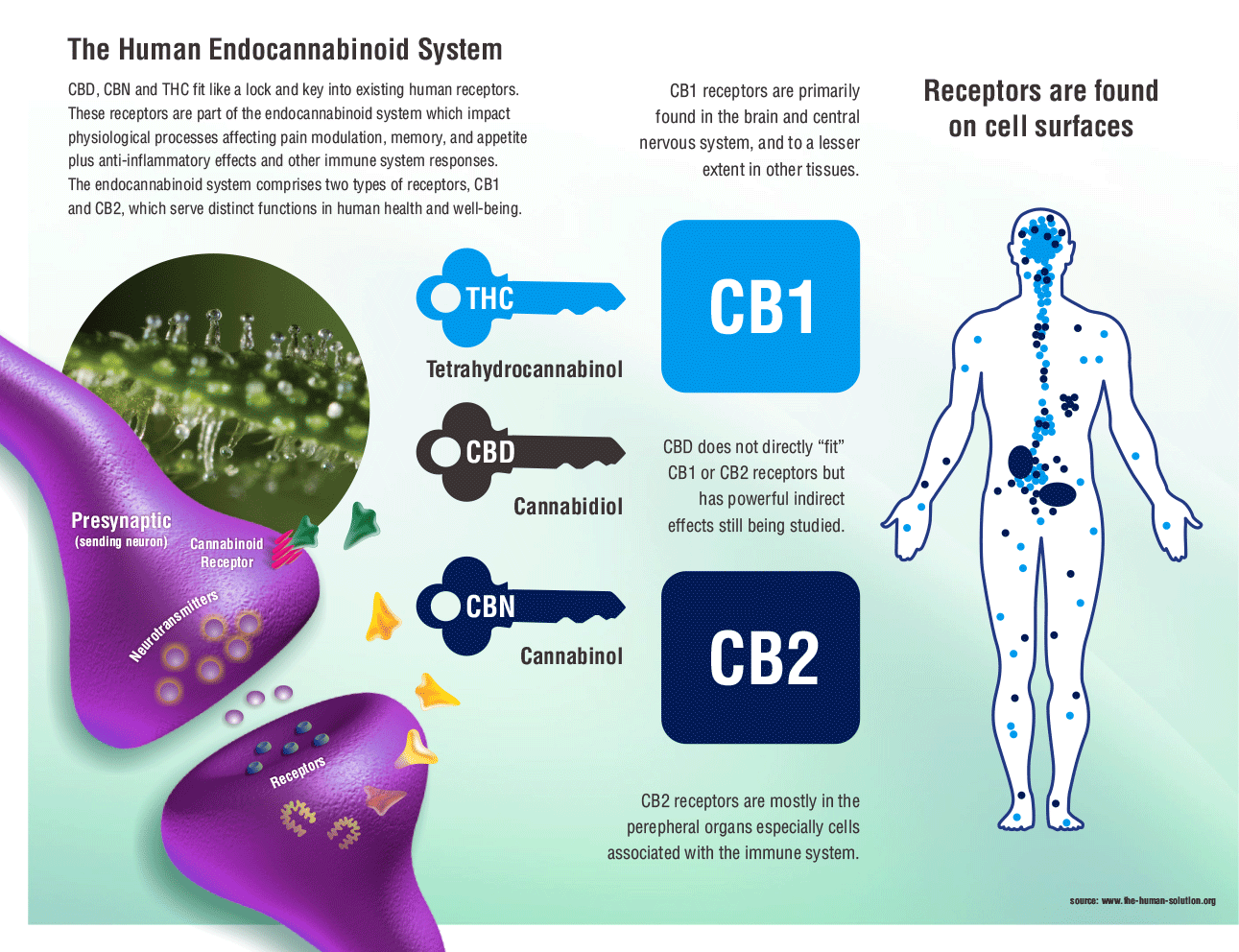 It turns out that we humans have actually been built to receive such molecules as evidenced by the presence of cannabinoid receptors in our tissues and in particular our brains. The presence of these substances is even important in birth. Jokisch et al compared cord blood levels of endocanabinoids between those infants delivered vaginally and those by c-section without labour. The infants born by vaginal birth had significantly higher levels of these substances in their blood demonstrating that they have a role to play in the transition to extrauterine life. These endogenously produced versions are called endocannabinoids. Furthermore breast milk contains such endocannabinoids which raises the questions of what these substances are doing there.
It turns out that we humans have actually been built to receive such molecules as evidenced by the presence of cannabinoid receptors in our tissues and in particular our brains. The presence of these substances is even important in birth. Jokisch et al compared cord blood levels of endocanabinoids between those infants delivered vaginally and those by c-section without labour. The infants born by vaginal birth had significantly higher levels of these substances in their blood demonstrating that they have a role to play in the transition to extrauterine life. These endogenously produced versions are called endocannabinoids. Furthermore breast milk contains such endocannabinoids which raises the questions of what these substances are doing there.
To answer this question an elegant study was performed in mice in which the CB1 receptor antagonist rimonabant was injected at different time points to block the effect of endocannabinoids. When given in the first 24 hours, “milk ingestion and subsequent growth was completely inhibited in most pups (75%–100%) and death followed within days after antagonist administration.” When examining the reason for poor milk ingestion it was an inability to suck that was the cause, rather than loss of appetite. Although speculative, I cannot help but wonder if the infant of a diabetic mother who demonstrates poor coordination of suck might well have altered expression of cannabinoid receptors or antagonism of the same.
What Benefits Could We See From Medicinal Use?
When it comes to life in the modern NICU it is the large number of patients in need of gavage feeding that keep our census numbers high. Whether they be the infants of diabetic mothers or survivors of extreme prematurity, many remain in hospital soley for poor feeding. We can treat their apnea with caffeine but for years I have questioned whether an appetite stimulant might offer hope to transition such children to the home. We are not in a position to start using cannabinoids in clinical practice yet as w have not had any trials that I am aware of outside of an animal model but I would suggest to you that this may be the next frontier.
For those that use marijuana or one of it’s other forms they will tell you there are many potential benefits and the same could be true for newborns. There is no question that THC can be sedating and calming so could there be a role as an alternative to narcotics and benzodiazepines? Additionally, animal models of hypoxic ischemic encephalopathy are revealing a protective effect of cannabinoids both in the short and long term. Much like erythropoietin and melatonin have emerged as adjunctive treatments to cooling, based on animal studies we may find cannabinoids trialed in human studies before long.
What Does The Future Hold In Store For Us
I have certainly talked about this on rounds before but have not had the confidence that such studies would pass through a local ethics board.  Now the winds have changed with the election of Mr. Trudeau Prime Minister and the perception of marijuana? As we become more comfortable with the benefits of cannabinoids I suspect we will see these substances come into play much like caffeine did oh so many years before. There is no question that when people say that marijuana is “natural’ they are right in a sense. The building blocks of THC are produced in our bodies and we have receptors anxiously awaiting stimulation by these substances. The time for medicinal use in the NICU will come sooner or later. Sound a little crazy?
Now the winds have changed with the election of Mr. Trudeau Prime Minister and the perception of marijuana? As we become more comfortable with the benefits of cannabinoids I suspect we will see these substances come into play much like caffeine did oh so many years before. There is no question that when people say that marijuana is “natural’ they are right in a sense. The building blocks of THC are produced in our bodies and we have receptors anxiously awaiting stimulation by these substances. The time for medicinal use in the NICU will come sooner or later. Sound a little crazy?
Trials have already begun based on research in animals in the field of HIE as discussed in this article.
Let’s look back at this post in 5-10 years.

 Survival at these GA in the recent NEJM study of almost 5000 preterm infants under 27 weeks were 33 and 57 % respectively at 23 & 24 weeks with rates of survival without moderate or severe disability being 16 and 31% in the two groups. The fallout from this and other studies at the extremes of gestational age have been that we should be more aggressive as the outcomes are not as bad as one would predict. How can we argue this for the 23-24 week infants and for term infant with the same likelihood of outcomes we would unilaterally stop in many centres?!
Survival at these GA in the recent NEJM study of almost 5000 preterm infants under 27 weeks were 33 and 57 % respectively at 23 & 24 weeks with rates of survival without moderate or severe disability being 16 and 31% in the two groups. The fallout from this and other studies at the extremes of gestational age have been that we should be more aggressive as the outcomes are not as bad as one would predict. How can we argue this for the 23-24 week infants and for term infant with the same likelihood of outcomes we would unilaterally stop in many centres?!

 In April of 2015
In April of 2015  This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.
This represents about a 5% increase in patient bed days per year. Five percent may not seem like a large increase at first blush but when we like many hospitals have been trying to deal with staffing issues and many days in which we are at or near capacity, this is not an insignificant challenge. It is a challenge though that we must face head on. Resources must be found, and space provided to accommodate for these children. We live in a world now where it is not solely up to us but to the family as well who must be integral to any such decision to either pursue or withdraw care. News of such infants surviving has spread to the public and I have no doubt that many families will have heard stories of such survivors. The next phase of care for these infants must address the shortcomings in care at the moment.